Year in Review 2018
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Whiteness and Civility: White Racial Attitudes in the Concho Valley, 1869-1930
WHITENESS AND CIVILITY: WHITE RACIAL ATTITUDES IN THE CONCHO VALLEY, 1869-1930 A Thesis Presented to the Faculty of the College of Graduate Studies of Angelo State University In Partial Fulfillment of the Requirements for the Degree MASTER OF ARTS by MATTHEW SCOTT JOHNSTON August 2015 Major: History WHITENESS AND CIVILITY: WHITE RACIAL ATTITUDES IN THE CONCHO VALLEY, 1869-1930 by MATTHEW SCOTT JOHNSTON APPROVED: Dr. Jason Pierce, Ph. D. Dr. Kenneth Heinemann, Ph. D. Dr. Kanisorn Wongsrichanalai, Ph.D. Dr. Cheryl Stenmark, Ph.D August 2015 APPROVED: Dr. Susan E. Keith Dean of the College of Graduate Studies ABSTRACT Implicit in the ideology of White Supremacy is the idea of moral supremacy over non-white peoples. However, in the late nineteenth and early twentieth century whites consistently crossed the blurry, racialized line that defined them by what they were not. In the west-central Texas region of the Concho Valley, breaching law and order and social mores condemned some whites to lose degrees of whiteness in the eyes of their peers. Some whites appeared hypocritical in their rebuke of racial terrorism. In the late nineteenth and early twentieth century many white West Texans became guilty of the very lawless and violent attributes they generally applied to those of a different skin color, thus exposing the schizophrenic and ambiguous nature of the notion of white supremacy. iii TABLE OF CONTENTS Page ABSTRACT……………………………………………………………………………….....iii TABLE OF CONTENTS…......................................................................................................iv INTRODUCTION….................................................................................................................1 CHAPTER I. AFTER JUNTEENTH: RACE AND WHITE SUPREMACY IN POSTBELLUM TEXAS………………………………………………………………………………………..7 II. WHITE SUPREMACY IN THE CONCHO COUNTRY, 1867-1900…................18 III. -

History Newsletter
NEWSLETTER FOR ALUMNI AND FRIENDS, DEPARTMENT OF HISTORY, UNIVERSITY OF ARKANSAS, FAYETTEVILLE HISTORY NEWSLETTER ISSUE NO. XXXV, 2006-2007 tle, but also came to us since forgiven Dr. Pierce and promises very well fitted to teach to send him to the Ivory Coast just as labor history. Pierce soon as it can. earned his Ph.D. at the With the expertise he has devel- Ohio State University in oped in Arkansas history, Mike Pierce 1999, having written a seems poised to finally make good on dissertation on industrial David Y. Thomas’s call in the very first labor and American issue of the Arkansas Historical Quarterly Populism. That work has (1942) for “research in the history of developed into a meaty labor” in the state. He has already em- manuscript, “The Plow barked on a fascinating project centered and Hammer: Organized on Fort Smith. But even more than Labor, Farmers, and the that, colleagues look forward to Dr. Populist Party in Ohio,” Pierce and Tricia Starks doing the currently under consid- Sonny and Cher thing at department eration by a major schol- meetings. “Babe…..” arly press. He has pub- lished essays in Labor THE NEW TEAM History and Agricultural History, and in History of Dan Sutherland has an elaborate Law in Ohio (2004), ed- baseball analogy for what’s going on in Michael C. Pierce ited by Michael Les the History Department. It measures Benedict and John Winkler. Pierce co- various aspects of our professional lives edited, with Warren Van Tine, Builders of WE LIKE MIKE to the third decimal point, arriving Ohio: A Biographical History (2003), and co- ultimately at such statistics as Esoteric authored, with Van Tine, C.J. -

Melophobe Months 2012 Music Reviews
Melophobe Months 2012 Music Reviews Walter Biggins This is issue #6 of Afronaut. Published by Afronaut Press, February 2013. Text and design © 2013 Walter Biggins. The following issues are available at Quiet Bubble (http://quietbubble.wordpress.com/zines/): Demo Tapes: Essays by Walter Biggins, 2005-2010 (issues #4 & 5, May 2011). A Tribute to Whitney Balliett (issue #3, October 2010). The Patter of Raindrops: The Wonderful Worlds of Hayao Miyazaki (issue #2, February 2010). Letters to Mr. Konigsberg (issue #1, October 2009). Muñeco: A 24-Hour Comic (issue #0, November 2000). For more information, please contact me at [email protected] or check out my blog: quietbubble.wordpress.com. Introduction. Something’s happened to me over the last five years. I listen to, and trust, pop music far less than I did in my twenties, and the pop that I still listen to is radically different than what I grew up with. My ears cock, like a cat’s, more toward jazz, avant-garde, and instrumental hip-hop now than to the rock, rap, R&B, and beat-driven fare that sustained me for twenty years. To be fair, jazz was always there, ever since I bought a $20 CD of Miles Davis’s Capitol/Blue Note years in a cold January morning in 1994. I bought it from Sound Warehouse, a chain that’s long gone, because the cover was cool and Davis—with his close-cropped hair and natty suit—looked cooler than I could ever hope for. It was a sophistication to aspire toward, and to try and impress girls with. -

The Abbey Message
The Abbey Subiaco Message Abbey “...likened to the Son of God, He continues a priest forever.” day thou shalt be with me in paradise.” Christ our Eternal High Priest is further by Mr. Clare Wolf The penitent thief was justified by obscured by the unique way in which Ed. Note: Mr. Clare Wolf, a pioneer divine grace given to him personally and the priestly work of Christ is carried on in the field of Catholic lay evangelism, directly by the dying Redeemer. This through the Church. When we assist at died this past January 6 at his home in was an instance in which the God-man the Holy Sacrifice we do not have any Prairie View. During the 1960s and 70s, personally and directly bestowed the doubt that at the words of Consecra- he was a highly-regarded speaker, teacher, sanctifying grace of God on another tion the bread and wine become the and writer on theological topics in the member of the human race. During Body and Blood of Jesus Christ, just as Subiaco Deanery, in the Diocese of Little His public ministry Christ discharged truly as they did when Christ Himself Rock, and beyond. He was a frequent both of the functions of a priest. spoke the consecrating words at the Last contributor to The Abbey Message. In But, the Christ of history is no Supper. Nor do we doubt that when we his honor, we reprint one of his articles of longer visible among us. He has have contritely confessed our sins to the June 1962. -

Off-Beats and Cross Streets: a Collection of Writing About Music, Relationships, and New York City
University of Southern Maine USM Digital Commons Stonecoast MFA Student Scholarship 2020 Off-Beats and Cross Streets: A Collection of Writing about Music, Relationships, and New York City Tyler Scott Margid University of Southern Maine, [email protected] Follow this and additional works at: https://digitalcommons.usm.maine.edu/stonecoast Recommended Citation Margid, Tyler Scott, "Off-Beats and Cross Streets: A Collection of Writing about Music, Relationships, and New York City" (2020). Stonecoast MFA. 135. https://digitalcommons.usm.maine.edu/stonecoast/135 This Open Access Thesis is brought to you for free and open access by the Student Scholarship at USM Digital Commons. It has been accepted for inclusion in Stonecoast MFA by an authorized administrator of USM Digital Commons. For more information, please contact [email protected]. Off-Beats and Cross-Streets: A Collection of Writing about Music, Relationships, and New York City A THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUTREMENTS FOR THE DEGREE OF MASTER OF FINE ARTS, UNIVERSITY OF SOUTHERN MAINE, STONECOAST MFA IN CREATIVE WRITINC BY Tyler Scott Margid 20t9 THE UNIVERSITY OF SOUTHERN MAINE STONECOAST MFA IN CREATIVE WRITING November 20,2019 We hereby recommend that the thesis of Tyler Margid entitled OffÙeats and Cross- Streets be accepted as partial fulfillment of the requirements for the Degree of Master of Fine Arts Advisor Florio -'1 4rl:ri'{" ¡ 'l¡ ¡-tÁ+ -- Reader Debra Marquart Director J Accepted ¿/k Dean, College of Arts, Humanities, and Social Sciences Adam-Max Tuchinsky At¡stract Through a series of concert reviews, album reviews, and personal essays, this thesis tracks a musical memoir about the transition from a childhood growing up in a sheltered Connecticut suburb to young adulthood working in New York City, discovering relationships and music scenes that shape the narrator's senss of identity as well the larger culture he f,rnds himself in. -

The Hyphenated Norwegian
VESTERHEIM IN RED, WHITE AND BLUE: THE HYPHENATED NORWEGIAN- AMERICAN AND REGIONAL IDENTITY IN THE PACIFIC NORTHWEST, 1890-1950 By HANS-PETTER GRAV A dissertation submitted in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY WASHINGTON STATE UNIVERSITY Department of History MAY 2018 © Copyright by HANS-PETTER GRAV, 2018 All Rights Reserved © Copyright by HANS-PETTER GRAV, 2018 All Rights Reserved To the Faculty of Washington State University: The members of the Committee appointed to examine the dissertation of HANS-PETTER GRAV find it satisfactory and recommend that it be accepted. LAURIE MERCIER, Ph.D., Chair ROBERT BAUMAN, Ph.D. JEFFREY SANDERS, Ph.D. LUZ MARIA GORDILLO, Ph.D. ii ACKNOWLEDGMENTS This dissertation has been many years in the making. It all began in 2004 at Pacific Lutheran University in Tacoma, Washington. Chandra Manning, Gina Hames, Carlton Benson, and Beth Kraig instilled in me a desire to pursue history as a profession. I completed a second major in history during the course of one academic year, and I do not believe I could have done it that quickly without the encouragement of Chuck Nelson and David Gerry at the Office of International Student Services. Important during my time at PLU was also the support of Helen Rogers, a close friend and an experienced history major. While my interest in Norwegian Americans’ relationship with Norway and Norwegian culture began during my time at PLU, it was during my years pursuing a Master’s degree at Montana State University in Bozeman that this project began to take shape. -

Dog Title Dog Name Owners Name Champion CH Abfab Ura Neap To
Dog Title Dog Name Owners Name Capt. Tim Egenrieder & Lesley Early & Jess Champion CH Abfab Ura Neap To Spring Witchey Champion CH Ammardan's Griffon At Folly Hill Darby Lewes & Jennifer Gray Champion CH Bayshore Avatar Bases Loaded Susan Devaux Champion CH Borderfame Tridntru At Hotshot Heidi Laskowski Champion CH Companion's Reasons To Believe Renea Windley Champion CH Fallon's Home Run Duffy O'Tahoe PT Gary Hankoff Champion CH Holly Creek Appalachian Dance David Thomas & Donna P Thomas Champion CH Jbk Cowboy Outlaw Jodie Keener Champion CH Jbk Secret Crown Jewels Jodie Keener Champion CH Jule Too Fairy Of Enchantment Mitzi Tinaglia & Lisa Schneider Champion CH Korsakov's You'Ve Got Mail! Jane M Bishop Champion CH Love's Twilight Companion RN CGC Gail Hollon Champion CH Mccidos Ace Up My Sleeve CGC Janet Bruner Champion CH Mi-Ken's I Herd Ewe Mrs. Michelle Davis Champion CH Pawcific It Takes Hope Emily Barnhart & Kristy Bister Champion CH Shoreland's Golden Star In Texas Kim Crick Champion CH Sportingfields On The Loose At Angrelor RN Anna Lorenz & Dionne Butt-Einck Champion CH Tenja's Ewe Otter Be Envious RN CGC Crystal Mackie & Tera Majors Champion CH Triskles First Tracks Of Dalbrian Ms. Britt I. Haley Grand Champion GCH CH Arcane's On Ruby Wings Kendra Hayes & Kelly Hayes Grand Champion GCH CH Ariel Linwald Eibhlin A Ruan PT FDC OA OAJ OF Mary P Ezzo V.M.D & Linda J Dietrich Grand Champion GCH CH Echowyn Testla Eye Of The Storm CGC Holly H Brown & Paula J Holcomb Grand Champion GCH CH Harbormist Soaring Like A Hot Shot Dorothy Yarberry Grand Champion GCH CH Hot Shot Wrapped Around Your Finger NA NAJ Julie Smarney & Heidi Laskowski Grand Champion GCH CH Outburst Sequel To Passion VICTORIA LEE SCOFIELD Mrs. -
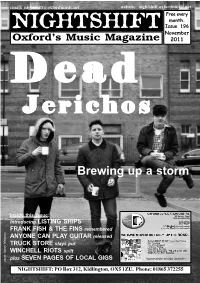
Issue 196.Pmd
email: [email protected] website: nightshift.oxfordmusic.net Free every month. NIGHTSHIFT Issue 196 November Oxford’s Music Magazine 2011 DeadDeadDead JerichosJerichosJerichos Brewing up a storm Inside this issue: Introducing LISTING SHIPS FRANK FISH & THE FINS remembered ANYONE CAN PLAY GUITAR released TRUCK STORE stays put WINCHELL RIOTS split plus SEVEN PAGES OF LOCAL GIGS photo: Sonny Malhotra NIGHTSHIFT: PO Box 312, Kidlington, OX5 1ZU. Phone: 01865 372255 NEWNEWSS Nightshift: PO Box 312, Kidlington, OX5 1ZU Phone: 01865 372255 email: [email protected] Online: nightshift.oxfordmusic.net TRUCK STORE is staying put for the foreseeable future. Having reported last month that it was due to up sticks from its Cowley Road home and reopen in Gloucester Green, owners Rapture have had a change of heart. Explaining the decision to stay put, manager Carl Smithson posted the following ANYONE CAN PLAY GUITAR gets its official release this month. The statement on the shop’s Facebook film, produced and directed by Jon Spira (pictured) tells the story of Oxford’s WINCHELL RIOTS have split up. page: “It’s been something of a music scene from the early-1980s through to 2007 and the closure of the The local indie rock faves issued a rollercoaster few weeks here at Zodiac and features interviews with Ride, Radiohead, Supergrass and Foals statement through the band’s website Truck Store with lots of statements along with members of other Oxford bands and characters who helped create where singer Phil McMinn explained and press going out giving the local scene over the years. Comedian Stewart Lee narrates the story. -

MUSICAL FAMILY TREE and Get It Set up As a Proper Database
Who’s behind this? What’s up with Musicalfamilytree.com? The site was started by Jeb Banner one winter night in early 2004. he ran it off his home The site is a free archive of 1000’s of MP3’s by mostly Indie rock bands that are also computer for the first 9 months. Later Joe Downey got on board to help re-design the site mostly from Indiana. Basically it all started as a way for a group of friends who origi- MUSICAL FAMILY TREE and get it set up as a proper database. Chris Menkhaus is our loyal live show archivist nally met in Bloomington, Indiana back in the mid-1990s to share their music. Everyone had and all around great guy. Also Jenny Banner, Eric Cox, Jake Petroff and PJ Christie help these cassette tapes, DAT’s and a hand full of CD’s and we needed a communal environ- out in many ways. ment where it could all be documented and appreciated by others. Over time it has grown DELICIOUS BERRIES Margot and the Nuclear So and So’s, Everything, Now!, from a couple dozen bands to over 200. We have also followed our friends as they have VOLUME Compiled and Notes by Jeb Banner, Mastered by Carl Saff (saffmastering.com), Cover Art moved around the country, made music with new friends and then we get their friends on Mysteries of Life, John Strohm, marmoset, bigbigcar, by Jason Pierce of Mperfect Design (mperfectdesign.com). Thanks to Jason pierce and Todd the site and so on. -

Sit Down and Shut up Sit Down and Shut Up
Sit Down and Shut Up Sit Down and Shut Up Punk Rock Commentaries on Buddha, God, Truth, Sex, Death,and Dogen’s Treasury of the Right Dharma Eye Brad Warner New World Library Novato, California New World Library 14 Pamaron Way Novato, California 94949 Copyright © 2007 by Brad Warner All rights reserved. This book may not be reproduced in whole or in part, stored in a retrieval system, or transmitted in any form or by any means — electronic, mechanical, or other — without written permission from the publisher, except by a reviewer, who may quote brief passages in a review. Grateful acknowledgment to Alfred Publishing and Hal Leonard Publishing for use of the lyrics to “Hell Hole” by Spinal Tap on pages 155–56. Text design and typography by Tona Pearce Myers Library of Congress Cataloging-in-Publication Data Warner, Brad. Sit down and shut up : punk rock commentaries on Buddha, god, truth, sex, death, and Dogen’s Treasury of the right dharma eye / Brad Warner. p. cm. ISBN 978-1-57731-559-9 (pbk. : alk. paper) 1. Meditation—Zen Buddhism. 2. Dogen, 1200–1253. I. Title. BQ9288.W377 2007 294.3'85—dc22 2007002802 First printing, May 2007 ISBN-10: 1-57731-559-6 ISBN-13: 978-1-57731-559-9 Printed in Canada on acid-free, recycled paper New World Library is a proud member of the Green Press Initiative. 10 9 8 7 6 5 4 3 2 1 Dedicated to my mother, Sandra Sue Warner Contents 1. Why Dogen Matters 2. “Genjo Koan” 3. Proper Posture Required 4. -

The Grizzly, November 15, 1994
Ursinus College Digital Commons @ Ursinus College Ursinus College Grizzly Newspaper Newspapers 11-15-1994 The Grizzly, November 15, 1994 Marc Ellman Ursinus College Mark Leiser Ursinus College Hope Rinehimer Ursinus College Jayson Blocksidge Ursinus College Tarik Qasim Ursinus College See next page for additional authors Follow this and additional works at: https://digitalcommons.ursinus.edu/grizzlynews Part of the Cultural History Commons, Higher Education Commons, Liberal Studies Commons, Social History Commons, and the United States History Commons Click here to let us know how access to this document benefits ou.y Recommended Citation Ellman, Marc; Leiser, Mark; Rinehimer, Hope; Blocksidge, Jayson; Qasim, Tarik; Caiazzo, Phil; Callahan, Erin; Davenport, Amy K.; Darby, Alicia; Richter, Richard P.; Landau, Maxine; Schofer, Joel; D'orsaneo, Nicole; Weingroff, Charlie; and Gaft, David, "The Grizzly, November 15, 1994" (1994). Ursinus College Grizzly Newspaper. 347. https://digitalcommons.ursinus.edu/grizzlynews/347 This Book is brought to you for free and open access by the Newspapers at Digital Commons @ Ursinus College. It has been accepted for inclusion in Ursinus College Grizzly Newspaper by an authorized administrator of Digital Commons @ Ursinus College. For more information, please contact [email protected]. Authors Marc Ellman, Mark Leiser, Hope Rinehimer, Jayson Blocksidge, Tarik Qasim, Phil Caiazzo, Erin Callahan, Amy K. Davenport, Alicia Darby, Richard P. Richter, Maxine Landau, Joel Schofer, Nicole D'orsaneo, Charlie Weingroff, and David Gaft This book is available at Digital Commons @ Ursinus College: https://digitalcommons.ursinus.edu/grizzlynews/347 Medicine -- The only profession that labors to destroy the reason for its own existence. Th~ Grizzly -James Bryce Volume xvn Number IX U rsinus College November 15, 1994 Judiciary Board Hearing Founders' Day Closes 125th Ends with Guilty Verdict Anniversary Celebration BY HOPE RINEHIMER AND Kalbacher, Fred Woll, John BY MARK LEISER tribute to Richard P. -

2009-10 Profile
Abbreviation Guide School Corporation About IHSAA Membership 2009-10 Profi le As stated in Article III of the IHSAA By-Laws & Articles of Incorporation Full Member Schools: 411 Boys Girls School Athletic Directors Junior Member Schools: 0 Section 1. Total Member Schools: 411 .......................... AD ........... Athletic Director EVANSVILLE All Memberships Are Voluntary. Any secondary school in the state may Paul Neidig become a member of this Corporation by meeting the requirements for .........................AAD .......... Asst. Athletic Director membership, by subscribing to all of these rules and regulations of the Cor- Full Members Gained: 3 [email protected] 21st Century Charter School - Gary ......................Ath Sec........ Athletic Secretary 5400 First Avenue poration, and by completing and submitting a membership application form Indiana Math & Science Academy ........................Ath Tr......... Athletic Trainer Evansville, IN 47710 to the Commissioner on or before September 1 of each year. Applications Indianapolis Shortridge (approved BA ...................................... Baseball Coach Phone: 812-435-8501 for membership by non-member schools must be accompanied with a one FAX: 812-435-8564 thousand dollar initiation fee and must be received by the Commissioner no in 2008-09) BB .......BB.......................... Basketball Coach later than August 1. ....................... Co-AD ........ Co-Athletic Director GARY Section 2. Full Members Lost: 2 CC ......CC ......................... Cross Country Coach Earl Smith Full membership in this Corporation shall be open to all public, private, Gary Wirt 1800 E. 35th Ave. parochial, boarding, and institutional high schools of the state offering and Morton Memorial FB ...................................... Football Coach Gary, IN 46409 maintaining two or more years of high school work, provided they meet the GO ....