Spindle Cell Sarcomatoid Carcinoma of the Trachea: First Case Report of Surgical Resection Juan P
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sarcomatoid Renal Cell Carcinom Atoid Renal Cell Carcinoma
Research Article Sarcomatoid renal cell carcinoma: A case series K Subashree 1*, M Susruthan 2, N Priyathersini 3, Leena Dennis Joseph 4, Sandhya Sundaram 5 1PG Student, 2,3 Assistant Professor, 4,5 Professor, Department of Pathology , Sri Ramachandra Medical College and Research Institute Porur, Chennai-116, Tamil Nadu, INDIA. Email : [email protected] Abstract Introduction: Renal cell carcinoma is the most common form of Renal malignancy. Sarcomatoid renal cell carcinoma represents a high grade dedifferentiation of Renal cell carcinoma. This phenotype can occur in all subtypes of renal cell carcinomas, including clear cell, papillary, chromophob e, and collecting duct carcinoma. Although prognosis in sarcomatoid renal cell carcinoma is known to be extremely poor, little is known about the clinicopathologic information about them. Methods and Methodology: The population of this retrospective study consisted of all patients who underwent surgery for Renal cell carcinoma between January 2010 and February 2013 in the Department of Pathology, Sri Ramachandra university and Research Institute .A total of 64 renal cell carcinoma cases were diagnosed among which 9 had sarcomatoid changes. All 9 cases were reassessed and the diagnosis was confirmed on the basis of morphologic features. Complete baseline and follow -up data were available for analysis for all 9 patients. Conclusion: Present study showed that s arcomatoid changes were seen more commonly in younger age group with male preponderance and ne crosis was a consistent feature. Sarcomatoid areas constitute 1-25% in majority of cases which makes extensive sampling an important measure. Majority of renal cell carcinomas with sarcomatoid changes ha ve a high grade and high stage. -

Rare Sarcomatoid Carcinoma of the Liver in a Patient with No History of Hepatocellular Carcinoma: a Case Report
Rare sarcomatoid carcinoma of the liver in a patient with no history of hepatocellular carcinoma: a case report Abstract Sarcomatoid carcinoma is a rare malignant tumor of unknown pathogenesis characterized by poorly differentiated carcinoma tissue containing sarcoma-like differentiation of either spindle or giant cell and rarely occurs in the gastrointestinal tract and hepatobiliary-pancreatic system.1 Primary hepatic sarcomatoid carcinoma accounts for only 0.2 % of primary malignant liver tumors, and 1.8% of all surgically resected hepatocellular carcinomas.2 The majority of hepatic sarcomatoid carcinoma cases appear to occur simultaneously with hepatocellular or cholangiocellular carcinoma.3 The preferred treatment for hepatic sarcomatoid carcinoma is surgical resection and the overall prognosis is poor.4 This case depicts a 62-year-old female who underwent initial resection of a cavernous hemangioma in 2010. Seven years after her initial diagnosis, she developed what was initially felt to be local recurrence of the hemangioma but additional diagnostic workup with a liver biopsy confirmed primary hepatic sarcomatoid carcinoma. Keywords Sarcomatoid Carcinoma, Hepatocellular Carcinoma, Primary Hepatic Sarcomatoid Carcinoma Case Report A 62-year-old female with past medical history significant for vegan diet, hypothyroidism, iron deficiency anemia, and cavernous liver hemangioma presented with weight loss and abdominal fullness for approximately one month with two days of acute altered mental status, fatigue, and weakness. Patient had a complicated gastrointestinal history and underwent surgical resection of a cavernous hemangioma in 2010. Six years later, she developed abdominal fullness with right upper quadrant pain and an abdominal ultrasound at that time suggested hemangioma recurrence. In 2017, she underwent laparoscopy with unroofing of the hemangioma, drainage of an old organizing hematoma, removal of debris, and placement of an omental patch. -

Lung Equivalent Terms, Definitions, Charts, Tables and Illustrations C340-C349 (Excludes Lymphoma and Leukemia M9590-9989 and Kaposi Sarcoma M9140)
Lung Equivalent Terms, Definitions, Charts, Tables and Illustrations C340-C349 (Excludes lymphoma and leukemia M9590-9989 and Kaposi sarcoma M9140) Introduction Use these rules only for cases with primary lung cancer. Lung carcinomas may be broadly grouped into two categories, small cell and non-small cell carcinoma. Frequently a patient may have two or more tumors in one lung and may have one or more tumors in the contralateral lung. The physician may biopsy only one of the tumors. Code the case as a single primary (See Rule M1, Note 2) unless one of the tumors is proven to be a different histology. It is irrelevant whether the other tumors are identified as cancer, primary tumors, or metastases. Equivalent or Equal Terms • Low grade neuroendocrine carcinoma, carcinoid • Tumor, mass, lesion, neoplasm (for multiple primary and histology coding rules only) • Type, subtype, predominantly, with features of, major, or with ___differentiation Obsolete Terms for Small Cell Carcinoma (Terms that are no longer recognized) • Intermediate cell carcinoma (8044) • Mixed small cell/large cell carcinoma (8045) (Code is still used; however current accepted terminology is combined small cell carcinoma) • Oat cell carcinoma (8042) • Small cell anaplastic carcinoma (No ICD-O-3 code) • Undifferentiated small cell carcinoma (No ICD-O-3 code) Definitions Adenocarcinoma with mixed subtypes (8255): A mixture of two or more of the subtypes of adenocarcinoma such as acinar, papillary, bronchoalveolar, or solid with mucin formation. Adenosquamous carcinoma (8560): A single histology in a single tumor composed of both squamous cell carcinoma and adenocarcinoma. Bilateral lung cancer: This phrase simply means that there is at least one malignancy in the right lung and at least one malignancy in the left lung. -

Primary Tracheal Squamous Cell Carcinoma - Presenting with Circumferential Invasion and Treated with Photodynamic Therapy
218 Primary Tracheal Squamous Cell Carcinoma - Presenting with Circumferential Invasion and Treated with Photodynamic Therapy Lih-Yu Chang*, Sheng-Kai Liang**, Chia-Lin Hsu*, Jang-Ming Lee***, Chong-Jen Yu* Primary neoplasms of the trachea are extremely rare. The diagnosis usually depends on computed tomography (CT) scan. We report a 50-year-old woman who suffered from chronic productive cough for 1 year. Roentgenograms and chest CT showed no abnormal finding. Bronchoscopy showed diffuse circumferential papilloma-like lesions at the trachea. Endobronchial ultrasound showed submucosal invasion of the trachea. The pathology of the endotracheal biopsy showed squamous cell carcinoma. She received photodynamic therapy as first-line treatment with a good response and tumor regression. (Thorac Med 2014; 29: 218-223) Key words: squamous cell carcinoma, tracheal tumor, bronchoscopy, endobronchial ultrasound, photodynamic therapy Introduction agnosis of tracheal tumor and evaluation of the relationship between the surrounding tissue and Primary tracheal tumors are rare, and are organs [1]. Pulmonary function test may show usually malignant in adults (80-90%) and be- fixed upper airway obstruction [1]. Bronchos- nign in children (60-70%) [1-2]. Clinical pre- copy is used for tissue sampling and assessment sentations include dyspnea (58%), cough (54%), of the location and extent of the disease [1]. hemoptysis (45%), wheezing (36%) and stri- In previous reports, tracheal tumor almost dor (24%) [3]. Diagnosis is often delayed for always presented with a protruding mass and months due to initial misdiagnosis as asthma, could be easy diagnosed by chest CT. We pres- chronic obstructive airway disease, or chronic ent a case of primary tracheal squamous cell bronchitis. -

Clinical Efficacy of Treatment for Primary Tracheal Tumors by Flexible Bronchoscopy: Airway Stenosis Recanalization and Quality of Life
EXPERIMENTAL AND THERAPEUTIC MEDICINE 20: 2099-2105, 2020 Clinical efficacy of treatment for primary tracheal tumors by flexible bronchoscopy: Airway stenosis recanalization and quality of life ZE‑RUI HAO1,2, ZHOU‑HONG YAO1, JING‑QUAN ZHAO3, DE-ZHI LI1, YUN‑YAN WAN1, YAN‑MENG KANG4 and DIAN‑JIE LIN1 1Department of Respiratory Medicine, Shandong Provincial Hospital Affiliated to Shandong University, Jinan, Shandong 250021; 2Department of Respiratory Medicine, The Second People's Hospital of Liaocheng Affiliated to Taishan Medical College, Linqing, Shandong 252601; 3Department of Respiratory Medicine, Beijing Tsinghua Changgung Hospital, Beijing 102218; 4Department of Respiratory Medicine, Qianfo Mountain Hospital, School of Medicine, Shandong University, Jinan, Shandong 250014, P.R. China Received April 10, 2019; Accepted January 6, 2020 DOI: 10.3892/etm.2020.8900 Abstract. The aim of the present study was to evaluate the rate of primary tracheal tumors is approximately one case effectiveness of interventional treatment of primary tracheal per million. Of all tracheal tumors, the rate of malignancy is tumors through flexible bronchoscopy. The clinical data of ~90% in adults and ~30% in children. Tracheal malignancies 38 patients with primary tracheal tumours who underwent account for ~0.2% of all respiratory‑tract cancers and <0.05% flexible bronchoscopy intervention therapy between January of all malignancies (1‑4). Treatments of common tracheal 2011 and January 2017 were retrospectively analyzed. The tumors include surgical resection, radiotherapy and chemo- average time interval from onset of symptoms to the appear- therapy. Surgery has been considered the treatment of choice ance of actual clinical manifestations in the 38 patients ranged for a long time (5). -

Sarcomatoid Urothelial Carcinoma Arising in the Female Urethral Diverticulum
Journal of Pathology and Translational Medicine 2021; 55: 298-302 https://doi.org/10.4132/jptm.2021.04.23 CASE STUDY Sarcomatoid urothelial carcinoma arising in the female urethral diverticulum Heae Surng Park Department of Pathology, Ewha Womans University Seoul Hospital, Seoul, Korea A sarcomatoid variant of urothelial carcinoma in the female urethral diverticulum has not been reported previously. A 66-year-old woman suffering from dysuria presented with a huge urethral mass invading the urinary bladder and vagina. Histopathological examination of the resected specimen revealed predominantly undifferentiated pleomorphic sarcoma with sclerosis. Only a small portion of conven- tional urothelial carcinoma was identified around the urethral diverticulum, which contained glandular epithelium and villous adenoma. The patient showed rapid systemic recurrence and resistance to immune checkpoint inhibitor therapy despite high expression of pro- grammed cell death ligand-1. We report the first case of urethral diverticular carcinoma with sarcomatoid features. Key Words: Sarcomatoid carcinoma; Urothelial carcinoma; Urethral diverticulum Received: March 9, 2021 Revised: April 16, 2021 Accepted: April 23, 2021 Corresponding Author: Heae Surng Park, MD, PhD, Department of Pathology, Ewha Womans University Seoul Hospital, Ewha Womans University College of Medicine, 260 Gonghang-daero, Gangseo-gu, Seoul 07804, Korea Tel: +82-2-6986-5253, Fax: +82-2-6986-3423, E-mail: [email protected] Urethral diverticular carcinoma (UDC) is extremely rare; the urinary bladder, and vagina with enlarged lymph nodes at both most common histological subtype is adenocarcinoma [1,2]. femoral, both inguinal, and both internal and external iliac areas Sarcomatoid urothelial carcinoma (UC) is also unusual. Due to (Fig. 1B). -

Primary Cutaneous Carcinosarcoma: a Case Report and Discussion of a Histological “Chimera”
Primary Cutaneous Carcinosarcoma: A Case Report and Discussion of a Histological “Chimera” Joseph Dyer, DO,* Kaylan Pustover, DO,** Prasanna Sinkre, MD,*** Richard Miller, DO, FAOCD**** *Dermatology Resident, 1st year, Largo Medical Center, Largo, FL **PGY-1, Largo Medical Center, Largo, FL ***Dermatopathologist, Cockerell Dermatopathology, Dallas, TX ****Dermatology Residency Program Director, Largo Medical Center, Largo, FL Abstract Primary cutaneous carcinosarcoma is a rare and aggressive biphasic malignant neoplasm that exhibits both epithelial and mesenchymal components. This malignancy is more commonly described arising from organs such as the uterus, breast, bladder, and lung, and is rarely seen on the skin. The histopathogenesis of this neoplasm is unknown, but a prevailing divergence theory exists. It is imperative that this neoplasm be diagnosed and treated, as it can be fatal. Here we report a case of primary cutaneous carcinosarcoma presenting on the skin of an 86-year-old male. Introduction carcinoma. The mesenchymal component may be Immunohistochemical stains are important for Primary cutaneous carcinosarcoma (PCC) is of osseous, cartilaginous or, more rarely, skeletal- the diagnosis of carcinosarcoma. Cytokeratin or smooth-muscle lineage.5 highlights the epithelial elements, while vimentin a rare neoplasm not commonly found on the 1 skin. To our knowledge, fewer than 100 cases Although the histopathogenesis of PCC is highlights the mesenchymal elements. Two 1 of PCC have been reported in world literature. unknown, there are two common theories at studies emphasize the role of p63, a homologue Carcinosarcoma is most often observed in organs present. The prevailing hypothesis, also known of the tumor suppressor gene p53, in confirming epithelial derivation of poorly differentiated or other than the skin including the uterus, breast, as the divergence or monoclonal hypothesis, 6,7 1,2 It is thought that p63 is urinary bladder, and lungs. -

Case Report Rare Sarcomatoid Liver Carcinoma Composed of Atypical Spindle Cells Without Features of Either HCC Or ICC: a Case Report
Int J Clin Exp Med 2016;9(10):20308-20313 www.ijcem.com /ISSN:1940-5901/IJCEM0033483 Case Report Rare sarcomatoid liver carcinoma composed of atypical spindle cells without features of either HCC or ICC: a case report Kazushige Nirei1, Shunichi Matsuoka1, Mitsuhiko Moriyama1, Hitomi Nakamura1, Toshiya Maebayashi2, Tadatoshi Takayama3, Masahiko Sugitani4 1Division of Gastroenterology and Hepatology, Department of Internal Medicine, 2Department of Radiology, 3Department of Digestive Surgery, 4Department of Pathology, Nihon University School of Medicine, Tokyo, Japan Received November 14, 2015; Accepted September 4, 2016; Epub October 15, 2016; Published October 30, 2016 Abstract: The patient was a 68-year-old male with a history of chemotherapy for malignant lymphoma which had achieved a complete remission. As he was infected with the hepatitis C virus, he was followed periodically, and 7 years after chemotherapy completion computed tomography revealed a 51 mm-in-diameter tumor in the right lobe of the liver. F-Fluorodeoxyglucose positron emission tomography with computed tomography showed a maximum standardized uptake value of 14.6. The patient had no history of transcatheter arterial chemoembolization, percu- taneous ethanol injection therapy or radiofrequency ablation. The alfa fetoprotein level was 5.9 ng/ml. Malignant lymphoma recurrence was thus suspected. The tumor was surgically resected and examined. There was no patho- logical evidence of malignant lymphoma. The entire tumor area was composed of atypical spindle cells with no components of either hepatocellular carcinoma or intrahepatic cholangiocarcinoma. Immunohistochemically, the tumor cells were diffusely positive for cytokeratin 7 and vimentin, indicating a poorly differentiated carcinoma. The appearance of the adjacent liver parenchyma was consistent with chronic hepatitis. -
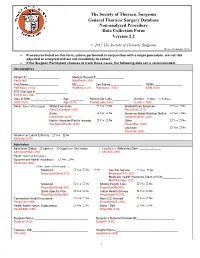
Annotated Non-Analyzed Procedure
The Society of Thoracic Surgeons General Thoracic Surgery Database Non-analyzed Procedure Data Collection Form Version 2.2 © 2012 The Society of Thoracic Surgeons Revised February, 2012 • Procedures listed on this form, unless performed in conjunction with a major procedure, are not risk adjusted or analyzed and are not mandatory to collect. • If the Surgeon Participant chooses to track these cases, the following data set is recommended. Demographics Patient ID: ___________________ Medical Record #:_________________ PatID (80) MedRecN (100) First Name:__________________ MI:_____ Last Name:___________________ SSN#:_________________ PatFName (110) PatMInit (120) PatLName (130) SSN (140) STS Trial Link #:____________________ STSTLink (150) Date of Birth:____/____/______ Age: ________ Patient Zip Code:__________ Gender: Male Female DOB (160) Age (170) PostalCode (180) Gender (190) Race: Select all that apply → White/Caucasian Yes No Black/African American Yes No RaceCaucasian (200) RaceBlack (210) Asian Yes No American Indian/Alaskan Native Yes No RaceAsian (220) RaceNativeAm (230) Native Hawaiian/Pacific Islander Yes No Other Yes No RacNativePacific (240) RaceOther (250) Unknown Yes No RaceUnk (260) Hispanic or Latino Ethnicity: Yes No Ethnicity (270) Admission Admission Status: Inpatient Outpatient / Observation If Inpatient → Admission Date: ____/___/_____ AdmissionStat (280) AdmitDt (290) Payor: Select all that apply ↓ Government Health Insurance: Yes No PayorGov (300) If Yes: Select all that apply: ↓ Medicare Yes No If Yes → Fee For Service: Yes No PayorGovMcare(310) MedicareFFS (320) Medicare Health Insurance Claim (HIC)#:____________ MHICNumber (331) Medicaid Yes No Military Health Care Yes No PayorGovMcaid(340) PayorGovMil(350) State-Specific Plan Yes No Indian Health Service Yes No PayorGovState(360) PayorGovIHS(370) Commercial Health Insurance Yes No Non-U.S. -

Sarcomatoid Squamous Cell Carcinoma of Pharynx: a Case Report with Immunohistochemical Study
http://crcp.sciedupress.com Case Reports in Clinical Pathology 2016, Vol. 3, No. 2 CASE REPORT Sarcomatoid squamous cell carcinoma of pharynx: A case report with immunohistochemical study Tadashi Terada∗ Department of Pathology, Shizuoka City Shimizu Hospital, Shizuoka, Japan Received: December 28, 2015 Accepted: January 29, 2016 Online Published: March 15, 2016 DOI: 10.5430/crcp.v3n2p39 URL: http://dx.doi.org/10.5430/crcp.v3n2p39 ABSTRACT Primary sarcomatoid squamous cell carcinoma (S-SCC) of pharynx is a very rare tumor. A 77-year-old woman presented with sore throat. Laryngoscope revealed an infiltrating tumor of lower pharynx. The tumor was ulcerated and measured 3 cm × 4 cm × 3 cm. The tumor was invasive and involved the surrounding tissues. Biopsies showed sarcomatous malignant spindle cell proliferation as well as invasive well-differentiated squamous cell carcinoma (SCC). The former occupied 80% and the latter 20%. Gradual transitions between malignant spindle cells and SCC were frequently seen. The histological diagnosis was S-SCC. Immunohistochemically (the results are shown in Table 1), the tumor cells were positive for vimentin, cytokeratin (CK) AE1/3, CK CAM5.2, CK WSS, CK KL-1, CK MNF-15, CK5, CK6, CK7, CK8, CK 18, CK19, p53 and Ki67 (labeling index = 65%), but negative for CK34BE12, CK20, EMA, S100 protein, NSE, NCAM, synaptophysin, chromogranin, desmin, α-smooth muscle actin, smooth muscle actin (HHF-35), h-caldemon, CD31, factor VIII-related antigen, CD34, HMB45, KIT, PDGFRA, CA19-9, CEA, bcl-2, CD3, CD20, CD45, CD138, myoglobin, HPV, and EBER. The author’s diagnosis was S-SCC. The patient received chemotherapy and radiation, and is now in complete remission 3 years after the diagnosis. -

Sarcomatoid Differentiation in Renal Cell Carcinoma: Prognostic Implications Marcos F
Clinical Urology SARCOMATOID DIFFERENTIATION IN RCC International Braz J Urol Vol. 31 (1): 10-16, January - February, 2005 Official Journal of the Brazilian Society of Urology SARCOMATOID DIFFERENTIATION IN RENAL CELL CARCINOMA: PROGNOSTIC IMPLICATIONS MARCOS F. DALL’OGLIO, MARCO LIEBERKNECHT, VALTER GOUVEIA, ALEXANDRE C. SANT’ANNA, KATIA R. LEITE, MIGUEL SROUGI Division of Urology, Paulista School of Medicine, Federal University of Sao Paulo, UNIFESP, Sao Paulo, SP, Brazil ABSTRACT Introduction: Renal cell carcinoma with sarcomatoid differentiation is a tumor with aggres- sive behavior that is poorly responsive to immunotherapy. The objective of this study is to report our experience in the treatment of 15 patients with this tumor. Materials and Methods: We retrospectively analyzed 15 consecutive cases of renal cell car- cinoma with sarcomatoid differentiation diagnosed between 1991 and 2003. The clinical presentation and the pathological stage were assessed, as were the tumor’s pathological features, use of adjuvant immunotherapy and survival. The study’s primary end-point was to assess survival of these individu- als. Results: The sample included 8 women and 7 men with mean age of 63 years (44 - 80); follow-up ranged from 1 to 100 months (mean 34). Upon presentation, 87% were symptomatic and 4 individuals had metastatic disease. Mean tumor size was 9.5 cm (4 - 24) with the following pathologi- cal stages: 7% pT1, 7% pT2, 33% pT3, and 53% pT4. The pathological features showed high-grade tumors with tumoral necrosis in 87% of the lesions and 80% of intratumoral microvascular invasion. Disease-free and cancer-specific survival rates were 40 and 46% respectively, with 2 cases respond- ing to adjuvant immunotherapy. -

Oncologic Outcome and Potential Prognostic Factors in Primary Squamous Cell Carcinoma of the Parotid Gland Qigen Fang1* , Junfu Wu1 and Fei Liu2
Fang et al. BMC Cancer (2019) 19:752 https://doi.org/10.1186/s12885-019-5969-6 RESEARCHARTICLE Open Access Oncologic outcome and potential prognostic factors in primary squamous cell carcinoma of the parotid gland Qigen Fang1* , Junfu Wu1 and Fei Liu2 Abstracts Background: Primary parotid squamous cell carcinoma (SCC) is an uncommon tumour, and there is limited data on its prognosis and treatment. The goal of the current study was to analyse the potential prognostic factors and clinical outcomes for this tumour type. Methods: Consecutive patients with surgically treated primary parotid SCC were retrospectively enrolled in this study. The primary end point was locoregional control (LRC) and disease-specific survival (DSS), which were calculated by the Kaplan-Meier method. Independent prognostic factors were evaluated by the Cox proportional hazards method. Results: In total, 53 patients were included for analysis. Perineural and lymphovascular invasion were observed in 21 and 16 patients, respectively. Intraparotid node (IPN) metastasis was reported in 23 patients with an incidence rate of 43.3%. Twenty-six patients with cN0 disease underwent neck dissection, and pathologic node metastasis was observed in 10 cases. The 5-year LRC and DS S rates were 35 and 49%, respectively. The Cox model was used to report the independence of disease stage and IPN metastasis in predicting LRC and the independence of disease stage and perineural invasion in predicting DSS. Conclusions: The prognosis of primary parotid SCC is relatively unfavourable. IPN metastasis significantly decreases disease control, disease stage is the most important prognostic factor, and neck dissection is suggested for patients at any stage.