Taking a Bite out of Bruxism by Jordan Moshkovich
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ECORFAN Journal-Spain Bruxism, Stress and Anxiety in Young People
16 Article ECORFAN Journal-Spain December, 2019 Vol.6 No.11 16-19 Bruxism, stress and anxiety in young people Bruxismo, estrés y ansiedad en jóvenes CAPETILLO-HERNÁNDEZ, Guadalupe Rosalía†*, TORRES-CAPETILLO, Evelyn Guadalupe, OCHOA-MARTINEZ, Rosa Elena and FLORES-AGUILAR, Silvia Georgina Universidad Veracruzana, Facultad de Odontología, Región Veracruz ID 1st Author: Guadalupe Rosalía, Capetillo-Hernandez / ORC ID: 0000-0002-2033-4660, Researcher ID Thomson: S- 7875-2018, CVU CONACYT ID: 386320 ID 1st Coauthor: Evelyn Guadalupe, Torres-Capetillo / ORC ID: 0000-0003-0576-0327, Researcher ID Thomson: T-1680- 2018, CVU CONACYT ID: 308188 ID 2nd Coauthor: Rosa Elena, Ochoa-Martínez / ORC ID: 0000-0002-0676-6387 ID 3rd Coauthor: Silvia Georgina, Flores-Aguilar / ORC ID: 0000-0002-5857-4969 DOI: 10.35429/EJS.2019.11.6.16.19 Received September 10, 2019; Accepted December 15, 2019 Abstract Resumen Introduction. The bruxism is the act of clenching and/or Introducción. El bruxismo que es el acto de apretar y/o grinding the teeth, a habit that compromises the orofacial rechinar los dientes, un hábito que compromete la región region. It is often associated with emotional aspects, such orofacial. A menudo se asocia con aspectos emocionales, as anxiety and stress, and can lead to alterations in como la ansiedad y el estrés , y puede dar lugar a orofacial structures, functional modifications and social alteraciones en las estructuras orofaciales, modificaciones repercussions. (1). The etiology of bruxism is unclear, but funcionales y repercusión social. (1) La etiología del the condition has been associated with stress, occlusal bruxismo no está claro, pero la condición se ha asociado disorders, allergies and sleep positioning. -

Bruxism, Related Factors and Oral Health-Related Quality of Life Among Vietnamese Medical Students
International Journal of Environmental Research and Public Health Article Bruxism, Related Factors and Oral Health-Related Quality of Life Among Vietnamese Medical Students Nguyen Thi Thu Phuong 1, Vo Truong Nhu Ngoc 1, Le My Linh 1, Nguyen Minh Duc 1,2,* , Nguyen Thu Tra 1,* and Le Quynh Anh 1,3 1 School of Odonto Stomatology, Hanoi Medical University, Hanoi 100000, Vietnam; [email protected] (N.T.T.P.); [email protected] (V.T.N.N.); [email protected] (L.M.L.); [email protected] (L.Q.A.) 2 Division of Research and Treatment for Oral Maxillofacial Congenital Anomalies, Aichi Gakuin University, 2-11 Suemori-dori, Chikusa, Nagoya, Aichi 464-8651, Japan 3 School of Dentistry, Faculty of Medicine and Health, The University of Sydney, Sydney, NSW 2000, Australia * Correspondence: [email protected] (N.M.D.); [email protected] (N.T.T.); Tel.: +81-807-893-2739 (N.M.D.); +84-963-036-443 (N.T.T.) Received: 24 August 2020; Accepted: 11 October 2020; Published: 12 October 2020 Abstract: Although bruxism is a common issue with a high prevalence, there has been a lack of epidemiological data about bruxism in Vietnam. This cross-sectional study aimed to determine the prevalence and associated factors of bruxism and its impact on oral health-related quality of life among Vietnamese medical students. Bruxism was assessed by the Bruxism Assessment Questionnaire. Temporomandibular disorders were clinically examined followed by the Diagnostic Criteria for Temporomandibular Disorders Axis I. Perceived stress, educational stress, and oral health-related quality of life were assessed using the Vietnamese version of Perceived Stress Scale 10, the Vietnamese version of the Educational Stress Scale for Adolescents, and the Vietnamese version of the 14-item Oral Health Impact Profile, respectively. -

A Philosophy of the Dreaming Mind
Dream Pluralism: A Philosophy of the Dreaming Mind By Melanie Rosen A THESIS SUBMITTED TO MACQUARIE UNIVERSITY FOR THE DEGREE OF DOCTOR OF PHILOSOPHY DEPARTMENT OF COGNITIVE SCIENCE, FACULTY OF HUMAN SCIENCE MACQUARIE UNIVERSITY, NSW 2109, AUSTRALIA JULY 2012 Table of Contents Abstract 9 Declaration 11 Acknowledgements 13 Introduction 15 Part 1: Dream Pluralism 25 Chapter 1: The Empirical Study of Dreams: Discoveries and Disputes 27 1.1 Stages of sleep 29 1.1.1 NREM Sleep 30 1.1.2 REM Sleep 32 1.1.3 The Scanning Hypothesis: an attempt to correlate eye movements with dream reports 33 1.2 Dream reports 35 1.2.1 The benefits of lab-based research 36 1.2.2 The benefits of home-based research 38 1.3 Measuring the physiology of the sleeping brain and body 41 1.3.1 Physiological measures: pros and cons 42 1.4 Cognitive and neural features of sleep 48 1.5 Lucid dreamers in the dream lab 55 Conclusion 59 1 Chapter 2: Bizarreness and Metacognition in Dreams: the Pluralist View of Content and Cognition 61 2.1 A pluralistic account of dream content 62 2.1.1 Bizarre and incoherent dreams 63 2.1.2 Dreams are not particularly bizarre 66 2.1.3 Explanations of the conflicting results 69 2.1.4 Dreams vs. fantasy reports 72 2.2 Cognition in dreams: deficient or equivalent? 80 2.2.1 What is metacognition? 80 2.2.2 Metacognition in dreams 83 Conclusion 97 Chapter 3: Rethinking the Received View: Anti-Experience and Narrative Fabrication 99 3.1 Malcolm on dreaming 101 3.1.1 Dreams and verification 102 3.1.2 Evidence against Malcolm 109 3.2 Metaphysical anti-experience theses 115 3.2.1 The cassette view 115 3.2.2 Arguments against the cassette view 118 3.2.3 Consciousness requires recognition or clout 120 3.3 Narrative fabrication in dream reports 122 3.3.1 Rationalisation of strange content 123 3.3.2 Confabulation and memory loss 127 3.3.3 Altered states of consciousness and what it’s like to be a bat. -
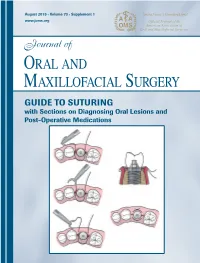
GUIDE to SUTURING with Sections on Diagnosing Oral Lesions and Post-Operative Medications
Journal of Oral and Maxillofacial Surgery Journal of Oral and Maxillofacial August 2015 • Volume 73 • Supplement 1 www.joms.org August 2015 • Volume 73 • Supplement 1 • pp 1-62 73 • Supplement 1 Volume August 2015 • GUIDE TO SUTURING with Sections on Diagnosing Oral Lesions and Post-Operative Medications INSERT ADVERT Elsevier YJOMS_v73_i8_sS_COVER.indd 1 23-07-2015 04:49:39 Journal of Oral and Maxillofacial Surgery Subscriptions: Yearly subscription rates: United States and possessions: individual, $330.00 student and resident, $221.00; single issue, $56.00. Outside USA: individual, $518.00; student and resident, $301.00; single issue, $56.00. To receive student/resident rate, orders must be accompanied by name of affiliated institution, date of term, and the signature of program/residency coordinator on institution letter- head. Orders will be billed at individual rate until proof of status is received. Prices are subject to change without notice. Current prices are in effect for back volumes and back issues. Single issues, both current and back, exist in limited quantities and are offered for sale subject to availability. Back issues sold in conjunction with a subscription are on a prorated basis. Correspondence regarding subscriptions or changes of address should be directed to JOURNAL OF ORAL AND MAXILLOFACIAL SURGERY, Elsevier Health Sciences Division, Subscription Customer Service, 3251 Riverport Lane, Maryland Heights, MO 63043. Telephone: 1-800-654-2452 (US and Canada); 314-447-8871 (outside US and Canada). Fax: 314-447-8029. E-mail: journalscustomerservice-usa@ elsevier.com (for print support); [email protected] (for online support). Changes of address should be sent preferably 60 days before the new address will become effective. -

Mouthguard Use Effect on the Biomechanical Response Of
life Article Mouthguard Use Effect on the Biomechanical Response of an Ankylosed Maxillary Central Incisor during a Traumatic Impact: A 3-Dimensional Finite Element Analysis Alexandre Luiz Souto Borges 1, Amanda Maria de Oliveira Dal Piva 1, Laís Regiane da Silva Concílio 2, Tarcisio José de Arruda Paes-Junior 1 and João Paulo Mendes Tribst 1,* 1 Institute of Science and Technology, São Paulo State University (Unesp), São José dos Campos, São Paulo 12220690, Brazil; [email protected] (A.L.S.B.); [email protected] (A.M.d.O.D.P.); [email protected] (T.J.d.A.P.-J.) 2 Department of Prosthodontics, School of Dentistry, University of Taubaté, Taubaté,São Paulo 12020-340, Brazil; [email protected] * Correspondence: [email protected]; Tel.: +55-3947-9000 Received: 15 September 2020; Accepted: 28 September 2020; Published: 20 November 2020 Abstract: (1) Background: Trauma is a very common experience in contact sports; however, there is an absence of data regarding the effect of athletes wearing mouthguards (MG) associated with ankylosed maxillary central incisor during a traumatic impact. (2) Methods: To evaluate the stress distribution in the bone and teeth in this situation, models of maxillary central incisor were created containing cortical bone, trabecular bone, soft tissue, root dentin, enamel, periodontal ligament, and antagonist teeth were modeled. One model received a MG with 4-mm thickness. Both models were subdivided into finite elements. The frictionless contacts were used and a nonlinear dynamic impact analysis was performed in which a rigid object hit the model at 1 m s 1. -

Lucid Dreaming and the Feeling of Being Refreshed in the Morning: a Diary Study
Article Lucid Dreaming and the Feeling of Being Refreshed in the Morning: A Diary Study Michael Schredl 1,* , Sophie Dyck 2 and Anja Kühnel 2 1 Central Institute of Mental Health, Medical Faculty Mannheim/Heidelberg University, Zentralinstitut für Seelische Gesundheit, J5, 68159 Mannheim, Germany 2 Department of Psychology, Medical School Berlin, Calandrellistraße 1-9, 12247 Berlin, Germany * Correspondence: [email protected]; Tel.: +49-621-1703-1782 Received: 15 December 2019; Accepted: 10 February 2020; Published: 12 February 2020 Abstract: REM periods with lucid dreaming show increased brain activation, especially in the prefrontal cortex, compared to REM periods without lucid dreaming and, thus, the question of whether lucid dreaming interferes with the recovery function of sleep arises. Cross-sectional studies found a negative relationship between sleep quality and lucid dreaming frequency, but this relationship was explained by nightmare frequency. The present study included 149 participants keeping a dream diary for five weeks though the course of a lucid dream induction study. The results clearly indicate that there is no negative effect of having a lucid dream on the feeling of being refreshed in the morning compared to nights with the recall of a non-lucid dream; on the contrary, the feeling of being refreshed was higher after a night with a lucid dream. Future studies should be carried out to elicit tiredness and sleepiness during the day using objective and subjective measurement methods. Keywords: lucid dreaming; sleep quality; nightmares 1. Introduction Lucid dreams are defined as dreams in which the dreamer is aware that he or she is dreaming [1]. -

End of an Animal
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Professional Papers Graduate School 2021 End of an Animal Alyx Brittany Chandler University of Montana, Missoula Follow this and additional works at: https://scholarworks.umt.edu/etd Let us know how access to this document benefits ou.y Recommended Citation Chandler, Alyx Brittany, "End of an Animal" (2021). Graduate Student Theses, Dissertations, & Professional Papers. 11726. https://scholarworks.umt.edu/etd/11726 This Thesis is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. END OF AN ANIMAL By ALYX BRITTANY CHANDLER Bachelor of Arts in Communication & Information Sciences, The University of Alabama, Tuscaloosa, AL, 2016 Bachelor of Science in Commerce & Business Administration, The University of Alabama, Tuscaloosa, AL, 2016 Thesis presented in partial fulfillment of the requirements for the degree of Master of Fine Arts in Creative Writing, Poetry The University of Montana Missoula, MT May 2021 Approved by: Scott Whittenburg, Dean of The Graduate School Graduate School Keetje Kuipers, Chair Department of Creative Writing Sean Hill Department of Creative Writing Dr. Sara Hayden Department of Communication Studies Chandler, Alyx, M.F.A., Spring 2021 Creative Writing End of an Animal Chairperson: Keetje Kuipers Co-Chairpeople: Sean Hill, Sara Hayden End of an Animal explores the imagined and the contradictory realities of growing up in the South near the Gulf through lyrical poetics and uncompromising language. -

Articles State Farm “With Teeth”: Heightened Judicial Review in the Absence of Executive Oversight
\\jciprod01\productn\N\NYU\89-5\NYU502.txt unknown Seq: 1 19-NOV-14 15:43 ARTICLES STATE FARM “WITH TEETH”: HEIGHTENED JUDICIAL REVIEW IN THE ABSENCE OF EXECUTIVE OVERSIGHT CATHERINE M. SHARKEY* While courts and commentators have considered the information-forcing role of executive oversight and judicial review of agency action, the dynamic relationship between the two has yet to be considered. This Article presents a novel justification for heightened judicial scrutiny in the absence of meaningful executive oversight, premised on a reasoned decision-making basis. Judicial review of certain types of agency determinations should be more stringent because those determinations have not been vetted by executive oversight and are thus less likely to be premised on reasons backed by empirical support. Agency cost-benefit analyses and agency con- flict preemption determinations—two realms rarely if ever considered together— are compared in terms of their reliance on underlying factual predicates and con- trasted in terms of the existing framework for executive oversight and judicial review of agency determinations. A heightened judicial review standard—what I term “State Farm with teeth”— should guide courts’ evaluations of the cost-benefit analyses performed by indepen- dent agencies not subject to executive oversight. This Article is the first to draw the distinction between independent and executive agencies in the State Farm hard- look context. It is also the first to explore the recent Business Roundtable decision by the D.C. Circuit through this analytical lens. The stringent “State Farm with teeth” standard should likewise be applied to judi- cial review of agency determinations of conflict preemption made in the absence of executive oversight. -

Sleep Problems
Sleep Problems About 70 million Americans have some kind of sleep problem, and for many it’s a long-term problem. Even though sleep problems are very common, they are very often undiagnosed and untreated. Here are descriptions of some of the most common sleep problems. Bruxism Bruxism is grinding, gnashing, or clenching your teeth during sleep or in situations that make you feel anxious or tense. It can be mild and happen only once in a while, or it may be violent and happen often. Bruxism most often happens in the early part of the night. You may not be aware that you have bruxism until your teeth or jaws are damaged. People who have bruxism are also more likely to snore and develop sleep apnea. Hypersomnia Hypersomnia is excessive daytime sleepiness or prolonged nighttime sleep. If you have hypersomnia, you feel very drowsy during the day and have an overwhelming urge to fall asleep, even after getting enough sleep at night. You often doze, nap, or fall asleep in situations where you need or want to be awake and alert. Other symptoms may include irritability, mild depression, trouble concentrating, and memory loss. Kleine-Levin Syndrome Kleine-Levin syndrome is a rare disorder that causes you to be extremely drowsy off and on. You may sleep up to 20 hours a day. Other symptoms include eating too much, being irritable, feeling disoriented, lacking energy, and being very sensitive to noise. The disorder usually starts in the late teens and is more common in men than in women. Symptoms may last for days to weeks, then go away, and then come back. -

190 HOVERING in DEAD SPACE: the GHOSTLY FUTURE in Please
NOTRE DAME REVIEW HOVERING IN DEAD SPACE: THE GHOSTLY FUTURE IN PLEASE PLEASE GET OVER HERE PLEASE AND THE TERRAFORMERS Jamison Crabtree. please please get over here please. Cartridge Lit, 2017. Dan Hoy. The Terraformers. Third Man Books, 2017. Jayme Russell Lately, I’ve been fixated on ghosts and the future and how those two concepts intersect. At first they seem to be diametrically opposed to one an- other, but they are also permanently interconnected. The two fade into each other; they eerily float together in Venn diagram form. The following chap- books overlap in the same way. The form and content indicate ghostliness and futurity. Although the means of publication, one a physical hand sewn book and the other a digital text on a screen, are extremely different, these two chapbooks have a similar otherworldly atmosphere and tone. When we flip the pages or scroll down, we are caught in the middle of the diagram. I. We arrive at ghosts: A haunt is another word for a face; scary to see so many floating through the world. The ghost lives in digital space in Jamison Crabtree’s please please get over here please. This online chapbook at Cartridge Lit is airy in a world without air. The white background and colorless font creates an empty space and a slow scroll/scrawl of text, at once enticingly ethereal and cautionary. Alive & dead & asleep, bodies ache to press against something new. II. The words float on until abruptly interrupted by the strangeness of videogame language. Like Carol Anne as she channels ghosts, we hear and see sound and picture with sudden clarity amid the onscreen static. -
Dreams and Nightmares with a Person’S Waking Life
When nightmares do not disappear spontaneously, psychotherapy may help. Research has demonstrated that simple techniques of dream narration and transformation of the storyline are very useful in eliminating nightmares. Children may be encouraged to share their nightmare experiences with parents and professionals; very young children can benefit from drawing them. It is well documented that traumatic experiences can trigger intensive recurrent nightmares. These NIGHTMARES AND SLEEP nightmares can be associated with post-traumatic TERRORS stress disorder (PTSD), which is often experienced as Dreams and Some dream experiences are particularly distressing a result of war, assault, accidents, and other trauma. and have a negative impact on waking life. Professional help is recommended to alleviate Nightmares are well-elaborated dreams that have recurring nightmares following trauma. Nightmares a frightful, anxious or other dysphoric content that usually wakes up the dreamer. Nightmares tend to WHAT IS DREAMING? occur late in the night and normally during episodes of REM sleep. Sleep terrors, in contrast, are characterized by sudden awakenings from deep (non-REM) sleep near the beginning of the night. Although they too are WHAT ARE THE SOURCES associated with intense and negative mental OF DREAMS? experiences, they are typically very short and not remembered the next morning. The person wakes up from a sleep terror very suddenly with a dramatically increased respiration and heart rate and outward ARE DREAMS USEFUL? expressions of fear or panic. Sleep terrors can cause serious injuries at night and substantial daytime distress. Nightmares increase in prevalence through childhood into adolescence. From 1% to 4% of NIGHTMARES AND parents report their preschoolers have nightmares SLEEP TERRORS “often” or “always”. -
The Tooth Gets Short Shrift in Anatomy Class: We Spend All of Five Minutes on It
CHAPTER FOUR TEETH EVERYWHERE The tooth gets short shrift in anatomy class: we spend all of five minutes on it. In the pantheon of favorite organs—I’ll leave it to each of you to make your list—teeth rarely reach the top five. Yet the little tooth contains so much of our connection to the rest of life that it is virtually impossible to understand our bodies without knowing teeth. Teeth also have special significance for me, because it was in searching for them that I first learned how to find fossils and how to run a fossil expedition. The job of teeth is to make bigger creatures into smaller pieces. When attached to a moving jaw, teeth slice, dice, and macerate. Mouths are only so big, and teeth enable creatures to eat things that are bigger than their mouths. This is particularly true of creatures that do not have hands or claws that can shred or cut things before they get to the mouth. True, big fish tend to eat littler fish. But teeth can be the great equalizer: smaller fish can munch on bigger fish if they have good teeth. Smaller fish can use their teeth to scrape scales, feed on particles, or take out whole chunks of 81 flesh from bigger fish. We can learn a lot about an animal by looking at its teeth. The bumps, pits, and ridges on teeth often reflect the diet. Carnivores, such as cats, have blade-like molars to cut meat, while plant eaters have a mouth full of flatter teeth that can macerate leaves and nuts.