Conductive Hearing Loss
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CASE REPORT Resolution of Delayed Sudden Sensorineural Hearing Loss After Stapedectomy
The Mediterranean Journal of Otology CASE REPORT Resolution of Delayed Sudden Sensorineural Hearing Loss After Stapedectomy: A Case Report and Review of the Literature Noam Yehudai, MD, Michal Luntz, MD From the Department of Significant sensorineural hearing loss may develop immediately after suc- Otolaryngology, Head and Neck cessful stapedectomy but sometimes occurs months or even years later. Surgery, Bnai-Zion Medical The rate of recovery from that disorder has not been determined. Several Center, Technion-Israel School of Technology, Haifa, Israel reports in the 1960s described patients with delayed sensorineural hear- ing loss, but that entity has not been mentioned in the English-language Correspondence literature for the last 30 years. We present a review of the literature on this Michal Luntz, MD postsurgical auditory complication and describe a patient with delayed Department of Otolaryngology, Head and Neck Surgery poststapedectomy sensorineural hearing loss that developed 15 months Bnai-Zion Medical Center, after surgery and resolved completely after treatment with an oral steroid. Technion-Israel School of Technology 47 Golomb St, PO Box 4940, Haifa 31048, Israel Phone: 972-4-8359544 Fax: 972-4-8361069 E-mail: [email protected] Submitted: 05 February, 2006 Revised: 07 May, 2006 Accepted: 09 May, 2006 Mediterr J Otol 2006; 3: 156-160 Copyright 2005 © The Mediterranean Society of Otology and Audiology 156 Resolution of Delayed Sudden Sensorineural Hearing Loss After Stapedectomy: A Case Report and Review of the Literature -
A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: a Clinical Study
Int Adv Otol 2014; 10(2): 102-6 • DOI: 10.5152/iao.2014.40 Original Article A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: A Clinical Study Can Özbay, Rıza Dündar, Erkan Kulduk, Kemal Fatih Soy, Mehmet Aslan, Hüseyin Katılmış Department of Otorhinolaryngology, Şifa University Faculty of Medicine, İzmir, Turkey (CÖ) Department of Otorhinolaryngology, Mardin State Hospital, Mardin, Turkey (RD, EK, KFS, MA) Department of Otorhinolaryngology, Katip Çelebi University Atatürk Training and Research Hospital, İzmir, Turkey (HK) OBJECTIVE: Myringosclerosis (MS) is a pathological condition characterized by hyaline degeneration and calcification of the collagenous structure of the fibrotic layer of the tympanic membrane, which may develop after trauma, infection, or inflammation as myringotomy, insertion of a ventila- tion tube, or myringoplasty. The aim of our study was to both reveal and evaluate the impact of the factors that might be effective on the post-tym- panoplasty development of myringosclerosis in the graft. MATERIALS and METHODS: In line with this objective, a total of 108 patients (44 males and 64 females) aged between 11 and 66 years (mean age, 29.5 years) who had undergone type 1 tympanoplasty (TP) with an intact canal wall technique and type 2 TP, followed up for an average of 38.8 months, were evaluated. In the presence of myringosclerosis, in consideration of the tympanic membrane (TM) quadrants involved, the influential factors were analyzed in our study, together with the development of myringosclerosis, including preoperative factors, such as the presence of myringosclerosis in the residual and also contralateral tympanic membrane, extent and location of the perforation, and perioperative factors, such as tympanosclerosis in the middle ear and mastoid cavity, cholesteatoma, granulation tissue, and type of the operation performed. -

Temporo-Mandibular Joint (Tmj) Dysfunction
Office: (310) 423-1220 BeverlyHillsENT.com Fax: (310) 423-1230 TEMPORO-MANDIBULAR JOINT (TMJ) DYSFUNCTION You may not have heard of it, but you use it hundreds of times every day. It is the Temporo- Mandibular Joint (TMJ), the joint where the mandible (the lower jaw) joins the temporal bone of the skull, immediately in front of the ear on each side of your head. You move the joint every time you chew or swallow. You can locate this joint by putting your finger on the triangular structure in front of your ear. Then move your finger just slightly forward and press firmly while you open your jaw all the way and shut it. The motion you feel is the TMJ. You can also feel the joint motion in your ear canal. These maneuvers can cause considerable discomfort to a patient who is having TMJ trouble, and physicians use these maneuvers with patients for diagnosis. TMJ Dysfunction can cause the following symptoms: Ear pain Sore jaw muscles Temple/cheek pain Jaw popping/clicking Locking of the jaw Difficulty in opening the mouth fully Frequent head/neck aches The pain may be sharp and searing, occurring each time you swallow, yawn, talk, or chew, or it may be dull and constant. It hurts over the joint, immediately in front of the ear, but pain can also radiate elsewhere. It often causes spasms in the adjacent muscles that are attached to the bones of the skull, face, and jaws. Then, pain can be felt at the side of the head (the temple), the cheek, the lower jaw, and the teeth. -

UPDATE VOLUME 20 • ISSUE 3 the Newsletter of the Council for Accreditation in Occupational Hearing Conservation
Fall 2008 UPDATE VOLUME 20 • ISSUE 3 The Newsletter of the Council for Accreditation in Occupational Hearing Conservation Hearing noise-induced hearing loss and further degradation of communication. If too much hearing protection is provided, Conservation the combined effects of the hearing loss and the attenuation provided by the hearing protector may result in critical sounds for the Hearing- and communication signals becoming inaudible. I’m often asked what type of hearing protector is best for Impaired Worker workers with hearing impairment. Considering that there is no ‘best’ HPD for all workers in any hearing category, it Introduction by Ted Madison should come as no surprise that no single type of device will The prevalence of hearing loss among persons enrolled meet the needs of all those with hearing loss. What seems in occupational hearing conservation programs (HCPs) is to be consistent, however, is that each case is unique, and difficult to determine. Recently, Tak and Calvert (2008) that extra time and effort is required to help these workers estimated that 11.4% of the overall US workforce reports find the right combination of protection, having hearing difficulty of varying communication and auditory awareness. degrees and that approximately ¼ of Consultation with an audiologist or other the hearing difficulty reported can hearing health care professional is also be attributed to employment. These an important step in most cases. estimates are based on analysis of data One valuable resource is the OSHA from the US National Health Interview Safety & Health Information Bulletin Survey (NHIS) that were collected (SHIB) titled “Hearing Conservation from 1997 to 2003. -
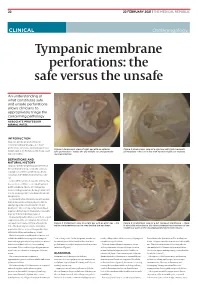
Tympanic Membrane Perforations: the Safe Versus the Unsafe
TMR_210222_22 2021-02-12T14:56:54+11:00 22 22 FEBRUARY 2021 | THE MEDICAL REPUBLIC CLINICAL Otolaryngology Tympanic membrane perforations: the safe versus the unsafe An understanding of what constitutes safe and unsafe perforations allows clinicians to appropriately triage the concerning pathology ASSOCIATE PROFESSOR NIRMAL PATEL INTRODUCTION Tympanic membrane perforations are seen frequently in general practice. Some perforations can be associated with significant Figure 1: Endoscopic view of right ear with an anterior Figure 2: Endoscopic view of a right ear with twin traumatic disease, such as cholesteatoma which may cause safe perforation – notice the dry middle ear and posterior perforations – the ear is dry with normal middle ear mucosa. major morbidity. myringosclerosis DEFINITIONS AND NATURAL HISTORY Tympanic membrane perforations are holes in the ear drum that most commonly occur as a consequence of either ear infections, chronic eustachian tube dysfunction or trauma to the ear. Acute middle ear infection (acute otitis media) is a common condition occurring at least once in 80% of children. Most acute otitis media resolves with spontaneous discharge of infected secretions through the eustachian tube into the nasopharynx. Occasionally when the infections are frequent, there is extensive scarring (tympanosclerosis and myringosclerosis) of the ear drum and middle ear . This scarring compromises blood supply to the healing ear drum and occasionally stops the hole from healing. (Figure 1) Traumatically induced holes occur from a rapid compression of the air column in the external ear canal, most commonly from a blow to the Figure 3: Endoscopic view of a right ear with an attic wax – the Figure 4: Endoscopic view of a left tympanic membrane – there white cholesteatoma can be seen behind the ear drum. -
Instruction Sheet: Otitis Externa
University of North Carolina Wilmington Abrons Student Health Center INSTRUCTION SHEET: OTITIS EXTERNA The Student Health Provider has diagnosed otitis externa, also known as external ear infection, or swimmer's ear. Otitis externa is a bacterial/fungal infection in the ear canal (the ear canal goes from the outside opening of the ear to the eardrum). Water in the ear, from swimming or bathing, makes the ear canal prone to infection. Hot and humid weather also predisposes to infection. Symptoms of otitis externa include: ear pain, fullness or itching in the ear, ear drainage, and temporary loss of hearing. These symptoms are similar to those caused by otitis media (middle ear infection). To differentiate between external ear infection and middle ear infection, the provider looks in the ear with an instrument called an otoscope. It is important to distinguish between the two infections, as they are treated differently: External otitis is treated with drops in the ear canal, while middle ear infection is sometimes treated with an antibiotic by mouth. MEASURES YOU SHOULD TAKE TO HELP TREAT EXTERNAL EAR INFECTION: 1. Use the ear drops regularly, as directed on the prescription. 2. The key to treatment is getting the drops down into the canal and keeping the medicine there. To accomplish this: Lie on your side, with the unaffected ear down. Put three to four drops in the infected ear canal, then gently pull the outer ear back and forth several times, working the medicine deeper into the ear canal. Remain still, good-ear-side-down for about 15 minutes. -

The Ear, Nose, and Throat Exam Jeffrey Texiera, MD and Joshua Jabaut, MD CPT, MC, USA LT, MC, USN
The Ear, Nose, and Throat Exam Jeffrey Texiera, MD and Joshua Jabaut, MD CPT, MC, USA LT, MC, USN Midatlantic Regional Occupational and Environmental Medicine Conference Sept. 23, 2017 Disclosures ●We have no funding or financial interest in any product featured in this presentation. The items included are for demonstration purposes only. ●We have no conflicts of interest to disclose. Overview ● Overview of clinically oriented anatomy - presented in the format of the exam ● The approach ● The examination ● Variants of normal anatomy ● ENT emergencies ● Summary/highlights ● Questions Anatomy ● The head and neck exam consists of some of the most comprehensive and complicated anatomy in the human body. ● The ear, nose, and throat comprise a portion of that exam and a focused clinical encounter for an acute ENT complaint may require only this portion of the exam. Ears www.Medscape.com www.taqplayer.info Ear – Vestibular organ www.humanantomylibrary.com Nose/Sinus Anatomy Inferior Middle Turbinate Turbinate Septum Dorsum Sidewalls Ala Floor Tip www.ENT4Students.blogspot.com Columella Vestibule www.beautyepic.com Oral cavity and oropharynx (throat) www.apsubiology.org Neck www.rdhmag.com The Ear, Nose, and Throat exam Perform in a standardized systematic way that works for you Do it the same way every time, this mitigates risk of missing a portion of the exam Practice the exam to increase comfort with performance and familiarize self with variants of normal Describe what you are doing to the patient, describe what you see in your documentation Use your PPE as appropriate A question to keep in mind… ●T/F: The otoscope is the optimal tool for examining the tympanic membrane. -

Consultation Diagnoses and Procedures Billed Among Recent Graduates Practicing General Otolaryngology – Head & Neck Surger
Eskander et al. Journal of Otolaryngology - Head and Neck Surgery (2018) 47:47 https://doi.org/10.1186/s40463-018-0293-8 ORIGINALRESEARCHARTICLE Open Access Consultation diagnoses and procedures billed among recent graduates practicing general otolaryngology – head & neck surgery in Ontario, Canada Antoine Eskander1,2,3* , Paolo Campisi4, Ian J. Witterick5 and David D. Pothier6 Abstract Background: An analysis of the scope of practice of recent Otolaryngology – Head and Neck Surgery (OHNS) graduates working as general otolaryngologists has not been previously performed. As Canadian OHNS residency programs implement competency-based training strategies, this data may be used to align residency curricula with the clinical and surgical practice of recent graduates. Methods: Ontario billing data were used to identify the most common diagnostic and procedure codes used by general otolaryngologists issued a billing number between 2006 and 2012. The codes were categorized by OHNS subspecialty. Practitioners with a narrow range of procedure codes or a high rate of complex procedure codes, were deemed subspecialists and therefore excluded. Results: There were 108 recent graduates in a general practice identified. The most common diagnostic codes assigned to consultation billings were categorized as ‘otology’ (42%), ‘general otolaryngology’ (35%), ‘rhinology’ (17%) and ‘head and neck’ (4%). The most common procedure codes were categorized as ‘general otolaryngology’ (45%), ‘otology’ (23%), ‘head and neck’ (13%) and ‘rhinology’ (9%). The top 5 procedures were nasolaryngoscopy, ear microdebridement, myringotomy with insertion of ventilation tube, tonsillectomy, and turbinate reduction. Although otology encompassed a large proportion of procedures billed, tympanoplasty and mastoidectomy were surprisingly uncommon. Conclusion: This is the first study to analyze the nature of the clinical and surgical cases managed by recent OHNS graduates. -

BMC Ear, Nose and Throat Disorders Biomed Central
BMC Ear, Nose and Throat Disorders BioMed Central Case report Open Access Acute unilateral hearing loss as an unusual presentation of cholesteatoma Daniel Thio*1, Shahzada K Ahmed2 and Richard C Bickerton3 Address: 1Department of Otorhinolaryngology, South Warwickshire General Hospitals NHS Trust Warwick CV34 5BW UK, 2Department of Otorhinolaryngology, South Warwickshire General Hospitals NHS Trust Warwick CV34 5BW UK and 3Department of Otorhinolaryngology, South Warwickshire General Hospitals NHS Trust Warwick CV34 5BW UK Email: Daniel Thio* - [email protected]; Shahzada K Ahmed - [email protected]; Richard C Bickerton - [email protected] * Corresponding author Published: 18 September 2005 Received: 10 July 2005 Accepted: 18 September 2005 BMC Ear, Nose and Throat Disorders 2005, 5:9 doi:10.1186/1472-6815-5-9 This article is available from: http://www.biomedcentral.com/1472-6815/5/9 © 2005 Thio et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: Cholesteatomas are epithelial cysts that contain desquamated keratin. Patients commonly present with progressive hearing loss and a chronically discharging ear. We report an unusual presentation of the disease with an acute hearing loss suffered immediately after prolonged use of a pneumatic drill. Case presentation: A 41 year old man with no previous history of ear problems presented with a sudden loss of hearing in his right ear immediately following the prolonged use of a pneumatic drill on concrete. -

Investigation of the Incidence of Eustachian Tube Dysfunction in Patients with Sinonasal Disease*
ORIGINAL CONTRIBUTION Investigation of the incidence of Eustachian tube dysfunction in patients with sinonasal disease* 1 2 1 1 C.E. Rennie , M. Gutierrez , Y. Darby , V.J. Lund Rhinology Online, Vol 1: 85 - 89, 2018 http://doi.org/10.4193/RHINOL/18.050 1 Royal National Throat Nose and Ear Hospital, ENT, London, United Kingdom 2 University of North Carolina, Medical student, North Carolina, USA *Received for publication: August 12, 2018 Accepted: August 14, 2018 Abstract Background: Rhinosinusitis is characterised by inflammation affecting the respiratory mucosa of the nose and sinuses. Since the Eustachian tube and the middle ear cavity are also lined by the same mucosa, it is likely that the pathophysiological processes that give rise to rhinosinusitis will also affect these areas. Eustachian tube dysfunction (ETD) is a common condition, but it is often dismissed as a "minor" symptom in rhinology patients. Objective: The aim of this study was to determine the frequency of otologic symptoms in patients attending the rhinology clinic. The seven-item Eustachian Tube Dysfunction Questionnaire (ETDQ-7), a validated disease-specific instrument was used to assess symptoms with respect to ETD7. Study design: 119 patients attending the rhinology outpatient clinic completed ETDQ-7, a SNOT 22 and had their PNIF measured. Results: The results showed a significantly higher rate of ETD (p<0.01 paired t-test) in the rhinology patients (mean score 3.1, SD 1.64) as compared to a control population (mean 1.3, SD 0.3). Conclusion: Eustachian tube dysfunction is more common in rhinology patients then the general population, and within the rhinology population. -

Tympanostomy Tubes in Children Final Evidence Report: Appendices
Health Technology Assessment Tympanostomy Tubes in Children Final Evidence Report: Appendices October 16, 2015 Health Technology Assessment Program (HTA) Washington State Health Care Authority PO Box 42712 Olympia, WA 98504-2712 (360) 725-5126 www.hca.wa.gov/hta/ [email protected] Tympanostomy Tubes Provided by: Spectrum Research, Inc. Final Report APPENDICES October 16, 2015 WA – Health Technology Assessment October 16, 2015 Table of Contents Appendices Appendix A. Algorithm for Article Selection ................................................................................................. 1 Appendix B. Search Strategies ...................................................................................................................... 2 Appendix C. Excluded Articles ....................................................................................................................... 4 Appendix D. Class of Evidence, Strength of Evidence, and QHES Determination ........................................ 9 Appendix E. Study quality: CoE and QHES evaluation ................................................................................ 13 Appendix F. Study characteristics ............................................................................................................... 20 Appendix G. Results Tables for Key Question 1 (Efficacy and Effectiveness) ............................................. 39 Appendix H. Results Tables for Key Question 2 (Safety) ............................................................................ -

Acoustic Trauma and Hyperbaric Oxygen Treatment
Acoustic Trauma and Hyperbaric Oxygen Treatment Mesut MUTLUOGLU Department of Underwater and Hyperbaric Medicine Gulhane Military Medical Academy Haydarpasa Teaching Hospital 34668, Uskudar, Istanbul TURKEY [email protected] ABSTRACT As stated in the conclusions of the HFM-192 report on hyperbaric oxygen therapy (HBOT) in military medical setting, acoustic trauma is a frequent consequence of military activity in operation. Acoustic trauma refers to an acute hearing loss following a single sudden and very intense noise exposure. It differs from chronic noise induced hearing (NIHL) loss in that it is usually unilateral and causes sudden profound hearing loss. Acoustic trauma is a type of sensorineural hearing loss affecting inner ear structures; particularly the inner and outer hair cells of the organ of Corti within the cochlea. Exposure to noise levels above 85 decibel (dB) may cause hearing loss. While long-term exposure to repetitive or continuous noise above 85 dB may cause chronic NIHL, a single exposure above 130-140 dB, as observed in acoustic trauma, may cause acute NIHL. The loudest sound a human ear may tolerate without pain varies individually, but is usually around 120dB. Military personnel are especially at increased risk for acoustic trauma due to fire arm use in the battle zone. While a machine gun generates around 145dB sound, a rifle generates 157- 163dB, a 105 mm towed howitzer 183dB and an improvised explosive device around 180dB sound. Acoustic trauma displays a gradually down-slopping pattern in the audiogram, particularly after 3000Hz and is therefore described as high-frequency hearing loss. Tinnitus is almost always associated with acoustic trauma.