Primary Tracheal Squamous Cell Carcinoma - Presenting with Circumferential Invasion and Treated with Photodynamic Therapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Efficacy of Treatment for Primary Tracheal Tumors by Flexible Bronchoscopy: Airway Stenosis Recanalization and Quality of Life
EXPERIMENTAL AND THERAPEUTIC MEDICINE 20: 2099-2105, 2020 Clinical efficacy of treatment for primary tracheal tumors by flexible bronchoscopy: Airway stenosis recanalization and quality of life ZE‑RUI HAO1,2, ZHOU‑HONG YAO1, JING‑QUAN ZHAO3, DE-ZHI LI1, YUN‑YAN WAN1, YAN‑MENG KANG4 and DIAN‑JIE LIN1 1Department of Respiratory Medicine, Shandong Provincial Hospital Affiliated to Shandong University, Jinan, Shandong 250021; 2Department of Respiratory Medicine, The Second People's Hospital of Liaocheng Affiliated to Taishan Medical College, Linqing, Shandong 252601; 3Department of Respiratory Medicine, Beijing Tsinghua Changgung Hospital, Beijing 102218; 4Department of Respiratory Medicine, Qianfo Mountain Hospital, School of Medicine, Shandong University, Jinan, Shandong 250014, P.R. China Received April 10, 2019; Accepted January 6, 2020 DOI: 10.3892/etm.2020.8900 Abstract. The aim of the present study was to evaluate the rate of primary tracheal tumors is approximately one case effectiveness of interventional treatment of primary tracheal per million. Of all tracheal tumors, the rate of malignancy is tumors through flexible bronchoscopy. The clinical data of ~90% in adults and ~30% in children. Tracheal malignancies 38 patients with primary tracheal tumours who underwent account for ~0.2% of all respiratory‑tract cancers and <0.05% flexible bronchoscopy intervention therapy between January of all malignancies (1‑4). Treatments of common tracheal 2011 and January 2017 were retrospectively analyzed. The tumors include surgical resection, radiotherapy and chemo- average time interval from onset of symptoms to the appear- therapy. Surgery has been considered the treatment of choice ance of actual clinical manifestations in the 38 patients ranged for a long time (5). -
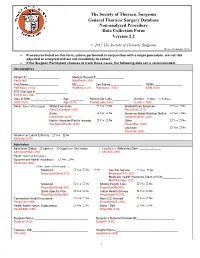
Annotated Non-Analyzed Procedure
The Society of Thoracic Surgeons General Thoracic Surgery Database Non-analyzed Procedure Data Collection Form Version 2.2 © 2012 The Society of Thoracic Surgeons Revised February, 2012 • Procedures listed on this form, unless performed in conjunction with a major procedure, are not risk adjusted or analyzed and are not mandatory to collect. • If the Surgeon Participant chooses to track these cases, the following data set is recommended. Demographics Patient ID: ___________________ Medical Record #:_________________ PatID (80) MedRecN (100) First Name:__________________ MI:_____ Last Name:___________________ SSN#:_________________ PatFName (110) PatMInit (120) PatLName (130) SSN (140) STS Trial Link #:____________________ STSTLink (150) Date of Birth:____/____/______ Age: ________ Patient Zip Code:__________ Gender: Male Female DOB (160) Age (170) PostalCode (180) Gender (190) Race: Select all that apply → White/Caucasian Yes No Black/African American Yes No RaceCaucasian (200) RaceBlack (210) Asian Yes No American Indian/Alaskan Native Yes No RaceAsian (220) RaceNativeAm (230) Native Hawaiian/Pacific Islander Yes No Other Yes No RacNativePacific (240) RaceOther (250) Unknown Yes No RaceUnk (260) Hispanic or Latino Ethnicity: Yes No Ethnicity (270) Admission Admission Status: Inpatient Outpatient / Observation If Inpatient → Admission Date: ____/___/_____ AdmissionStat (280) AdmitDt (290) Payor: Select all that apply ↓ Government Health Insurance: Yes No PayorGov (300) If Yes: Select all that apply: ↓ Medicare Yes No If Yes → Fee For Service: Yes No PayorGovMcare(310) MedicareFFS (320) Medicare Health Insurance Claim (HIC)#:____________ MHICNumber (331) Medicaid Yes No Military Health Care Yes No PayorGovMcaid(340) PayorGovMil(350) State-Specific Plan Yes No Indian Health Service Yes No PayorGovState(360) PayorGovIHS(370) Commercial Health Insurance Yes No Non-U.S. -

Nomograms for Predicting Survival Outcomes in Patients with Primary Tracheal Tumors: a Large Population-Based Analysis
Journal name: Cancer Management and Research Article Designation: Original Research Year: 2018 Volume: 10 Cancer Management and Research Dovepress Running head verso: Wen et al Running head recto: Role of nomograms in primary tracheal tumors open access to scientific and medical research DOI: http://dx.doi.org/10.2147/CMAR.S186546 Open Access Full Text Article ORIGINAL RESEARCH Nomograms for predicting survival outcomes in patients with primary tracheal tumors: a large population-based analysis Junmiao Wen1,2,* Background: The aim of this study was to develop and validate reliable nomograms to predict Di Liu1,2,* individual overall survival (OS) and cancer-specific survival (CSS) for patients with primary tra- Xinyan Xu1,2 cheal tumors and further estimate the role of postoperative radiotherapy (PORT) for these entities. Donglai Chen3 Patients and methods: A total of 405 eligible patients diagnosed between 1988 and 2015 Yongbing Chen4 were selected from the Surveillance, Epidemiology, and End Results database. All of them were randomly divided into training (n 303) and validation (n 102) sets. For the purpose of Liang Sun5 = = establishing nomograms, the Akaike information criterion was employed to select significant Jiayan Chen1,2 prognostic factors in multivariate Cox regression models. Both internal and external validations 1,2 Min Fan of the nomograms were evaluated by Harrell’s concordance index (C-index) and calibration plots. 1 For personal use only. Department of Radiation Oncology, Propensity score matching (PSM) method was performed to reduce the influence of selection Fudan University Shanghai Cancer bias between the PORT group and the non-PORT group. Center, Shanghai 200032, People’s Republic of China; 2Department Results: Two nomograms shared common variables including age at diagnosis, histology, of Oncology, Shanghai Medical N and M stages, tumor size, and treatment types, while gender was only incorporated in the College, Fudan University, Shanghai 200032, People’s Republic of China; CSS nomogram. -

Version 2.41 Training Manual
GENERAL THORACIC SURGERY DATABASE TRAINING MANUAL VERSION 2.41 General Thoracic Surgery Database V2.41 Training Manual November 15, 2018 Table of Contents Case Examples ............................................................................................................................................................3 Definitions ..................................................................................................................................................................4 Demographics .............................................................................................................................................................4 Admission ................................................................................................................................................................ 13 Pre-Operative Evaluation ........................................................................................................................................ 19 Diagnosis (Category of Disease) .............................................................................................................................. 54 Operative ................................................................................................................................................................. 76 Lung Cancer ............................................................................................................................................................ 113 Esophageal Cancer ................................................................................................................................................. -

Fibromyxomaof the Trachea Kazuo Takaoka, Atsuko Satoh, Mikihito Matsuda*, Yasunori Fujioka** and Shoichi Inoue***
CASE REPORT Fibromyxomaof the Trachea Kazuo Takaoka, Atsuko Satoh, Mikihito Matsuda*, Yasunori Fujioka** and Shoichi Inoue*** A 53-year-old male with a small cell carcinoma of the lung was admitted to the Department of Respiratory Diseases, Nikko Memorial Hospital. During bronchofiberoptic examination of the cancer, a small nodule was discovered on the anterior wall of the trachea, about 8 cmbelow the vocal cord. Histopathologically, it was diagnosed as fibromyxoma of the trachea. Primary tumors of the trachea are very rare and fibromyxomaof the trachea is extremely rare. This is only the second report of a fibromyxomaon the tracheal wall. In this report its clinical manifestations were compared with those reported in the first case. (Internal Medicine 32: 895-896, 1993) Key words: benign tumor Case Report cartilage was located in the deeper region. A small amount of fatty tissue was also observed in the loose collagenous tissue. The patient was a 53-year-old male priest. A chest x-ray Anepithelial componentof tumor constitution wasnot recog- revealed a nodular shadow in the right upper lung and enlarge- nized, although hamartoma is composed of non-epithelial and mentof the right hilus suggesting a lung cancer. Computed epithelial components. No malignant findings such as pleo- tomography of the chest also showeda tiny protrusion on the morphismor mitosis were seen. tracheal anterior wall. There was neither tumor infiltration to The final histopathologic diagnosis was made as fibromyxoma the surrounding mediastinum nor a tracheal deformity. Bronchofiberoptic examination (Fig. 1 ) revealed a small hemi- spheric nodule located on the anterior wall of the trachea, approximately 8 cm below the vocal cord. -

Behavior of Primary Tracheal Glomus Tumor, Uncertain Malignant Potential Subtype
General Thoracic and Cardiovascular Surgery (2019) 67:991–995 https://doi.org/10.1007/s11748-019-01085-8 CASE REPORT Behavior of primary tracheal glomus tumor, uncertain malignant potential subtype Yuxing Jin1 · Samer AL Sawalhi1 · Deping Zhao1 · Haomin Cai1 · Ahmad M. Odeh2 · Huikang Xie3 · Jiong Song4 Received: 16 September 2018 / Accepted: 3 February 2019 / Published online: 25 February 2019 © The Japanese Association for Thoracic Surgery 2019 Abstract The behavior of the pathological subtypes of tracheal glomus tumor (benign, uncertain malignant potential UMP, malignant) is vague. In a 51-year-old gentleman, suffering from cough for 4 months, computed tomography scan showed a mass at lower third of the trachea and the bronchoscope revealed exophytic mass at the tracheal lumen. Segmental tracheal resection was done using special modified endotracheal tube for the distal lung ventilation. The tracheal glomus tumor was also diagnosed based on the immunohistochemical staining. The tumor was 2 cm in diameter, deeply located, mitotic phase was difficult to identify, and a diagnosis of UMP subtype was made. There was no recurrence after 2 years follow-up. This is the first reported case of UMP subtype in lower trachea and we studied the treatment options with the clinic-pathological behavior of this tumor and its sequel by regular follow-up. Keywords Glomus tumor · Trachea · Endotracheal intubation Introduction [1]. However, this is the first reported case of UMPS in the lower trachea. Furthermore, this case discussed the clinic- Glomus tumor (GT) is a rare soft tissue neoplasm derived pathological differentiation between carcinoid and tracheal from modified smooth muscle cells of the normal glomus GT, because both of them have shared clinical, radiological body surrounding arteriovenous anastomosis [1]. -

Tracheal Solid Variant of Adenoid Cystic Carcinoma with Basaloid Features: a Case Report and Review of Literature
Tracheal Solid Variant of Adenoid Cystic Carcinoma with Basaloid Features: A Case Report and Review of Literature Feng Gao Shanghai General Hospital Aliated to Shanghai Jiaotong University School of Medicine Department of Pathology Lijuan Zang Shanghai General Hospital Aliated to Shanghai Jiaotong University School of Medicine Department of Pathology Jin He Shanghai General Hospital Aliated to Shanghai Jiaotong University School of Medicine Department of Pathology Weiqing Xu ( [email protected] ) Shanghai First Peoples Hospital Aliated to Shanghai Jiaotong University School of Medicine Department of Pathology https://orcid.org/0000-0002-3639-9338 Case report Keywords: tracheal neoplasm, adenoid cystic carcinoma, clinical pathology, immunohistochemistry, MYB Posted Date: June 8th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-32937/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/11 Abstract Background: Primary tracheal adenoid cystic carcinoma (ACC) is a rare and heterogeneous group of neoplasms arising from the respiratory tract. The solid variant of ACC is a histologically distinct subtype with unfavorable clinical course. We report a case of tracheal ACC with immunohistochemical and molecular analysis together with a review of the literature. Case presentation: A 31-year-old man presented with a neoplasm growing on the lower part of the total tracheal membrane, left side wall and anterior wall. The tumor was obtained via beroptic bronchoscopy. Histologically, the tumor is characterized by a predominant compact sheet-like and nested pattern of rounded basaloid cells. Immunohistochemically, the tumor was diffusely positive for CK and CD117. CK7 and CK5/6 was focally positive in the genuine glandular structures. -

Polyomavirus Jcpyv Infrequently Detectable in Adenoid Cystic Carcinoma of the Oral Cavity and the Airways
Virchows Archiv (2019) 475:609–616 https://doi.org/10.1007/s00428-019-02617-6 ORIGINAL ARTICLE Polyomavirus JCPyV infrequently detectable in adenoid cystic carcinoma of the oral cavity and the airways Hanna Hämetoja1,2 & Jaana Hagström2,3 & Caj Haglund3,4 & Leif Bäck5 & Antti Mäkitie5,6,7 & Stina Syrjänen1 Received: 29 March 2019 /Revised: 13 June 2019 /Accepted: 25 June 2019 /Published online: 1 July 2019 # The Author(s) 2019 Abstract Our objective was to assess the presence of three polyomaviruses, namely SV40, JCPyV, and BKPyV, and human papilloma- viruses (HPV) in adenoid cystic carcinomas (ACC) of the minor salivary glands (MiSG) in the head and neck region. The study comprised 68 MiSG ACC patients operated during 1974–2012 at the Helsinki University Hospital (Helsinki, Finland). Medical records and 68 histological samples were reviewed. Polyomaviruses were detected with quantitative PCR and the DNA-positive samples were further analyzed for the presence of viral tumor T antigen (T-ag) with immunohistochemistry. HPV genotyping was performed with a Multiplex HPV Genotyping Kit. Only JCPyV DNAwas found in ACC samples, being present in 7 (10.3%) out of the 68 samples. The viral load of JCPyV was low varying between 1 to 226 copies/μg DNA. The JCPyV-positive samples originated from trachea (two samples), paranasal sinuses (one), and oral cavity (two). Additionally, JCPyV positivity was found in one lung metastasis of a tracheal tumor and one local disease failure of an oral cavity tumor. Three JCPyV DNA-positive samples showed weak nuclear staining for large T-ag. In conclusion, only JCPyV but not SV40, BKPyV, or HPV was found in ACC from the upper and lower airways. -

Surgical Treatment of Primary Tracheal Tumors in Children and Adolescents
Review Article Page 1 of 7 Surgical treatment of primary tracheal tumors in children and adolescents Lorenzo Giannini1,2, Fabiola Incandela1, Lorenzo Bresciani1, Cesare Piazza1 1Department of Otorhinolaryngology, Maxillofacial, and Thyroid Surgery, Fondazione IRCCS, National Cancer Institute of Milan, University of Milan, Milan, Italy; 2Departmemnt of Otorhinolaryngology-Head and Neck Surgery, ASST Santi Paolo e Carlo, University of Milan, Milan, Italy Contributions: (I) Conception and design: All authors; (II) Administrative support: C Piazza; (III) Provision of study materials or patients: None; (IV) Collection and assembly of data: L Giannini, F Incandela, L Bresciani; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Cesare Piazza, MD. Chief of the Department of Otorhinolaryngology, Maxillofacial, and Thyroid Surgery, Fondazione IRCCS, National Cancer Institute of Milan, University of Milan, 20133 Milan, Italy. Email: [email protected]; [email protected]. Abstract: Pediatric primary tracheal tumors (PTTs) are rare entities, with an estimated incidence of 0.2% among all neoplasms in children and adolescents. Benign lesions and malignancies are rather equally represented, with subglottic hemangioma, granular cell tumor, carcinoid tumor, and low-grade mucoepidermoid carcinoma being the most common histotypes. Guidelines on management and treatment of pediatric PTTs are not available, and only a few reviews, case reports, and single surgeon/institute experiences have been published. A literature search was carried out focusing on the surgical approaches utilized in the most recent publications to manage pediatric PTTs, thus including case reports, single institute experiences, and reviews on surgical techniques. Moreover, we divided the available intervention modalities based on an anatomical classification, distinguishing between laryngotracheal, cervical tracheal, lower tracheal, and carinal scenarios. -

Role of Video-Assisted Thoracic Surgery in T4 NSCLC
11 Review Article Page 1 of 11 Role of video-assisted thoracic surgery in T4 NSCLC Debora Brascia1, Giulia De Iaco1, Marcella Schiavone1, Samuele Nicotra2, Francesca Signore1, Teodora Panza1, Alessandro Geronimo1, Doroty Sampietro1, Giuseppe Marulli1 1Thoracic Surgery Unit, Department of Organ Transplantation and Emergency, University Hospital of Bari, Bari, Italy; 2Thoracic Surgery Unit, Department of Cardiologic, Thoracic and Vascular Sciences, University of Padova, Padova, Italy Contributions: (I) Conception and design: G Marulli, D Brascia; (II) Administrative support: All authors; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Prof. Giuseppe Marulli. Thoracic Surgery Unit, Department of Organ Transplantation and Emergency University Hospital of Bari, Italy. Email: [email protected]; [email protected]. Abstract: For many years, T4 lung tumors have been considered less suitable for surgery, because of their local extension invading central structures or vertebral bodies. To date, many studies have confirmed the advantages in terms of survival of a multimodality approach made up of surgical resection associated with neoadjuvant and/or adjuvant therapy for selected patients with advanced lung cancer. In those patients, in fact, minimally invasive surgery could improve overall survival rates while promoting faster recovery, faster access to adjuvant therapies and preserving a better functionality of the immune system. Because of the difficulty in collecting data on patients with T4 lung tumors amenable to minimally invasive surgery, published evidences only come from case reports which prove the feasibility and the possible advantages of video-assisted thoracic surgery (VATS) procedures. -
Solitary Fibrous Tumor of the Trachea: CT Findings with a Pathological Correlation
Solitary Fibrous Tumor of the Trachea: CT Findings with a Pathological Correlation Young Sup Shim, MD1 We present the multidetector CT findings with a pathologic correlation for the Soo Jin Choi, MD1 case of a solitary fibrous tumor located in the trachea. The MDCT revealed a well- Hyung Sik Kim, MD1 circumscribed intraluminal mass arising from the trachea, with strong nodular Jae Ik Lee, MD2 enhancement in the periphery of the mass. The enhancement pattern of the mass corresponded histopathologically to a focal hypocellular area in the center and prominent blood vessels along the periphery of the mass. We also present volume-rendered and virtual bronchoscopic images of this rare submucosal tra- cheal tumor. rimary benign tumors of the trachea are a rare occurrence, and solitary fibrous tumors (SFTs) that are benign tracheal tumors, are even rarer (1- P 3). SFTs may occur anywhere in the thoracic or extrathoracic region, but generally occur in the pleura and lungs (4). In only extremely rare cases has a SFT of the trachea been reported in the English language clinical literature (2, 3). To the best Index terms: of our knowledge, our report is the first to present clinical evidence of CT findings for Trachea, Neoplasm Solitary fibrous tumor tracheal SFTs with a pathological correlation. Computed tomography (CT) Multidetector-row computed tomography (MDCT) CASE REPORT DOI:10.3348/kjr.2008.9.3.286 A 62-year-old woman with dyspnea, and recent aggravation of the condition 10 days prior, was referred to our institution for further evaluation of the tracheal mass. The woman had no outstanding medical history; however, upon a physical examina- Korean J Radiol 2008;9:286-289 tion, a stridor and wheezing sound was examined by auscultation. -

Enke: Kleintieronkologie
1 Literaturverzeichnis 1 Ätiologie und Pathologie von [21] Cleary MP, Grossmann ME, Ray A: Effect of obesity on breast can- cer development. Vet Pathol. 2010; 47: 202–213 Krebserkrankungen [22] Cruz Cardona JA, Milner R, Alleman AR et al.: BCR-ABL transloca- [1] Ahern TE, Bird RC, Bird AE et al.: Expression of the oncogene tion in a dog with chronic monocytic leukemia. Vet Clin Pathol. – c-erbB-2 in canine mammary cancers and tumor-derived cell lines. 2011; 40: 40 47 Am J Vet Res. 1996; 57: 693–696 [23] De Maria R, Miretti S, Iussich S et al.: met oncogene activation [2] Angres G, Scherf HR, Schmahl D: Tumor heterogeneity and che- qualifies spontaneous canine osteosarcoma as a suitable pre-clinical – mosensitivity to cyclophosphamide, vinblastine and hexadecylphos- model of human osteosarcoma. J Pathol. 2009; 218: 399 408 phocholine. Cancer Treat Rev. 1990; 17: 339–345 [24] de Visser KE, Eichten A, Coussens LM: Paradoxical roles of the immune system during cancer development. Nat Rev Cancer. 2006; [3] Argyle DJ, Nasir L: Pathophysiology of cellular regulation, cell Literaturverzeichnis – death, and cancer. In: Dunlop R.H. and Malbert C.H. (Hrsg.), Veteri- 6: 24 37 nary Pathophysiology. 1. Auflg. Iowa State Press, Ames, Iowa; 2004, [25] de Visser KE: Spontaneous immune responses to sporadic tumors: 25–78 tumor-promoting, tumor-protective or both? Cancer Immunol – [4] Argyle DJ, Blacking T: From viruses to cancer stem cells: dissecting Immunother. 2008; 57: 1531 1539 the pathways to malignancy. Vet J. 2008; 177: 311–323 [26] Dean M, Fojo T, Bates S: Tumour stem cells and drug resistance.