125509 Obiltoxaximab Clinpharm PREA
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Where Do Novel Drugs of 2016 Fit In?
FORMULARY JEOPARDY: WHERE DO NOVEL DRUGS OF 2016 FIT IN? Maabo Kludze, PharmD, MBA, CDE, BCPS, Associate Director Elizabeth A. Shlom, PharmD, BCPS, SVP & Director Clinical Pharmacy Program Acurity, Inc. Privileged and Confidential August 15, 2017 Privileged and Confidential Program Objectives By the end of the presentation, the pharmacist or pharmacy technician participant will be able to: ◆ Identify orphan drugs and first-in-class medications approved by the FDA in 2016. ◆ Describe the role of new agents approved for use in oncology patients. ◆ Identify and discuss the role of novel monoclonal antibodies. ◆ Discuss at least two new medications that address public health concerns. Neither Dr. Kludze nor Dr. Shlom have any conflicts of interest in regards to this presentation. Privileged and Confidential 2016 NDA Approvals (NMEs/BLAs) ◆ Nuplazid (primavanserin) P ◆ Adlyxin (lixisenatide) ◆ Ocaliva (obeticholic acid) P, O ◆ Anthim (obitoxaximab) O ◆ Rubraca (rucaparib camsylate) P, O ◆ Axumin (fluciclovive F18) P ◆ Spinraza (nusinersen sodium) P, O ◆ Briviact (brivaracetam) ◆ Taltz (ixekizumab) ◆ Cinqair (reslizumab) ◆ Tecentriq (atezolizumab) P ◆ Defitelio (defibrotide sodium) P, O ◆ Venclexta (venetoclax) P, O ◆ Epclusa (sofosburvir and velpatasvir) P ◆ Xiidra (lifitigrast) P ◆ Eucrisa (crisaborole) ◆ Zepatier (elbasvir and grazoprevir) P ◆ Exondys 51 (eteplirsen) P, O ◆ Zinbyrta (daclizumab) ◆ Lartruvo (olaratumab) P, O ◆ Zinplava (bezlotoxumab) P ◆ NETSTPOT (gallium Ga 68 dotatate) P, O O = Orphan; P = Priority Review; Red = BLA Privileged and Confidential History of FDA Approvals Privileged and Confidential Orphan Drugs ◆FDA Office of Orphan Products Development • Orphan Drug Act (1983) – drugs and biologics . “intended for safe and effective treatment, diagnosis or prevention of rare diseases/disorders that affect fewer than 200,000 people in the U.S. -

These Highlights Do Not Include All the Information Needed to Use ANTHIM Safely and Effectively. See Full Prescribing Information for ANTHIM
ANTHIM - obiltoxaximab solution Elusys Therapeutics, Inc. ---------- HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use ANTHIM safely and effectively. See full prescribing information for ANTHIM. ANTHIM® (obiltoxaximab) injection, for intravenous use Initial U.S. Approval: 2016 WARNING: HYPERSENSITIVITY and ANAPHYLAXIS See full prescribing information for complete boxed warning. Hypersensitivity reactions, including anaphylaxis, have been reported during ANTHIM infusion (5.1) ANTHIM should be administered in monitored settings by personnel trained and equipped to manage anaphylaxis (1.2, 2.4, 5.1) Stop ANTHIM infusion immediately and treat appropriately if hypersensitivity or anaphylaxis occurs (2.4, 5.1) INDICATIONS AND USAGE ANTHIM® is a monoclonal antibody directed against the protective antigen of Bacillus anthracis. It is indicated in adult and pediatric patients for treatment of inhalational anthrax due to B. anthracis in combination with appropriate antibacterial drugs and, for prophylaxis of inhalational anthrax when alternative therapies are not available or are not appropriate. (1.1) Limitations of Use ANTHIM should only be used for prophylaxis when its benefit for prevention of inhalational anthrax outweighs the risk of hypersensitivity and anaphylaxis. (1.2, 5.1) The effectiveness of ANTHIM is based solely on efficacy studies in animal models of inhalational anthrax. (1.2, 14) There have been no studies of the safety or pharmacokinetics (PK) of ANTHIM in the pediatric population. Dosing in pediatric patients was derived using a population PK approach. (1.2, 8.4) ANTHIM does not have direct antibacterial activity. ANTHIM should be used in combination with appropriate antibacterial drugs. (1.2) ANTHIM is not expected to cross the blood-brain barrier and does not prevent or treat meningitis. -

Pulmonary Delivery of Biological Drugs
pharmaceutics Review Pulmonary Delivery of Biological Drugs Wanling Liang 1,*, Harry W. Pan 1 , Driton Vllasaliu 2 and Jenny K. W. Lam 1 1 Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, 21 Sassoon Road, Pokfulam, Hong Kong, China; [email protected] (H.W.P.); [email protected] (J.K.W.L.) 2 School of Cancer and Pharmaceutical Sciences, King’s College London, 150 Stamford Street, London SE1 9NH, UK; [email protected] * Correspondence: [email protected]; Tel.: +852-3917-9024 Received: 15 September 2020; Accepted: 20 October 2020; Published: 26 October 2020 Abstract: In the last decade, biological drugs have rapidly proliferated and have now become an important therapeutic modality. This is because of their high potency, high specificity and desirable safety profile. The majority of biological drugs are peptide- and protein-based therapeutics with poor oral bioavailability. They are normally administered by parenteral injection (with a very few exceptions). Pulmonary delivery is an attractive non-invasive alternative route of administration for local and systemic delivery of biologics with immense potential to treat various diseases, including diabetes, cystic fibrosis, respiratory viral infection and asthma, etc. The massive surface area and extensive vascularisation in the lungs enable rapid absorption and fast onset of action. Despite the benefits of pulmonary delivery, development of inhalable biological drug is a challenging task. There are various anatomical, physiological and immunological barriers that affect the therapeutic efficacy of inhaled formulations. This review assesses the characteristics of biological drugs and the barriers to pulmonary drug delivery. -

125509Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 125509Orig1s000 ADMINISTRATIVE and CORRESPONDENCE DOCUMENTS ACTION PACKAGE CHECKLIST APPLICATION INFORMATION1 If NDA, Efficacy Supplement Type: BLA #125509 BLA Supplement # (an action package is not required for SE8 or SE9 supplements) Proprietary Name: Anthim Applicant: Elusys Therapeutics, Inc. Established/Proper Name: obiltoxaximab Agent for Applicant (if applicable): Dosage Form: injection RPM: Jane A. Dean, RN, MSN Division: Division of Anti-Infective Products For ALL 505(b)(2) applications, two months prior to EVERY action: NDA Application Type: 505(b)(1) 505(b)(2) Efficacy Supplement: 505(b)(1) 505(b)(2) Review the information in the 505(b)(2) Assessment and submit the draft2 to CDER OND IO for clearance. BLA Application Type: 351(k) 351(a) Check Orange Book for newly listed patents and/or Efficacy Supplement: 351(k) 351(a) exclusivity (including pediatric exclusivity) No changes New patent/exclusivity (notify CDER OND IO) Date of check: Note: If pediatric exclusivity has been granted or the pediatric information in the labeling of the listed drug changed, determine whether pediatric information needs to be added to or deleted from the labeling of this drug. Actions Proposed action AP TA CR User Fee Goal Date is 3/20/16 Previous actions (specify type and date for each action taken) None If accelerated approval or approval based on efficacy studies in animals, were promotional materials received? Note: Promotional materials to be used within 120 days after approval must have been Received submitted (for exceptions, see http://www fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guida nces/ucm069965.pdf). -
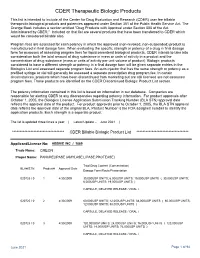
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database. -

Ride'n Drive on Government Waste
NEWS Table 1 Anthrax countermeasures in development Company Product Stage of development BARDA contract Human Genome Sciences ABthrax (raxibacumab), a human mAb against anthrax protective Biologic license $151 million antigen (PA) application Emergent BioSolutions AV-7909, a combination of BioThrax (aluminum-adsorbed cell- Phase 2 $447.6 million free filtrates of unencapsulated Bacillus anthracis) and Coley Pharmaceutical’s VaxImmune (an unmethylated CpG-motif oligonucleotide that acts as an agonist of Toll-like receptor 9) Anthrax immune globulin (AIGIV), polyclonal antibodies raised Phase 1/2 $13 million against BioThrax Elusys Therapeutics Anthim (ETI-204), a humanized mAb against PA Phase 1 Up to $143 million PharmAthene SparVax, an injectable rPA absorbed on to hydrogel Phase 2 $3.9 million NIAID DynPort Vaccine Anthrax vaccine, an injectable rPA vaccine Phase 1 NA Medarex, a subsidiary of Valortim (MDX-1303), a fully human mAb against PA Phase 1 $1 million from the US Department Bristol-Myers Squibb of Defense (DoD) payable to partner PHarmAthene Advanced Life Sciences Restanza, a once-daily oral ketolide cethromycin that inhibits Preclinical $3.8 million from DoD B. anthracis protein synthesis Sources: Sagient Research, BiomedTracker and BARDA. NA, Not available. Even with government support, PharmAthene For the US government, anthrax treatment procurement contract with the Centers for and other companies working under biodefense remains a critical element in its biodefense Disease Control and Prevention of Atlanta, contracts face the stark reality of drug develop- strategies. Emergent Solutions currently Georgia, to manufacture and deliver 14.5 ment: 30% of all candidates that reach phase manufactures the only approved vaccine for million doses of BioThrax for the strategic 3 clinical trials within the eight-year BARDA anthrax based on protective antigen (PA). -

Statistical Review(S)
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 125509Orig1s000 STATISTICAL REVIEW(S) U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research Office of Translational Sciences Office of Biostatistics S TATISTICAL R EVIEW AND E VA LU ATI O N ANIMAL EFFICACY STUDIES NDA/BLA #: BLA 125509 Drug Name: Anthim®(obiltoxaximab) 16 mg/kg IV Indication(s): Treatment and Prophylaxis of Inhalational Anthrax due to Bacillus anthracis Applicant: Elusys Therapeutics, Inc. Date(s): Submission date: 3/20/2015. PDUFA due date: 3/18/2016 Review Priority: Standard Biometrics Division: Division of Biometrics IV Statistical Reviewer: Xianbin Li, PhD Concurring Reviewers: Karen Higgins, ScD Daphne Lin, PhD Medical Division: Division of Anti-Infective Products (DAIP) Clinical Team: Elizabeth O'Shaughnessy, MD, Medical Reviewer John Alexander, MD, Medical Team Leader Sumathi Nambiar, MD, Medical Director Project Manager: Jane Dean, RN MSN Keywords: Animal efficacy studies Reference ID: 3859664 Table of Contents 1 EXECUTIVE SUMMARY .................................................................................................. 11 2 INTRODUCTION ................................................................................................................ 12 2.1 OVERVIEW ........................................................................................................................ 12 2.2 DATA SOURCES ............................................................................................................... -

Studies on Antitoxin Use for Postexposure Prophylaxis (PEP)
ACIP Anthrax Vaccine Work Group William Bower, MD, FIDSA Epidemiology Team Lead Bacterial Special Pathogens October 23, 2018 National Center for Emerging and Zoonotic Disease Division of High-Consequence Pathogens and Pathology Outline Overview of anthrax antitoxins Studies on antitoxin use for postexposure prophylaxis (PEP) . Anthrax antitoxin for PEP and survival in animal models . Anthrax antitoxin effect on acquired immunity . Anthrax antitoxin use with anthrax vaccine adsorbed (AVA) Work group discussions Guidance on anthrax antitoxin use for PEP 2 Anthrax Pathogenesis 3 Background – Anthrax Antitoxins There are currently three FDA approved anthrax antitoxins RAXIBACUMAB . Initial U.S. Approval: 2012 . Human IgG1λ monoclonal antibody that binds the protective antigen (PA) component of Bacillus anthracis toxin ANTHRASIL (Anthrax Immune Globulin Intravenous (AIGIV)) . Initial U.S. Approval: 2015 . Purified human IgG containing polyclonal antibodies that bind the protective antigen (PA) component of B. anthracis lethal and edema toxins collected from individuals immunized with AVA ANTHIM (obiltoxaximab) . Initial U.S. Approval: 2016 . Chimeric IgG1 kappa monoclonal antibody that binds the PA component of B. anthracis toxin 4 Background – Anthrax Antitoxins Indications Anthrax antitoxins all have an indication for the treatment of adult and pediatric patients with inhalation anthrax due to B. anthracis in combination with appropriate antimicrobials The monoclonal antitoxins, raxibacumab and obiltoxaximab, are also indicated for -

ENTRY WATCH 2016 Published by the Patented Medicine Prices Review Board June 2018 Meds Entry Watch, 2016 Is Available in Electronic Format on the PMPRB Website
MEDS ENTRY WATCH 2016 Published by the Patented Medicine Prices Review Board June 2018 Meds Entry Watch, 2016 is available in electronic format on the PMPRB website. Une traduction de ce document est également disponible en français sous le titre : Veille des médicaments mis en marché, 2016 Patented Medicine Prices Review Board Standard Life Centre Box L40 333 Laurier Avenue West Suite 1400 Ottawa, ON K1P 1C1 Tel.: 1-877-861-2350 TTY 613-288-9654 Email: [email protected] Web: www.pmprb-cepmb.gc.ca ISSN 2560-6204 Cat. No.: H79-12E-PDF © Her Majesty the Queen in Right of Canada, as represented by the NPDUIS initiative of the Patented Medicine Prices Review Board, 2018 MEDS ENTRY WATCH 2016 About the PMPRB Acknowledgements The Patented Medicine Prices Review Board This report was prepared by the Patented (PMPRB) is a respected public agency that makes Medicine Prices Review Board (PMPRB) a unique and valued contribution to sustainable as part of the National Prescription Drug spending on pharmaceuticals in Canada by: Utilization Information System (NPDUIS). ~ providing stakeholders with price, cost and The PMPRB would like to acknowledge the utilization information to help them make timely contributions of and knowledgeable drug pricing, purchasing and ~ The members of the NPDUIS Advisory reimbursement decisions; and Committee for their expert oversight and ~ acting as an effective check on the patent rights guidance in the preparation of this report. of pharmaceutical manufacturers through the ~ PMPRB NPDUIS staff for their contribution responsible and efficient use of its consumer to the analytical content of the report: protection powers. -

PRESCRIBING INFORMATION • Pre-Medicate with Diphenhydramine
----------------------- DOSAGE AND ADMINISTRATION ----------------------- HIGHLIGHTS OF PRESCRIBING INFORMATION • Pre-medicate with diphenhydramine. (2.1, 5.1) These highlights do not include all the information needed to use • Recommended Dosage of ANTHIM: ANTHIM safely and effectively. See full prescribing information for o Adult Patients: 16 mg/kg. (2.1) ANTHIM. o Pediatric Patients: (2.2) ➢ Greater than 40 kg: 16 mg/kg ANTHIM® (obiltoxaximab) injection, for intravenous use ➢ Greater than 15 kg to 40 kg: 24 mg/kg Initial U.S. Approval: 2016 ➢ Less than or equal to 15 kg: 32 mg/kg • Dilute the injection in 0.9% Sodium Chloride Injection, USP, before WARNING: HYPERSENSITIVITY and ANAPHYLAXIS administering as an intravenous (IV) infusion over 1 hour and 30 minutes. See full prescribing information for complete boxed warning. (2.3) • Administer ANTHIM in a monitored setting equipped to manage • Hypersensitivity reactions, including anaphylaxis, have been anaphylaxis. (2.4, 5.1) reported during ANTHIM infusion (5.1) • See Full Prescribing Information for instructions on preparation, dilution • ANTHIM should be administered in monitored settings by and administration of ANTHIM injection. (2.3, 2.4) personnel trained and equipped to manage anaphylaxis (1.2, 2.4, 5.1) --------------------- DOSAGE FORMS AND STRENGTHS --------------------- • Stop ANTHIM infusion immediately and treat appropriately if Injection: 600 mg/6 mL (100 mg/mL) solution in single-dose vial. (3) hypersensitivity or anaphylaxis occurs (2.4, 5.1) ------------------------------ CONTRAINDICATIONS ------------------------------ None (4) --------------------------- INDICATIONS AND USAGE ---------------------------- ANTHIM® is a monoclonal antibody directed against the protective antigen of ----------------------- WARNINGS AND PRECAUTIONS ----------------------- Bacillus anthracis. It is indicated in adult and pediatric patients for treatment Hypersensitivity reactions, including anaphylaxis (Boxed Warning, 1.2, 2.1, of inhalational anthrax due to B. -

Therapeutic Monoclonal Antibodies for Respiratory Diseases: Current Challenges & Perspectives March 31 - April 1, 2016
Therapeutic Monoclonal Antibodies for Respiratory Diseases: Current Challenges & Perspectives March 31 - April 1, 2016 Janice M. Reichert, Ph.D. Executive Director, The Antibody Society Editor-in-Chief, mAbs 1 Topics for discussion Overview of the antibody therapeutics clinical pipeline* ‘Other’ disorders, incl. respiratory disorders Antibodies recently approved or in regulatory review Antibodies in clinical studies Prospects for 2016 *Disclaimer: Commercial development; only public domain information known as of Feb 15, 2016 is included. It should be noted that frequent changes to the data occur over time. 2 3 Novel antibodies entering clinic* 120 102 100 81 80 66 54 60 50 40 20 0 2011 2012 2013 2014 2015 Year of first clinical study *Commercial development only Antibodies in Phase 3 studies 60 53 50 39 40 33 29 30 26 25 25 20 Number of mAbs in Phase 3 Phase in mAbs of Number 10 0 2010 2011 2012 2013 2014 2015 2016 Year of article publication Data from ‘Antibodies to watch’ articles published in mAbs. 5 10 11 Number of first approvals for mAbs of mAbs US or EU approvals First 0 1 2 3 4 5 6 7 8 9 the US or EU (antibodysociety.org) or US the in or in review approved of antibodies Table Source: approvals. number of first *Projected 97 98 99 00 01 02 Year of first US EUor approval of first Year 03 04 05 06 07 08 09 10 11 12 13 14 15 10+ ? 6 16* Three approvals in 2016 so far… Obiltoxaximab, targeting PA of B. anthracis exotoxin approved by FDA on March 18 ANTHIM® is indicated in adult and pediatric patients for treatment of inhalational anthrax due to Bacillus anthracis in combination with appropriate antibacterial drugs, and for prophylaxis of inhalational anthrax when alternative therapies are not available or appropriate. -

125509Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 125509Orig1s000 OTHER REVIEW(S) REGULATORY PROJECT MANAGER PHYSICIAN’S LABELING RULE (PLR) FORMAT REVIEW OF THE PRESCRIBING INFORMATION Complete for all new NDAs, BLAs, Efficacy Supplements, and PLR Conversion Labeling Supplements Application: BLA 125509 Application Type: New BLA Name of Drug/Dosage Form: Anthim (obiltoxaximab) Injection, for intravenous use Applicant: Elusys Therapeutics Receipt Date: March 20, 2015 Goal Date: March 18, 2016 1. Regulatory History and Applicant’s Main Proposals Elusys Therapeutics, Inc. submitted a new Biologics Licensing Application (BLA) under section 351(a) of the Public Health Service Act and 21CFR Part 601, Subpart H (Approval of a Biologic Product When Human Efficacy Studies are not Ethical or Feasible) Anthim (obiltoxaximab) with the following indications: treatment of adult and pediatric patients with inhalational anthrax due to Bacillus anthracis in combination with appropriate antibacterial drugs and prophylaxis of inhaltional anthrax when alternative therapies are not available or are not appropriate. 2. Review of the Prescribing Information This review is based on the applicant’s submitted Word format of the prescribing information (PI). The applicant’s proposed PI was reviewed in accordance with the labeling format requirements listed in the “Selected Requirements for Prescribing Information (SRPI)” checklist (see Section 4 of this review). 3. Conclusions/Recommendations No SRPI format deficiencies were identified in the review of this PI. 4. Selected Requirements of Prescribing Information The Selected Requirement of Prescribing Information (SRPI) is a 41-item, drop-down checklist of important format elements of the prescribing information (PI) based on labeling regulations (21 CFR 201.56 and 201.57) and guidances.