Downloads/Drugs/Drugsafety/UCM231731
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug-Resistant Streptococcus Pneumoniae and Methicillin
NEWS & NOTES Conference Summary pneumoniae can vary among popula- conference sessions was that statically tions and is influenced by local pre- sound methods of data collection that Drug-resistant scribing practices and the prevalence capture valid, meaningful, and useful of resistant clones. Conference pre- data and meet the financial restric- Streptococcus senters discussed the role of surveil- tions of state budgets are indicated. pneumoniae and lance in raising awareness of the Active, population-based surveil- Methicillin- resistance problem and in monitoring lance for collecting relevant isolates is the effectiveness of prevention and considered the standard criterion. resistant control programs. National- and state- Unfortunately, this type of surveil- Staphylococcus level epidemiologists discussed the lance is labor-intensive and costly, aureus benefits of including state-level sur- making it an impractical choice for 1 veillance data with appropriate antibi- many states. The challenges of isolate Surveillance otic use programs designed to address collection, packaging and transport, The Centers for Disease Control the antibiotic prescribing practices of data collection, and analysis may and Prevention (CDC) convened a clinicians. The potential for local sur- place an unacceptable workload on conference on March 12–13, 2003, in veillance to provide information on laboratory and epidemiology person- Atlanta, Georgia, to discuss improv- the impact of a new pneumococcal nel. ing state-based surveillance of drug- vaccine for children was also exam- Epidemiologists from several state resistant Streptococcus pneumoniae ined; the vaccine has been shown to health departments that have elected (DRSP) and methicillin-resistant reduce infections caused by resistance to implement enhanced antimicrobial Staphylococcus aureus (MRSA). -
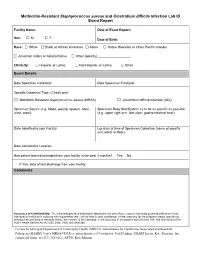
Methicillin-Resistant Staphylococcus Aureus and Clostridium Difficile Infection Lab ID Event Report
Methicillin-Resistant Staphylococcus aureus and Clostridium difficile Infection Lab ID Event Report Facility Name: Date of Event Report: Sex: M F □ □ Date of Birth: Race: □ White □ Black or African American □ Asian □ Native Hawaiian or Other Pacific Islander □ American Indian or Alaska Native □ Other [specify] __________________ Ethnicity: □ Hispanic or Latino □ Not Hispanic or Latino □ Other Event Details Date Specimen Collected: Date Specimen Finalized: Specific Organism Type: (Check one) □ Methicillin-Resistant Staphylococcus aureus (MRSA) □ Clostridium difficile Infection (CDI) Specimen Source (e.g. blood, wound, sputum, bone, Specimen Body Site/System try to be as specific as possible urine, stool): (e.g. upper right arm, foot ulcer, gastrointestinal tract): Date Admitted to your Facility: Location at time of Specimen Collection (name of specific unit, ward, or floor): Date Admitted to Location: Has patient been discharged from your facility in the past 3 months? Yes No If Yes, date of last discharge from your facility: Comments Assurance of Confidentiality: The voluntarily provided information obtained in this surveillance system that would permit identification of any individual or institution is collected with a guarantee that it will be held in strict confidence, will be used only for the purposes stated, and will not otherwise be disclosed or released without the consent of the individual, or the institution in accordance with Sections 304, 306 and 308(d) of the Public Health Service Act (42 USC 242b, 242k, and 242m(d)). For use by Michigan Department of Community Health (MDCH), Surveillance for Healthcare-Associated and Resistant Pathogens (SHARP) Unit’s MRSA/CDI Prevention Initiative (Coordinator: Gail Denkins, SHARP Intern: Kate Manton); fax completed forms to (517) 335-8263, ATTN: Kate Manton. -

These Highlights Do Not Include All the Information Needed to Use ANTHIM Safely and Effectively. See Full Prescribing Information for ANTHIM
ANTHIM - obiltoxaximab solution Elusys Therapeutics, Inc. ---------- HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use ANTHIM safely and effectively. See full prescribing information for ANTHIM. ANTHIM® (obiltoxaximab) injection, for intravenous use Initial U.S. Approval: 2016 WARNING: HYPERSENSITIVITY and ANAPHYLAXIS See full prescribing information for complete boxed warning. Hypersensitivity reactions, including anaphylaxis, have been reported during ANTHIM infusion (5.1) ANTHIM should be administered in monitored settings by personnel trained and equipped to manage anaphylaxis (1.2, 2.4, 5.1) Stop ANTHIM infusion immediately and treat appropriately if hypersensitivity or anaphylaxis occurs (2.4, 5.1) INDICATIONS AND USAGE ANTHIM® is a monoclonal antibody directed against the protective antigen of Bacillus anthracis. It is indicated in adult and pediatric patients for treatment of inhalational anthrax due to B. anthracis in combination with appropriate antibacterial drugs and, for prophylaxis of inhalational anthrax when alternative therapies are not available or are not appropriate. (1.1) Limitations of Use ANTHIM should only be used for prophylaxis when its benefit for prevention of inhalational anthrax outweighs the risk of hypersensitivity and anaphylaxis. (1.2, 5.1) The effectiveness of ANTHIM is based solely on efficacy studies in animal models of inhalational anthrax. (1.2, 14) There have been no studies of the safety or pharmacokinetics (PK) of ANTHIM in the pediatric population. Dosing in pediatric patients was derived using a population PK approach. (1.2, 8.4) ANTHIM does not have direct antibacterial activity. ANTHIM should be used in combination with appropriate antibacterial drugs. (1.2) ANTHIM is not expected to cross the blood-brain barrier and does not prevent or treat meningitis. -
Association Between Carriage of Streptococcus Pneumoniae and Staphylococcus Aureus in Children
BRIEF REPORT Association Between Carriage of Streptococcus pneumoniae and Staphylococcus aureus in Children Gili Regev-Yochay, MD Context Widespread pneumococcal conjugate vaccination may bring about epidemio- Ron Dagan, MD logic changes in upper respiratory tract flora of children. Of particular significance may Meir Raz, MD be an interaction between Streptococcus pneumoniae and Staphylococcus aureus, in view of the recent emergence of community-acquired methicillin-resistant S aureus. Yehuda Carmeli, MD, MPH Objective To examine the prevalence and risk factors of carriage of S pneumoniae Bracha Shainberg, PhD and S aureus in the prevaccination era in young children. Estela Derazne, MSc Design, Setting, and Patients Cross-sectional surveillance study of nasopharyn- geal carriage of S pneumoniae and nasal carriage of S aureus by 790 children aged 40 Galia Rahav, MD months or younger seen at primary care clinics in central Israel during February 2002. Ethan Rubinstein, MD Main Outcome Measures Carriage rates of S pneumoniae (by serotype) and S aureus; risk factors associated with carriage of each pathogen. TREPTOCOCCUS PNEUMONIAE AND Results Among 790 children screened, 43% carried S pneumoniae and 10% car- Staphylococcus aureus are com- ried S aureus. Staphylococcus aureus carriage among S pneumoniae carriers was 6.5% mon inhabitants of the upper vs 12.9% in S pneumoniae noncarriers. Streptococcus pneumoniae carriage among respiratory tract in children and S aureus carriers was 27.5% vs 44.8% in S aureus noncarriers. Only 2.8% carried both Sare responsible for common infec- pathogens concomitantly vs 4.3% expected dual carriage (P=.03). Risk factors for tions. Carriage of S aureus and S pneu- S pneumoniae carriage (attending day care, having young siblings, and age older than moniae can result in bacterial spread and 3 months) were negatively associated with S aureus carriage. -
Clostridium Difficile Infection: How to Deal with the Problem DH INFORMATION RE ADER B OX
Clostridium difficile infection: How to deal with the problem DH INFORMATION RE ADER B OX Policy Estates HR / Workforce Commissioning Management IM & T Planning / Finance Clinical Social Care / Partnership Working Document Purpose Best Practice Guidance Gateway Reference 9833 Title Clostridium difficile infection: How to deal with the problem Author DH and HPA Publication Date December 2008 Target Audience PCT CEs, NHS Trust CEs, SHA CEs, Care Trust CEs, Medical Directors, Directors of PH, Directors of Nursing, PCT PEC Chairs, NHS Trust Board Chairs, Special HA CEs, Directors of Infection Prevention and Control, Infection Control Teams, Health Protection Units, Chief Pharmacists Circulation List Description This guidance outlines newer evidence and approaches to delivering good infection control and environmental hygiene. It updates the 1994 guidance and takes into account a national framework for clinical governance which did not exist in 1994. Cross Ref N/A Superseded Docs Clostridium difficile Infection Prevention and Management (1994) Action Required CEs to consider with DIPCs and other colleagues Timing N/A Contact Details Healthcare Associated Infection and Antimicrobial Resistance Department of Health Room 528, Wellington House 133-155 Waterloo Road London SE1 8UG For Recipient's Use Front cover image: Clostridium difficile attached to intestinal cells. Reproduced courtesy of Dr Jan Hobot, Cardiff University School of Medicine. Clostridium difficile infection: How to deal with the problem Contents Foreword 1 Scope and purpose 2 Introduction 3 Why did CDI increase? 4 Approach to compiling the guidance 6 What is new in this guidance? 7 Core Guidance Key recommendations 9 Grading of recommendations 11 Summary of healthcare recommendations 12 1. -

Bacillus Cereus Pneumonia
‘Advances in Medicine and Biology’, Volume 67, 2013 Nova Science Publisher Inc., Editor: Berhardt LV To Alessia, my queen, and Giorgia, my princess Chapter BACILLUS CEREUS PNEUMONIA Vincenzo Savini* Clinical Microbiology and Virology, Spirito Santo Hospital, Pescara (PE), Italy ABSTRACT Bacillus cereus is a Gram positive/Gram variable environmental rod, that is emerging as a respiratory pathogen; particularly, pneumonia it causes may be serious and can resemble the anthrax disease. In fact, the organism is strictly related to the famous Bacillus anthracis, with which it shares genotypical, fenotypical, and pathogenic features. Treatment of B. cereus lower airway infections is becoming increasingly hard, due to the spread of multidrug resistance traits among members of the species. Hence, the present chapter’s scope is to shed a light on this bacterium’s lung pathogenicity, by depicting salient microbiological, epidemiological and clinical features it shows. Also, we would like to explore virulence determinants and resistance mechanisms that make B. cereus a life-threatening, potentially difficult-to-treat agent of airway pathologies. * Email: [email protected]. 2 Vincenzo Savini INTRODUCTION The genus Bacillus includes spore-forming species, strains of which are not usually considered to be clinically relevant when isolated from human specimens; in fact, these bacteria are known to be ubiquitously distributed in the environment and may easily contaminate culture material along with improperly handled sample collection devices (Miller, 2012; Brooks, 2001). Bacillus anthracis is the prominent agent of human pathologies within the genus Bacillus, although it is uncommon in most clinical laboratories (Miller, 2012). It is a frank pathogen, as it causes skin and enteric infections; above all, however, it is responsible for a serious lung disease (the ‘anthrax’) that is frequently associated with bloodstream infection and a high mortality rate (Frankard, 2004). -

Biosynthetic Origin of Anthracimycin: a Tricyclic Macrolide from Streptomyces Sp
The Journal of Antibiotics (2016) 69, 403–405 & 2016 Japan Antibiotics Research Association All rights reserved 0021-8820/16 www.nature.com/ja NOTE Biosynthetic origin of anthracimycin: a tricyclic macrolide from Streptomyces sp. Enjuro Harunari1, Hisayuki Komaki2 and Yasuhiro Igarashi1 The Journal of Antibiotics (2016) 69, 403–405; doi:10.1038/ja.2015.118; published online 2 December 2015 Anthracimycin (1) is a decalin-fused tricyclic macrolide isolated from signals arising from the 13C–13C coupling were clearly observed for all terrestrial and marine Streptomyces species (Figure 1).1–3 1 shows the carbons except for three methyl groups (C-23, C-24 and C-25) strong activity against Gram-stain-positive bacteria including Bacillus and C-11 and C-12 (Supplementary Figure S1). The outer split peaks anthracis and methicillin-resistant Staphylococcus aureus (MRSA).3,4 were invisible owing to the roof effect7 caused by the close chemical The most intriguing feature of this molecule is its enantiomerism to shifts between C-11 and C-12 (Δ 0.11 p.p.m.) although these carbons chlorotonil A (2), a secondary metabolite of a myxobacterium are likely derived from a single acetate unit. In the 2D-INADEQUATE 5 1 Sorangium cellulosum (Figure 1). Except for a methyl substitution at spectrum measured with a parameter set optimized for JCC 45 Hz, 13 C-8 in 2, the absolute configurations of the remaining chiral centers at cross peaks derived from the intact C2 acetate units were observed C-2, C-6, C-7, C-12, C-15 and C-16 are opposite between 1 and 2 for C-1/C-2, C-3/C-4, C-5/C-6, C-7/C-8, C-9/C-10, C-13/C-14, C-15/ although the dichrorination at C-4 in 2 is an additional difference C-16, C-17/C-18, C-19/C-20 and C-21/C-22 (Table 1, Supplementary between these compounds. -

Pulmonary Delivery of Biological Drugs
pharmaceutics Review Pulmonary Delivery of Biological Drugs Wanling Liang 1,*, Harry W. Pan 1 , Driton Vllasaliu 2 and Jenny K. W. Lam 1 1 Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, 21 Sassoon Road, Pokfulam, Hong Kong, China; [email protected] (H.W.P.); [email protected] (J.K.W.L.) 2 School of Cancer and Pharmaceutical Sciences, King’s College London, 150 Stamford Street, London SE1 9NH, UK; [email protected] * Correspondence: [email protected]; Tel.: +852-3917-9024 Received: 15 September 2020; Accepted: 20 October 2020; Published: 26 October 2020 Abstract: In the last decade, biological drugs have rapidly proliferated and have now become an important therapeutic modality. This is because of their high potency, high specificity and desirable safety profile. The majority of biological drugs are peptide- and protein-based therapeutics with poor oral bioavailability. They are normally administered by parenteral injection (with a very few exceptions). Pulmonary delivery is an attractive non-invasive alternative route of administration for local and systemic delivery of biologics with immense potential to treat various diseases, including diabetes, cystic fibrosis, respiratory viral infection and asthma, etc. The massive surface area and extensive vascularisation in the lungs enable rapid absorption and fast onset of action. Despite the benefits of pulmonary delivery, development of inhalable biological drug is a challenging task. There are various anatomical, physiological and immunological barriers that affect the therapeutic efficacy of inhaled formulations. This review assesses the characteristics of biological drugs and the barriers to pulmonary drug delivery. -
Towards the Total Synthesis of Anthracimycin
Towards the Total Synthesis of Anthracimycin Giacomo Lodovici Doctor of Philosophy University of York Chemistry January 2019 1. Abstract In 2013 W. Fenical et al. reported the isolation of a natural product from a marine microorganism of streptomyces species, which possessed significant activity against Gram-positive pathogens Bacillus anthracis, methicillin-resistant and vancomycin resistant Staphylococcus aureus (MRSA).15 The compound responsible for the antibiotic activity was found to be the 14-membered macrolide named anthracimycin. The research detailed in this thesis describes the efforts towards the total synthesis of this natural product and specifically the formation of the core of anthracimycin in 12-steps. Direct palladium catalysed oxidation formed the enone used as a dienophile in a stereo- and regio-selective Diels‒Alder/epimerisation sequence, which afforded the trans-decalin. A facial and stereoselective Hosomi‒Sakurai 1,4-addition reaction, followed by a selective borylation/dihydroxylation sequence on the exocyclic alkene, allowed the formation of the core of anthracimycin (Scheme 1). Scheme 1. The formation of the decalin core of anthracimcyin. 1 2. Contents 1. Abstract ............................................................................................................................................... 1 2. Contents .............................................................................................................................................. 2 3. List of Figures ..................................................................................................................................... -

Methicillin-Resistant Staphylococcus Aureus (MRSA)
Methicillin-Resistant Staphylococcus Aureus (MRSA) Over the past several decades, the incidence of resistant gram-positive organisms has risen in the United States. MRSA strains, first identified in the 1960s in England, were first observed in the U.S. in the mid 1980s.1 Resistance quickly developed, increasing from 2.4% in 1979 to 29% in 1991.2 The current prevalence for MRSA in hospitals and other facilities ranges from <10% to 65%. In 1999, MRSA accounted for more than 50% of all Staphylococcus aureus isolates within U.S. intensive care units.3, 4 The past years, however, outbreaks of MRSA have also been seen in the community setting, particularly among preschool-age children, some of whom have attended day-care centers.5, 6, 7 MRSA does not appear to be more virulent than methicillin-sensitive Staphylococcus aureus, but certainly poses a greater treatment challenge. MRSA also has been associated with higher hospital costs and mortality.8 Within a decade of its development, methicillin resistance to Staphylococcus aureus emerged.9 MRSA strains generally are now resistant to other antimicrobial classes including aminoglycosides, beta-lactams, carbapenems, cephalosporins, fluoroquinolones and macrolides.10,11 Most of the resistance was secondary to production of beta-lactamase enzymes or intrinsic resistance with alterations in penicillin-binding proteins. Staphylococcus aureus is the most frequent cause of nosocomial pneumonia and surgical- wound infections and the second most common cause of nosocomial bloodstream infections.12 Long-term care facilities (LTCFs) have developed rates of MRSA ranging from 25%-35%. MRSA rates may be higher in LTCFs if they are associated with hospitals that have higher rates.13 Transmission of MRSA generally occurs through direct or indirect contact with a reservoir. -

125509Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 125509Orig1s000 ADMINISTRATIVE and CORRESPONDENCE DOCUMENTS ACTION PACKAGE CHECKLIST APPLICATION INFORMATION1 If NDA, Efficacy Supplement Type: BLA #125509 BLA Supplement # (an action package is not required for SE8 or SE9 supplements) Proprietary Name: Anthim Applicant: Elusys Therapeutics, Inc. Established/Proper Name: obiltoxaximab Agent for Applicant (if applicable): Dosage Form: injection RPM: Jane A. Dean, RN, MSN Division: Division of Anti-Infective Products For ALL 505(b)(2) applications, two months prior to EVERY action: NDA Application Type: 505(b)(1) 505(b)(2) Efficacy Supplement: 505(b)(1) 505(b)(2) Review the information in the 505(b)(2) Assessment and submit the draft2 to CDER OND IO for clearance. BLA Application Type: 351(k) 351(a) Check Orange Book for newly listed patents and/or Efficacy Supplement: 351(k) 351(a) exclusivity (including pediatric exclusivity) No changes New patent/exclusivity (notify CDER OND IO) Date of check: Note: If pediatric exclusivity has been granted or the pediatric information in the labeling of the listed drug changed, determine whether pediatric information needs to be added to or deleted from the labeling of this drug. Actions Proposed action AP TA CR User Fee Goal Date is 3/20/16 Previous actions (specify type and date for each action taken) None If accelerated approval or approval based on efficacy studies in animals, were promotional materials received? Note: Promotional materials to be used within 120 days after approval must have been Received submitted (for exceptions, see http://www fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guida nces/ucm069965.pdf). -

Characterization of an Endolysin Targeting Clostridioides Difficile
International Journal of Molecular Sciences Article Characterization of an Endolysin Targeting Clostridioides difficile That Affects Spore Outgrowth Shakhinur Islam Mondal 1,2 , Arzuba Akter 3, Lorraine A. Draper 1,4 , R. Paul Ross 1 and Colin Hill 1,4,* 1 APC Microbiome Ireland, University College Cork, T12 YT20 Cork, Ireland; [email protected] (S.I.M.); [email protected] (L.A.D.); [email protected] (R.P.R.) 2 Genetic Engineering and Biotechnology Department, Shahjalal University of Science and Technology, Sylhet 3114, Bangladesh 3 Biochemistry and Molecular Biology Department, Shahjalal University of Science and Technology, Sylhet 3114, Bangladesh; [email protected] 4 School of Microbiology, University College Cork, T12 K8AF Cork, Ireland * Correspondence: [email protected] Abstract: Clostridioides difficile is a spore-forming enteric pathogen causing life-threatening diarrhoea and colitis. Microbial disruption caused by antibiotics has been linked with susceptibility to, and transmission and relapse of, C. difficile infection. Therefore, there is an urgent need for novel therapeutics that are effective in preventing C. difficile growth, spore germination, and outgrowth. In recent years bacteriophage-derived endolysins and their derivatives show promise as a novel class of antibacterial agents. In this study, we recombinantly expressed and characterized a cell wall hydrolase (CWH) lysin from C. difficile phage, phiMMP01. The full-length CWH displayed lytic activity against selected C. difficile strains. However, removing the N-terminal cell wall binding domain, creating CWH351—656, resulted in increased and/or an expanded lytic spectrum of activity. C. difficile specificity was retained versus commensal clostridia and other bacterial species.