Benton County Community Health Assessment 2017-2021
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Analysis of Hegemonic Social Structures in "Friends"
"I'LL BE THERE FOR YOU" IF YOU ARE JUST LIKE ME: AN ANALYSIS OF HEGEMONIC SOCIAL STRUCTURES IN "FRIENDS" Lisa Marie Marshall A Dissertation Submitted to the Graduate College of Bowling Green State University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY August 2007 Committee: Katherine A. Bradshaw, Advisor Audrey E. Ellenwood Graduate Faculty Representative James C. Foust Lynda Dee Dixon © 2007 Lisa Marshall All Rights Reserved iii ABSTRACT Katherine A. Bradshaw, Advisor The purpose of this dissertation is to analyze the dominant ideologies and hegemonic social constructs the television series Friends communicates in regard to friendship practices, gender roles, racial representations, and social class in order to suggest relationships between the series and social patterns in the broader culture. This dissertation describes the importance of studying television content and its relationship to media culture and social influence. The analysis included a quantitative content analysis of friendship maintenance, and a qualitative textual analysis of alternative families, gender, race, and class representations. The analysis found the characters displayed actions of selectivity, only accepting a small group of friends in their social circle based on friendship, gender, race, and social class distinctions as the six characters formed a culture that no one else was allowed to enter. iv ACKNOWLEDGMENTS This project stems from countless years of watching and appreciating television. When I was in college, a good friend told me about a series that featured six young people who discussed their lives over countless cups of coffee. Even though the series was in its seventh year at the time, I did not start to watch the show until that season. -

Motherhood: Designing Silent Player Characters for Storytelling
Motherhood: Designing Silent Player Characters for Storytelling Extended Abstract Bria Mears Jichen Zhu Drexel University Drexel University 3141 Chestnut St 3141 Chestnut St Philadelphia, Pennsylvania 19104 Philadelphia, Pennsylvania 19104 [email protected] [email protected] ABSTRACT a list of methods designers can use to eectively communicate a e silent player character (SPC) is a reoccurring but not well- SPC’s story. ird, we developed Motherhood, a short narrative understood type of player character in narrative-driven games. In experience featuring a SPC that exemplies how our found pat- this paper, we present how our ndings from an analysis of SPC terns can be implemented into a game’s design to communicate development have been exemplied in an interactive narrative a pre-dened SPC. Motherhood was built to evaluate the paerns experience. e ndings presented in this study were approved as developed in this study. a FDG’17 poster submission. First, we identify two main types of SPCs: projective and expressive characters. Second, we synthesized 2 RELATED WORK a list of methods designers can use to eectively communicate A traditional silent protagonist is oen linked with the term “avatar” a SPC’s story. ird, we present Motherhood, a short narrative - dened as “a player’s embodiment in the game” [2, 3]; in other experience featuring the development of a pre-dened SPC. words, the “blank canvas” PC. In the early days of digital games, CCS CONCEPTS game characters were lile more than generic gures that lacked both personality and depth in their design [9] and players played •So ware and its engineering ! Interactive games; •Applied through the game [1], focusing on their ludic goals, rather than computing ! Computer games; taking an interest in the avatar itself. -

Motherhood in Science – How Children Change Our Academic Careers
October 2020 Motherhood in Science – How children change our academic careers Experiences shared by the GYA Women in Science Working Group Nova Ahmed, Amal Amin, Shalini S. Arya, Mary Donnabelle Balela, Ghada Bassioni, Flavia Ferreira Pires, Ana M. González Ramos, Mimi Haryani Hassim, Roula Inglesi-Lotz, Mari-Vaughn V. Johnson, Sandeep Kaur-Ghumaan, Rym Kefi-Ben Atig, Seda Keskin, Sandra López-Vergès, Vanny Narita, Camila Ortolan Cervone, Milica Pešic, Anina Rich, Özge Yaka, Karin Carmit Yefet, Meron Zeleke Eresso Motherhood in Science Motherhood in Science Table of Contents Preface The modern scientist’s journey towards excellence is multidimensional and requires skills in balancing all the responsibilities consistently and in a timely Preface 3 manner. Even though progress has been achieved in recent times, when the Chapter 1: Introductory thoughts 5 academic is a “mother”, the roles toggle with different priorities involving ca- Section 1: Setting the scene of motherhood in science nowadays 8 reer, family and more. A professional mother working towards a deadline may Chapter 2: Why do we translate family and employment as competitive spheres? 8 change her role to a full-time mother once her child needs exclusive attention. Chapter 3: The “Problem that Has No Name”: giving voice to invisible Mothers-to-Be The experience of motherhood is challenging yet humbling as shared by eight- in academia 16 Chapter 4: Motherhood and science – who knew? 24 een women from the Women in Science Working Group of the Global Young Academy in this publication. Section 2: Balancing science and motherhood 29 Chapter 5: Motherhood: a journey of surprises 29 The decision of a woman to become a mother is rooted in a range of reasons Chapter 6: Following a schedule 32 Chapter 7: Motivation, persistence and harmony 35 – genetic, cultural, harmonic, societal, and others. -
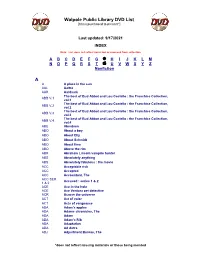
Walpole Public Library DVD List A
Walpole Public Library DVD List [Items purchased to present*] Last updated: 9/17/2021 INDEX Note: List does not reflect items lost or removed from collection A B C D E F G H I J K L M N O P Q R S T U V W X Y Z Nonfiction A A A place in the sun AAL Aaltra AAR Aardvark The best of Bud Abbot and Lou Costello : the Franchise Collection, ABB V.1 vol.1 The best of Bud Abbot and Lou Costello : the Franchise Collection, ABB V.2 vol.2 The best of Bud Abbot and Lou Costello : the Franchise Collection, ABB V.3 vol.3 The best of Bud Abbot and Lou Costello : the Franchise Collection, ABB V.4 vol.4 ABE Aberdeen ABO About a boy ABO About Elly ABO About Schmidt ABO About time ABO Above the rim ABR Abraham Lincoln vampire hunter ABS Absolutely anything ABS Absolutely fabulous : the movie ACC Acceptable risk ACC Accepted ACC Accountant, The ACC SER. Accused : series 1 & 2 1 & 2 ACE Ace in the hole ACE Ace Ventura pet detective ACR Across the universe ACT Act of valor ACT Acts of vengeance ADA Adam's apples ADA Adams chronicles, The ADA Adam ADA Adam’s Rib ADA Adaptation ADA Ad Astra ADJ Adjustment Bureau, The *does not reflect missing materials or those being mended Walpole Public Library DVD List [Items purchased to present*] ADM Admission ADO Adopt a highway ADR Adrift ADU Adult world ADV Adventure of Sherlock Holmes’ smarter brother, The ADV The adventures of Baron Munchausen ADV Adverse AEO Aeon Flux AFF SEAS.1 Affair, The : season 1 AFF SEAS.2 Affair, The : season 2 AFF SEAS.3 Affair, The : season 3 AFF SEAS.4 Affair, The : season 4 AFF SEAS.5 Affair, -

Convenient Fictions
CONVENIENT FICTIONS: THE SCRIPT OF LESBIAN DESIRE IN THE POST-ELLEN ERA. A NEW ZEALAND PERSPECTIVE By Alison Julie Hopkins A thesis submitted to Victoria University of Wellington in fulfilment of the requirements for the degree of Doctor of Philosophy Victoria University of Wellington 2009 Acknowledgements I would like to acknowledge those people who have supported me in my endeavour to complete this thesis. In particular, I would like to thank Dr Alison Laurie and Dr Lesley Hall, for their guidance and expertise, and Dr Tony Schirato for his insights, all of which were instrumental in the completion of my study. I would also like to express my gratitude to all of those people who participated in the research, in particular Mark Pope, facilitator of the ‘School’s Out’ programme, the staff at LAGANZ, and the staff at the photographic archive of The Alexander Turnbull Library. I would also like to acknowledge the support of The Chief Censor, Bill Hastings, and The Office of Film and Literature Classification, throughout this study. Finally, I would like to thank my most ardent supporters, Virginia, Darcy, and Mo. ii Abstract Little has been published about the ascending trajectory of lesbian characters in prime-time television texts. Rarer still are analyses of lesbian fictions on New Zealand television. This study offers a robust and critical interrogation of Sapphic expression found in the New Zealand television landscape. More specifically, this thesis analyses fictional lesbian representation found in New Zealand’s prime-time, free-to-air television environment. It argues that television’s script of lesbian desire is more about illusion than inclusion, and that lesbian representation is a misnomer, both qualitatively and quantitively. -

Participant List
Participant List 10/20/2019 8:45:44 AM Category First Name Last Name Position Organization Nationality CSO Jillian Abballe UN Advocacy Officer and Anglican Communion United States Head of Office Ramil Abbasov Chariman of the Managing Spektr Socio-Economic Azerbaijan Board Researches and Development Public Union Babak Abbaszadeh President and Chief Toronto Centre for Global Canada Executive Officer Leadership in Financial Supervision Amr Abdallah Director, Gulf Programs Educaiton for Employment - United States EFE HAGAR ABDELRAHM African affairs & SDGs Unit Maat for Peace, Development Egypt AN Manager and Human Rights Abukar Abdi CEO Juba Foundation Kenya Nabil Abdo MENA Senior Policy Oxfam International Lebanon Advisor Mala Abdulaziz Executive director Swift Relief Foundation Nigeria Maryati Abdullah Director/National Publish What You Pay Indonesia Coordinator Indonesia Yussuf Abdullahi Regional Team Lead Pact Kenya Abdulahi Abdulraheem Executive Director Initiative for Sound Education Nigeria Relationship & Health Muttaqa Abdulra'uf Research Fellow International Trade Union Nigeria Confederation (ITUC) Kehinde Abdulsalam Interfaith Minister Strength in Diversity Nigeria Development Centre, Nigeria Kassim Abdulsalam Zonal Coordinator/Field Strength in Diversity Nigeria Executive Development Centre, Nigeria and Farmers Advocacy and Support Initiative in Nig Shahlo Abdunabizoda Director Jahon Tajikistan Shontaye Abegaz Executive Director International Insitute for Human United States Security Subhashini Abeysinghe Research Director Verite -

The Next Gen Art Collectors 2021
COLLECTORS 1 THE NEXT COLLECTORS REPORT 2021 3 LARRY’S LIST is pleased to present The Next Gen that have not yet been acknowledged or made visible For us, size wasn’t a main consideration. Indeed, not a blue-chip artist will most likely generate more “likes” FOREWORDArt Collectors Report. Here, we continue our mission on a global scale. We want to share their stories and everyone listed has a large collection; charmingly, the than an unknown artist in an equally brilliant interior of monitoring global happenings, developments and thoughts. Next Gen often have collections in the making. The setting. But we still try to balance it and set aside any trends in the art world—particularly in the contemporary We also consider LARRY’S LIST as a guide and tool process is a development that happens over years care about the algorithm. art collector field—by looking extensively at the next for practitioners. We share and name collectors, those and so a mid-20-year-old collector may not yet be at generation of young art collectors on the scene. Over people who are buying art and contributing to the the same stage in their collection as someone in their Final words the past few months, we have investigated and profiled art scene. The Next Gen Art Collectors Report is a late 30s. I would like to express my gratitude to all the collectors these collectors, answering the questions central to this resource for artists, galleries, dealers, a general art- The end result of our efforts is this report listing over we exchanged with in the preparation of this report topic: Who are these collectors founding the next art interested audience and, of course, peer collectors. -
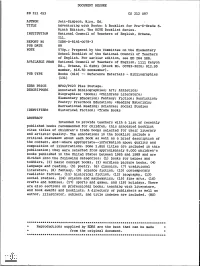
Adventuring with Books: a Booklist for Pre-K-Grade 6. the NCTE Booklist
DOCUMENT RESUME ED 311 453 CS 212 097 AUTHOR Jett-Simpson, Mary, Ed. TITLE Adventuring with Books: A Booklist for Pre-K-Grade 6. Ninth Edition. The NCTE Booklist Series. INSTITUTION National Council of Teachers of English, Urbana, Ill. REPORT NO ISBN-0-8141-0078-3 PUB DATE 89 NOTE 570p.; Prepared by the Committee on the Elementary School Booklist of the National Council of Teachers of English. For earlier edition, see ED 264 588. AVAILABLE FROMNational Council of Teachers of English, 1111 Kenyon Rd., Urbana, IL 61801 (Stock No. 00783-3020; $12.95 member, $16.50 nonmember). PUB TYPE Books (010) -- Reference Materials - Bibliographies (131) EDRS PRICE MF02/PC23 Plus Postage. DESCRIPTORS Annotated Bibliographies; Art; Athletics; Biographies; *Books; *Childress Literature; Elementary Education; Fantasy; Fiction; Nonfiction; Poetry; Preschool Education; *Reading Materials; Recreational Reading; Sciences; Social Studies IDENTIFIERS Historical Fiction; *Trade Books ABSTRACT Intended to provide teachers with a list of recently published books recommended for children, this annotated booklist cites titles of children's trade books selected for their literary and artistic quality. The annotations in the booklist include a critical statement about each book as well as a brief description of the content, and--where appropriate--information about quality and composition of illustrations. Some 1,800 titles are included in this publication; they were selected from approximately 8,000 children's books published in the United States between 1985 and 1989 and are divided into the following categories: (1) books for babies and toddlers, (2) basic concept books, (3) wordless picture books, (4) language and reading, (5) poetry. (6) classics, (7) traditional literature, (8) fantasy,(9) science fiction, (10) contemporary realistic fiction, (11) historical fiction, (12) biography, (13) social studies, (14) science and mathematics, (15) fine arts, (16) crafts and hobbies, (17) sports and games, and (18) holidays. -

Chester County Ledger
Chester County Ledger The Newsletter of the Chester County Historic Preservation Network www.cchpn.org Volume 22 Number 1 Established 1997 March 2019 The 30th Anniversary of “Jane’s Army” Chester County Ledger www.cchpn.org Page 2 March 2019 Chester County Ledger www.cchpn.org Page 3 March 2019 THE PRESIDENT’S LETTER: The President’s Letter: Becoming a Trusted Partner This year the Chester County Historic Preservation Network is celebrating its 30th Anniversary. There have been many accomplish- ments over the years from the founding to a thriving organization still sustained largely by volunteer efforts from across the County. With thir- ty years of building an ever-expanding network and developing expertise in the incredibly broad field of historic preservation, the organization has become a recognized place to go for guidance in everything from the smallest local issue to having a voice at a county and state level in preser- vation matters. In the field of professional services, reputation has to be earned. James B. Garrison A good reputation brings credibility and a place at the table where deci- sions are made. The group effort that has gone into making the reputa- tion of the Network is truly inspirational. It shows that a combination of Table of Contents enthusiasm, interest, and a diverse set of skills can come together with a Pg. Article and Author strong message. Historic preservation does not always have a happy or 3. President’s Letter—James B. easy message to deliver, but few issues that arise are really unique or oc- Garrison curring for the first time. -

Developing Character Through Literature: a Teacher's Resource Book
DOCUMENT RESUME ED 464 362 CS 511 101 TITLE Developing Character through Literature: A Teacher's Resource Book. INSTITUTION ERIC Clearinghouse on Reading, English, and Communication, Bloomington, IN.; Family Learning Association, Bloomington, IN. SPONS AGENCY Office of Educational Research and Improvement (ED), Washington, DC. ISBN ISBN-0-9719874-3-2 PUB DATE 2002-05-00 NOTE 187p. CONTRACT ED-99-CO-0028 AVAILABLE FROM ERIC Clearinghouse on Reading, English, and Communication, Indiana University, 2805 E. 10th Street, Suite 140, Bloomington, IN 47408-2698. Family Learning Association, 3925 Hagan St., Suite 101, Bloomington, IN 47401 (Order # 180-2199, $19.95). Tel: 800-759-4723 (Toll Free); Fax: 812-331-2776; Web site: http://kidscanlearn.com. PUB TYPE Guides - Classroom - Teacher (052) -- ERIC Publications (071) -- Reference Materials - Bibliographies (131) EDRS PRICE MFOl/PC08 Plus Postage. DESCRIPTORS *Adolescent Literature; Annotated Bibliographies; *Childrens Literature; *Citizenship Education; Concept Formation; Elementary Secondary Education; *Individual Development; Learning Activities; *Values Education IDENTIFIERS *Character Development; Character Education; Family Activities; *Trade Books ABSTRACT Based on the idea that the most important foundation of education is character development, this book guides teachers and parents in building strong character traits while reading and discussing popular books. Children's books and young adult books draw students into discussions that can lead to action and to personal development. Thoughtful teachers and parents can ,use that literature and the activities suggested in.this book as a means of bringing their children to the commitments that will gradually form character traits and citizenship attitudes that everyone is proud to acknowledge. The units in the book stand for the most commonly described topics in character education: responsibility, honesty, integrity, respect, living peaceably, caring, civility, and the golden rule. -
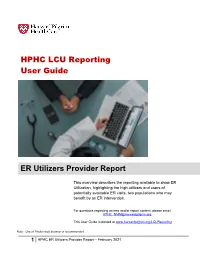
HPHC LCU Reporting User Guide ER Utilizers Provider Report
HPHC LCU Reporting User Guide ER Utilizers Provider Report This overview describes the reporting available to show ER Utilization, highlighting the high utilizers and users of potentially avoidable ER visits, two populations who may benefit by an ER intervention. For questions regarding access and/or report content, please email [email protected] This User Guide is posted at www.harvardpilgrim.org/LCUReporting Note: Use of Firefox web browser is recommended. 1 HPHC ER Utilizers Provider Report – February 2021 1.0 Introduction This user guide introduces clinical staff within our provider groups to the HPHC tools to identify patients’ utilization of ER services. This report offers an interactive, parameter-driven application which allow the user to select the desired date span specifications. The report output contains a summary level tab, with patient specific summary, including summary metrics: . # ER visits in last 6 months . # ER visits in last 12 months . # Return visits to the ER (within 30 days) . # Visits which are considered potentially avoidable (using the NYU/Billings algorithm described in appendix). 2.0 Navigating to the Care and Disease Management folder Once you are logged in to the web application, you will see the following screen: Click on the icon and you will see the following screen. Select the Shared Reports icon. Please note the PI/PHI Privacy Notice displayed. Click on the desired report name. Please allow a few moments for the next page to load. 2 HPHC ER Utilizers Provider Report – February 2021 Medicare STRIDE: Note the option for the Medicare drill path for users with Medicare reporting access. -

Biennial Report 1999 / 2000 Dedication
Chicago Police Department Richard M. Daley Mayor Terry G. Hillard Biennial Report 1999 / 2000 Superintendent of Police Dedication he 1999/2000 Biennial Report T is dedicated to all the men and women of the Chicago Police Department who have given their lives in service to the City of Chicago and its residents. Especially, Officer John C. Knight #5199 and Officer James H. Camp #3934 who died in the line of duty during 1999, and Officer Myles M. Smetana #14658 and Sergeant Alane Stoffregen #1203 who died in the performance of duty during 1999 and 2000, respectively. “You will always be remembered.” www.cityofchicago/caps Mission Statement he Chicago Police T Department, as part of, Biennial Report and empowered by the community, is committed 1999 / 2000 to protect the lives, property and rights of all people, to maintain order and to enforce the law impartially. Chicago Police We will provide quality police service in partnership Department with other members of the community. To fulfill our mission, we will strive to attain the highest degree of ethical behavior and professional conduct at all times. Prepared by the Chicago Police Department Research and Development Division Table of Message from the Superintendent . .4 Organization for Command . .5 Contents Fig. 1. Organization for Command . .6 Crime Trends . .5 Fig. 2a. Total Index Crime 1991 - 2000 . .7 Fig. 2b. Violent vs. Property Crimes . .8 Fig. 2c. Violent Crimes . .8 Fig. 2d. Property Crimes . .8 Fig. 2e. Index Crimes . .9 Chicago Police Districts . .8 Fig. 3a. Chicago Police Districts . .10 Fig. 3b. Police District Land Areas . .10 Fig.