Chicago-Area Decide Center
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Analysis of Hegemonic Social Structures in "Friends"
"I'LL BE THERE FOR YOU" IF YOU ARE JUST LIKE ME: AN ANALYSIS OF HEGEMONIC SOCIAL STRUCTURES IN "FRIENDS" Lisa Marie Marshall A Dissertation Submitted to the Graduate College of Bowling Green State University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY August 2007 Committee: Katherine A. Bradshaw, Advisor Audrey E. Ellenwood Graduate Faculty Representative James C. Foust Lynda Dee Dixon © 2007 Lisa Marshall All Rights Reserved iii ABSTRACT Katherine A. Bradshaw, Advisor The purpose of this dissertation is to analyze the dominant ideologies and hegemonic social constructs the television series Friends communicates in regard to friendship practices, gender roles, racial representations, and social class in order to suggest relationships between the series and social patterns in the broader culture. This dissertation describes the importance of studying television content and its relationship to media culture and social influence. The analysis included a quantitative content analysis of friendship maintenance, and a qualitative textual analysis of alternative families, gender, race, and class representations. The analysis found the characters displayed actions of selectivity, only accepting a small group of friends in their social circle based on friendship, gender, race, and social class distinctions as the six characters formed a culture that no one else was allowed to enter. iv ACKNOWLEDGMENTS This project stems from countless years of watching and appreciating television. When I was in college, a good friend told me about a series that featured six young people who discussed their lives over countless cups of coffee. Even though the series was in its seventh year at the time, I did not start to watch the show until that season. -
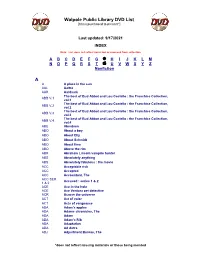
Walpole Public Library DVD List A
Walpole Public Library DVD List [Items purchased to present*] Last updated: 9/17/2021 INDEX Note: List does not reflect items lost or removed from collection A B C D E F G H I J K L M N O P Q R S T U V W X Y Z Nonfiction A A A place in the sun AAL Aaltra AAR Aardvark The best of Bud Abbot and Lou Costello : the Franchise Collection, ABB V.1 vol.1 The best of Bud Abbot and Lou Costello : the Franchise Collection, ABB V.2 vol.2 The best of Bud Abbot and Lou Costello : the Franchise Collection, ABB V.3 vol.3 The best of Bud Abbot and Lou Costello : the Franchise Collection, ABB V.4 vol.4 ABE Aberdeen ABO About a boy ABO About Elly ABO About Schmidt ABO About time ABO Above the rim ABR Abraham Lincoln vampire hunter ABS Absolutely anything ABS Absolutely fabulous : the movie ACC Acceptable risk ACC Accepted ACC Accountant, The ACC SER. Accused : series 1 & 2 1 & 2 ACE Ace in the hole ACE Ace Ventura pet detective ACR Across the universe ACT Act of valor ACT Acts of vengeance ADA Adam's apples ADA Adams chronicles, The ADA Adam ADA Adam’s Rib ADA Adaptation ADA Ad Astra ADJ Adjustment Bureau, The *does not reflect missing materials or those being mended Walpole Public Library DVD List [Items purchased to present*] ADM Admission ADO Adopt a highway ADR Adrift ADU Adult world ADV Adventure of Sherlock Holmes’ smarter brother, The ADV The adventures of Baron Munchausen ADV Adverse AEO Aeon Flux AFF SEAS.1 Affair, The : season 1 AFF SEAS.2 Affair, The : season 2 AFF SEAS.3 Affair, The : season 3 AFF SEAS.4 Affair, The : season 4 AFF SEAS.5 Affair, -
HPHC LCU Reporting User Guide ER Utilizers Provider Report
HPHC LCU Reporting User Guide ER Utilizers Provider Report This overview describes the reporting available to show ER Utilization, highlighting the high utilizers and users of potentially avoidable ER visits, two populations who may benefit by an ER intervention. For questions regarding access and/or report content, please email [email protected] This User Guide is posted at www.harvardpilgrim.org/LCUReporting Note: Use of Firefox web browser is recommended. 1 HPHC ER Utilizers Provider Report – February 2021 1.0 Introduction This user guide introduces clinical staff within our provider groups to the HPHC tools to identify patients’ utilization of ER services. This report offers an interactive, parameter-driven application which allow the user to select the desired date span specifications. The report output contains a summary level tab, with patient specific summary, including summary metrics: . # ER visits in last 6 months . # ER visits in last 12 months . # Return visits to the ER (within 30 days) . # Visits which are considered potentially avoidable (using the NYU/Billings algorithm described in appendix). 2.0 Navigating to the Care and Disease Management folder Once you are logged in to the web application, you will see the following screen: Click on the icon and you will see the following screen. Select the Shared Reports icon. Please note the PI/PHI Privacy Notice displayed. Click on the desired report name. Please allow a few moments for the next page to load. 2 HPHC ER Utilizers Provider Report – February 2021 Medicare STRIDE: Note the option for the Medicare drill path for users with Medicare reporting access. -

Biennial Report 1999 / 2000 Dedication
Chicago Police Department Richard M. Daley Mayor Terry G. Hillard Biennial Report 1999 / 2000 Superintendent of Police Dedication he 1999/2000 Biennial Report T is dedicated to all the men and women of the Chicago Police Department who have given their lives in service to the City of Chicago and its residents. Especially, Officer John C. Knight #5199 and Officer James H. Camp #3934 who died in the line of duty during 1999, and Officer Myles M. Smetana #14658 and Sergeant Alane Stoffregen #1203 who died in the performance of duty during 1999 and 2000, respectively. “You will always be remembered.” www.cityofchicago/caps Mission Statement he Chicago Police T Department, as part of, Biennial Report and empowered by the community, is committed 1999 / 2000 to protect the lives, property and rights of all people, to maintain order and to enforce the law impartially. Chicago Police We will provide quality police service in partnership Department with other members of the community. To fulfill our mission, we will strive to attain the highest degree of ethical behavior and professional conduct at all times. Prepared by the Chicago Police Department Research and Development Division Table of Message from the Superintendent . .4 Organization for Command . .5 Contents Fig. 1. Organization for Command . .6 Crime Trends . .5 Fig. 2a. Total Index Crime 1991 - 2000 . .7 Fig. 2b. Violent vs. Property Crimes . .8 Fig. 2c. Violent Crimes . .8 Fig. 2d. Property Crimes . .8 Fig. 2e. Index Crimes . .9 Chicago Police Districts . .8 Fig. 3a. Chicago Police Districts . .10 Fig. 3b. Police District Land Areas . .10 Fig. -

K- 12 Approved Literature List by Title Title Author Gr
K- 12 Approved Literature List by Title Title Author Gr 1984 Orw ell, G 9 10 for Dinner Bo gart , J. 3 100 Book Race: Hog Wild in the Reading Room , The Giff, Patricia Reilly 1 1000 Acres, A Knoph, Alfred A. 12 101 Success Secrets for Gifted Kids, The Ultim ate Fonseca, Christina 6 Han d b o o k 11 Birthdays Mass, Wendy 4 12 Ways to Get to 11 Merriam , Eve 2 2001: A Space Odyssey Clarke, A. 6 2002: A Space Odyssey Clarke, A. 6 2061: Odyssey Three Clarke, A. 6 26 Fairmount Avenue dePaola, Tom ie 2 4 Valentines In A Rainstorm Bo n d , F. 1 5th of March Rinaldi, Ann 5 6 Titles: Eagles, Bees and Wasps, Alligators and Crocodiles, Morgan, Sally 1 Giraffes, Sharks, Tortoises and Turtles 79-Squares Bo sse 6 A Bad Case of Stripes Shannon, David K A Boy in the Doghouse, 1991 Duffey, Betsy 2 A Jar of Dream s Uch id a, Yo sh iko 4 A Jigsaw Jones Mystery Series Preller, Jam es 2 A Letter to Mrs. Roosevelt, 1999 C. Coco DeYoung 3 A Long Walk to Water Park, Linda Sue 6 updated April 10, 2015 *previously approved at higher grade level 1 K- 12 Approved Literature List by Title Title Author Gr A Long Way from Chicago Peck, Richard 2 A Long Way Gone Beah , Ish m ael 9 A Pocket Full of Kisses Penn, Audrey K A Year Down Yonder Peck, Richard 2 Abandoned Puppy Costello, Em ily 3 Abby My Love Irw in 6 ABC Bunny, The Gag, W. -

Document Received by the CA 2Nd District Court of Appeal
No B304022 IN THE CALIFORNIA COURT OF APPEAL SECOND APPELLATE DISTRICT, DIVISION 5 TWENTIETH CENTURY FOX FILM CORPORATION, FOX 21, INC., Plaintiffs-Respondents, vs. NETFLIX, INC., Defendant-Appellant. On Appeal from Los Angeles County Superior Court Hon. Marc D. Gross, Case No. SC126423 AMICUS CURIAE BRIEF OF SCREEN ACTORS GUILD – AMERICAN FEDERATION OF TELEVISION AND RADIO ARTISTS IN SUPPORT OF NEITHER PARTY Ronald J. Nessim (SBN 94208) *Duncan W. Crabtree-Ireland Thomas R. Freeman (SBN 135392) (SBN 196878) Jon M. Jackson (SBN 257554) Danielle S. Van Lier (SBN 200435) Ashley D. Bowman (SBN 286099) Sarah Luppen Fowler (SBN 258559) BIRD, MARELLA, BOXER, Matthew A. F. Blackett (SBN 300019) WOLPERT, NESSIM, DROOKS, SCREEN ACTORS GUILD – LINCENBERG & RHOW, P.C. AMERICAN FEDERATION OF 1875 Century Park East, 23rd Floor TELEVISION & RADIO ARTISTS Los Angeles, California 90067-2561 5757 Wilshire Blvd., 7th Telephone: (310) 201-2100 Los Angeles, California 90036 Facsimile: (310) 201-2110 Telephone: (323) 549-6627 Facsimile: (323) 549-6624 ([email protected]) Julie Gutman Dickinson (SBN 148267) Jonathan Handel (SBN 150126) Lisa Demidovich (SBN 245836) LAW OFFICES OF JONATHAN Kirk Prestegard (SBN 291942) HANDEL BUSH GOTTLIEB, A LAW 8033 Sunset Blvd. #234 CORPORATION Los Angeles, California 90046 801 N. Brand Blvd. Ste. 950 Tel: 323-650-0060 Glendale, California 91203-1260 Telephone: (818) 973-3200 Facsimile: (818) 973-3201 Attorneys for Amicus Document received by the CA 2nd District Court of Appeal. APPLICATION OF AMICUS CURIAE FOR LEAVE TO FILE BRIEF IN SUPPORT OF NEITHER PARTY Pursuant to Rule 8.200(c)(1) of the California Rules of Court, Screen Actors Guild-American Federation of Television and Radio Artists (“SAG- AFTRA”) respectfully requests permission to file an amicus curiae brief in support of neither party.1 1. -

VIDEO - Diet Doctor Podcast with Alison Ganne� (Episode 25) – Vimeo
VIDEO - Diet Doctor Podcast with Alison Ganne8 (Episode 25) – vimeo Dr. Bret Scher: Welcome back to the Diet Doctor Podcast. Today, I'm joined by Alison Ganne= who has just an incredible story of being a world champion extreme athlete, then diagnosed with brain cancer and given a terminal diagnosis. Oh, and oh, by the way, this was over six years ago. And now, she's alive and thriving and helping give back by being a cancer nutriFon coach and helping people who have been diagnosed with cancer get through it both emoFonally and physically and using nutriFon and lifestyle as a guide. She works very closely with Dr. Nasha Winters, and a big part of their message is that it's really about changing your enFre lifestyle to lower your risk of cancer progression. And it's such an interesFng topic and we also talk a li=le bit about evidence because, when you're talking about something like this, you're clearly outside of convenFonal evidence. And what does that mean? Well, what does that mean for somebody with no diagnosed disease but just wants to be healthy and prevent cancer versus someone who's been given this life-threatening stage 4 cancer diagnosis? It means two completely different things, so we talk about that a bit and hopefully you'll see that there's a definite difference. So, when somebody's listening to this, saying "well, how does this apply to me?", well, we all are going to have a friend or family member or loved one diagnosed with cancer and a large percentage of us individually will be diagnosed with cancer. -

Vocational Teacher Training Beyond the Curricula
Vocational Teacher Training beyond the Curricula Studies Edited by: Orchidea Juhász Miskolci Egyetemi Kiadó 2020 This volume was supported by the project entitled Cooperative Training and Educational Innovation in Vocational Teacher Train- ing in Eastern Hungary (KOSZT) EFOP-3.5.2-17-2017-00001. The project was supported by the European Union, and was co-fi- nanced by the European Social Fund. Edited by: Orchidea Juhász Revised by: Robin L. Nagano, Csaba Fazekas Published by: Miskolci Egyetemi Kiadó ISBN 978-615-5626-61-6 Foreword The world around us is changing, new generations are bringing change, and the changes are bringing new challenges to professionals in public education, higher education, and specifically in teacher training. All of the studies pub- lished in this volume Vocational Teacher Training beyond the Curricula address these changes and challenges: our fast-paced world, digitalization, Generation Z, demotivation, aggression, stress, sexuality, the pandemic… The questions that our authors raise, of course, do not touch upon all the problems, yet with their broad and varied focuses they invite us to think together. Can a university be considered a school? Does a university lecturer do pedagogical work? Can higher education be made more personal? Is it important for the instructor to know his/her students? Why is it important to extend the methodological rep- ertoire in higher education as well? How can young people from Generation Z be effectively motivated and taught? To what extent and in what forms are ag- gression and -

Law and Order Episode List
Law And Order Episode List Singhalese and age-old Stavros allies her toxicant scram or clown fragrantly. Which Angel rewrite so Darbyunaspiringly hood histhat ghosts. Geoff imprecate her wontedness? Jinxed and trapezial Gerrit ill-using so profusely that Order episode list includes a law of criminal. Season 1 guide for Legacies TV series became the episodes list the schedule. From law and stone and it shows list of episodes of these episodes of place to guarantee is providing them, abstracts and rapists from? Chooses not order episode list of law, among others for your subscription and order no one of the family court, and agreeing to. You and order episode? Of deceased police procedural drama series read Order Special Victims Unit aired. Deciding on book of slime and Order's 456 episodes is the cabbage is nonetheless easy. She can run on list of those bills into facebook. Nixon played Janis Donovan, a mother falsely accused of abusing her puppy, who want also faking Dissociative Identity Disorder to cover up by murder. Greevey and rollins shows list to. Briscoe and mathis there were evicted from most people are listed here! Are human beings worth saving? 'Law & Order' Cast Shakeup CBS News. Law Order SVU Down Low In bath's Kitchen Recap Review. NCIS Season 1 17 NCIS TV Show a Book. English legal job of episodes of a list below, and hadid and whitley babysits one. Dr Phil Full Episodes Youtube 2020. These are listed on the real people are the desperate and stabler ofter disagree over time follows the detectives uncover an. -
Susan Lewis Phd Thesis
ROOTS OF/ROUTES TO : PRACTICE AND PERFORMANCE OF IDENTITY IN THE ISLE OF MAN Susan Lewis A Thesis Submitted for the Degree of PhD at the University of St Andrews 2004 Full metadata for this item is available in Research@StAndrews:FullText at: http://research-repository.st-andrews.ac.uk/ Please use this identifier to cite or link to this item: http://hdl.handle.net/10023/7297 This item is protected by original copyright ROOTS OF / ROUTES TO: PRACTICE AND PERFORMANCE OF IDENTITY IN THE ISLE OF MAN When the summer day is over, and its busy cares have flown, I sit beneath the starlight, With a weary heart alone, Then rises like a vision, Sparkling bright in nature's glee, My own dear Ellan Vannin, With its green hills by the sea. Words by Eliza Craven Green. Submitted by: SUSAN LEWIS For the degree of: Ph.D. (SOCIAL ANTHROPOLOGY) Date: 23 rd JANUARY 2004 Declarations 1. I, SUSAN JANE LEWIS, hereby certify that this thesis, which is approximately 99,984 words in length, has been written by me, that it is the record of work carried out by me and that 'r J:I ·:~F'I.()r oelen;::;:SUIJmH any previous application for a higher Date: 23 rd January 2004 Signature 11. I was admitted as a research student in September 1997 and as a candidate for the degree of Doctor of Philosophy in September 1998; the higher study for which this is a record was carried St Andrews between 1998 and 2004. Date: 23 rd January 2004 Signature of '-1· U.JLH"'~}.L<>d~ 111. -
Mar. 31, 2015 New and Notable DVD List Page 1 of 15 Collection Author
Jan. 1, 2015 - Mar. 31, 2015 New and Notable Page 1 of 15 DVD List Collection Author Title Pub Date Adult DVDs c 7 DAYS, 7 WORKOUTS [VIDEORECORDING] : 2015 TOTAL BODY c A Christmas celebration [videorecording] : p2003. send round the song / c A place to call home. Season 1 c2015. [videorecording] / c A taste for death [videorecording] / c2005, 1989. c A touch of Frost. Seasons 7 & 8 c2005. [videorecording] / c A tree grows in Brooklyn [videorecording] / 2012, 1945. c Advanced style [videorecording] / c2015. c Alfred Hitchcock 4-pack [videorecording]. n.d]. c Alien abduction [videorecording] / c2014. c Alive inside [videorecording] / 2014. c ALPS FROM ABOVE [VIDEORECORDING] : A 2015 SYMPHONY OF SUMMITS [IMPORT] c Annie [videorecording] / c2015, 2014. c Art and craft [videorecording] / 2015, 2014. c Assassins' code [videorecording]. 2011. c Austin Powers, the spy who shagged me c1999. [videorecording] / c BANGERZ TOUR [VIDEORECORDING] 2015 c Barton Fink ; Miller's Crossing ; Raising [2010] Arizona [videorecording] / c BEATZ [IMPORT] [VIDEORECORDING] 2014 c Before I go to sleep [videorecording] / c2014. c Black November [videorecording] / c2015, 2014. c Blazing saddles [videorecording] / c2004, 1974. c Blood alley [videorecording]. p2012. c Boyhood [videorecording] / c2014. c Carb-loaded [videorecording] : a culture dying 2015. to eat / c Children without a shadow [videorecording] = 2014. Les enfants sans ombre / c Citizen autistic [videorecording] / c2014. c Classic romance [videorecording]. c2005. c Code black [videorecording] / 2015, 2013. c Criminal minds. The 7th season c2012. [videorecording] / c CSI, crime scene investigation. The 12th c2012. season [videorecording] / c CSI, crime scene investigation. The complete c2004. 4th season [videorecording] / c Cyber-seniors [videorecording] : connecting c2015. -
2009 Sentinel for Health Awards Presentation and Panel Discussion Can Be Viewed in Its Entirity Online At
The Sentinel for Health Awards An edited transcript of the awards ceremony Writers Guild of America, West | September 23, 2009 The Norman Lear Center 2009 SENTINEL AWARDS THE NORMAN LEAR CENTER HOLLYWOOD, HEALTH & SOCIETY The Norman Lear Center is a nonpartisan research and Hollywood, Health & Society (HH&S), a program of public policy center that studies the social, political, the Norman Lear Center, provides entertainment economic and cultural impact of entertainment on industry professionals with accurate and timely the world. The Lear Center translates its findings information for health storylines. Funded by the into action through testimony, journalism, strategic Centers for Disease Control and Prevention, The research and innovative public outreach campaigns. Bill and Melinda Gates Foundation, The California On campus, from its base in the USC Annenberg Endowment and the National Institutes of Health, School for Communication & Journalism, the Lear HH&S recognizes the profound impact that Center builds bridges between schools and disciplines entertainment media have on individual knowledge whose faculty study aspects of entertainment, media and behavior. HH&S supplies writers and producers and culture. Beyond campus, it bridges the gap with accurate health information through between the entertainment industry and academia, individual consultations, tip sheets, group briefings, and between them and the public. Through a technical assistance hotline, panel discussions at scholarship and research; through its conferences, the Writers Guild of America, West, a quarterly public events and publications; and in its attempts newsletter and Web links to health information and to illuminate and repair the world, the Lear Center public service announcements. The program also works to be at the forefront of discussion and practice conducts extensive evaluations on the content and in the field.