Novel and Recurrent Non-Truncating Mutations of the MITF Basic Domain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Melanocytes and Their Diseases
Downloaded from http://perspectivesinmedicine.cshlp.org/ on October 2, 2021 - Published by Cold Spring Harbor Laboratory Press Melanocytes and Their Diseases Yuji Yamaguchi1 and Vincent J. Hearing2 1Medical, AbbVie GK, Mita, Tokyo 108-6302, Japan 2Laboratory of Cell Biology, National Cancer Institute, National Institutes of Health, Bethesda, Maryland 20892 Correspondence: [email protected] Human melanocytes are distributed not only in the epidermis and in hair follicles but also in mucosa, cochlea (ear), iris (eye), and mesencephalon (brain) among other tissues. Melano- cytes, which are derived from the neural crest, are unique in that they produce eu-/pheo- melanin pigments in unique membrane-bound organelles termed melanosomes, which can be divided into four stages depending on their degree of maturation. Pigmentation production is determined by three distinct elements: enzymes involved in melanin synthesis, proteins required for melanosome structure, and proteins required for their trafficking and distribution. Many genes are involved in regulating pigmentation at various levels, and mutations in many of them cause pigmentary disorders, which can be classified into three types: hyperpigmen- tation (including melasma), hypopigmentation (including oculocutaneous albinism [OCA]), and mixed hyper-/hypopigmentation (including dyschromatosis symmetrica hereditaria). We briefly review vitiligo as a representative of an acquired hypopigmentation disorder. igments that determine human skin colors somes can be divided into four stages depend- Pinclude melanin, hemoglobin (red), hemo- ing on their degree of maturation. Early mela- siderin (brown), carotene (yellow), and bilin nosomes, especially stage I melanosomes, are (yellow). Among those, melanins play key roles similar to lysosomes whereas late melanosomes in determining human skin (and hair) pigmen- contain a structured matrix and highly dense tation. -

PIGMENT CELL & MELANOMA Research
The official journal of INTERNATIONAL FEDERATION OF PIGMENT CELL SOCIETIES · SOCIETY FOR MELANOMA RESEARCH PIGMENT CELL & MELANOMA Research Hearing dysfunction in heterozygous Mitf Mi-wh/+ mice, a model for Waardenburg syndrome type 2 and Tietz syndrome Christina Ni, Deming Zhang, Lisa A. Beyer, Karin E. Halsey, Hideto Fukui, Yehoash Raphael, David F. Dolan and Thomas J. Hornyak DOI: 10.1111/pcmr.12030 Volume 26, Issue 1, Pages 78-87 If you wish to order reprints of this article, please see the guidelines here Supporting Information for this article is freely available here EMAIL ALERTS Receive free email alerts and stay up-to-date on what is published in Pigment Cell & Melanoma Research – click here Submit your next paper to PCMR online at http://mc.manuscriptcentral.com/pcmr Subscribe to PCMR and stay up-to-date with the only journal committed to publishing basic research in melanoma and pigment cell biology As a member of the IFPCS or the SMR you automatically get online access to PCMR. Sign up as a member today at www.ifpcs.org or at www.societymelanomaresarch.org To take out a personal subscription, please click here More information about Pigment Cell & Melanoma Research at www.pigment.org Pigment Cell Melanoma Res. 26; 78–87 ORIGINAL ARTICLE Hearing dysfunction in heterozygous Mitf Mi-wh/+ mice, a model for Waardenburg syndrome type 2 and Tietz syndrome Christina Ni1, Deming Zhang1, Lisa A. Beyer2, Karin E. Halsey2, Hideto Fukui2, Yehoash Raphael2, David F. Dolan2 and Thomas J. Hornyak1,3,4 1 Dermatology Branch, Center for Cancer -

E S P C R B U L L E T
E S P C R B U L L E T I N N° 54 April 2006 PUBLISHED BY THE EUROPEAN SOCIETY FOR PIGMENT CELL RESEARCH EDITOR: G. GHANEM (Brussels) INTERNATIONAL F. BEERMANN (Lausanne), J. BOROVANSKY (Prague), M. d’ISCHIA (Naples), JC GARCIA-BORRON (Murcia), , A. NAPOLITANO (Naples), M. PICARDO (Rome), N. SMIT (Leiden). EDITORIAL BOARD: R. MORANDINI (Brussels) Ed Ph In La stitu bor one ito 7. 3. 5. 2. 4. 8. 1. Review oftheliterature communications, ... Discussion, Letterstotheeditor,Reviews,Short CONTENTS Announcements andrelatedactivities 9. Melanomaexperime 6. ria at : t J.Bo 32 ory of Genetics, molecularand Neur Photobiology MSH, MCH,ot Melanosomes Tyrosinase, TRPs,otherenzymes l (DrA.Napolitano) Biology ofpigmentcells Chemistr Office (Dr M.Picardo) (Dr F.Beermann) (Prof JC.Garcia-Borron) - 2 - rdet, Ru 5 Onc 41 omel : .3 G. G o 2. l o 9 e Hég gy a 6 h y ofM a ani F n e n a e m d x: r-Bo Experi (Ed n (DrN.S 3 (Pro s 2 rd (ProfM.d'Ischia) - her hor ito 2 e et 1,B–10 - 5 r) me l a 41 , f J.Bo nt ni C. Meunier .3 al ntal 3. ns andot S 4 m mones u 9 rg 00 developmentalbiology , cellcult it) ery ro and pigmentarydisorders Bru , R. M ( van E-M L s sels, . O (DrR.Morandini) BULLETI R P S E her o .C a r sky i a . Belg l E : ndini g .) pi g ur , h ) ium. Uni a ( e gments n P e versi m ro @ duc u t é l t b Li i on Te . -

Hearing Loss in Waardenburg Syndrome: a Systematic Review
Clin Genet 2016: 89: 416–425 © 2015 John Wiley & Sons A/S. Printed in Singapore. All rights reserved Published by John Wiley & Sons Ltd CLINICAL GENETICS doi: 10.1111/cge.12631 Review Hearing loss in Waardenburg syndrome: a systematic review Song J., Feng Y., Acke F.R., Coucke P., Vleminckx K., Dhooge I.J. Hearing J. Songa,Y.Fenga, F.R. Ackeb, loss in Waardenburg syndrome: a systematic review. P. Couckec,K.Vleminckxc,d Clin Genet 2016: 89: 416–425. © John Wiley & Sons A/S. Published by and I.J. Dhoogeb John Wiley & Sons Ltd, 2015 aDepartment of Otolaryngology, Xiangya Waardenburg syndrome (WS) is a rare genetic disorder characterized by Hospital, Central South University, Changsha, People’s Republic of China, hearing loss (HL) and pigment disturbances of hair, skin and iris. b Classifications exist based on phenotype and genotype. The auditory Department of Otorhinolaryngology, cDepartment of Medical Genetics, Ghent phenotype is inconsistently reported among the different Waardenburg types University/Ghent University Hospital, and causal genes, urging the need for an up-to-date literature overview on Ghent, Belgium, and dDepartment for this particular topic. We performed a systematic review in search for articles Biomedical Molecular Biology, Ghent describing auditory features in WS patients along with the associated University, Ghent, Belgium genotype. Prevalences of HL were calculated and correlated with the different types and genes of WS. Seventy-three articles were included, describing 417 individual patients. HL was found in 71.0% and was Key words: genotype – hearing loss – predominantly bilateral and sensorineural. Prevalence of HL among the inner ear malformation – phenotype – different clinical types significantly differed (WS1: 52.3%, WS2: 91.6%, Waardenburg syndrome WS3: 57.1%, WS4: 83.5%). -

Hereditary Hearing Impairment with Cutaneous Abnormalities
G C A T T A C G G C A T genes Review Hereditary Hearing Impairment with Cutaneous Abnormalities Tung-Lin Lee 1 , Pei-Hsuan Lin 2,3, Pei-Lung Chen 3,4,5,6 , Jin-Bon Hong 4,7,* and Chen-Chi Wu 2,3,5,8,* 1 Department of Medical Education, National Taiwan University Hospital, Taipei City 100, Taiwan; [email protected] 2 Department of Otolaryngology, National Taiwan University Hospital, Taipei 11556, Taiwan; [email protected] 3 Graduate Institute of Clinical Medicine, National Taiwan University College of Medicine, Taipei City 100, Taiwan; [email protected] 4 Graduate Institute of Medical Genomics and Proteomics, National Taiwan University College of Medicine, Taipei City 100, Taiwan 5 Department of Medical Genetics, National Taiwan University Hospital, Taipei 10041, Taiwan 6 Department of Internal Medicine, National Taiwan University Hospital, Taipei 10041, Taiwan 7 Department of Dermatology, National Taiwan University Hospital, Taipei City 100, Taiwan 8 Department of Medical Research, National Taiwan University Biomedical Park Hospital, Hsinchu City 300, Taiwan * Correspondence: [email protected] (J.-B.H.); [email protected] (C.-C.W.) Abstract: Syndromic hereditary hearing impairment (HHI) is a clinically and etiologically diverse condition that has a profound influence on affected individuals and their families. As cutaneous findings are more apparent than hearing-related symptoms to clinicians and, more importantly, to caregivers of affected infants and young individuals, establishing a correlation map of skin manifestations and their underlying genetic causes is key to early identification and diagnosis of syndromic HHI. In this article, we performed a comprehensive PubMed database search on syndromic HHI with cutaneous abnormalities, and reviewed a total of 260 relevant publications. -

Waardenburg Syndrome Type 1 11/10/01 13:15
Waardenburg Syndrome Type 1 11/10/01 13:15 Funded by the NIH • Developed at the University of Washington, Seattle Waardenburg Syndrome Type 1 [WS1] Author: Jeff Milunsky, MD Boston University School of Medicine Posted: 30 July 2001 Summary Disease characteristics. Waardenburg syndrome type 1 (WS1) is an auditory-pigmentary disorder comprising congenital sensorineural hearing loss and pigmentary disturbances of the iris, hair, and skin, along with dystopia canthorum (lateral displacement of the inner canthi). The hearing loss in WS1 observed in ~57% of patients is congenital, typically nonprogressive, either unilateral or bilateral, and of the sensorineural type. The most common type of hearing loss in WS1 is profound bilateral loss (>100dB). The classic white forelock observed in ~45% of patients is the most common hair pigmentation anomaly seen in WS. The majority of individuals with WS1 have either a white forelock or early graying of the scalp hair before age 30 years. Patients may have complete heterochromia iridium, partial/segmental heterochromia, or hypoplastic or brilliant blue irides. Diagnosis/testing. The diagnosis is established by clinical findings in most patients. Diagnostic criteria rely upon the presence of sensorineural hearing loss, pigmentary changes, and calculation of the W index to identify dystopia canthorum. Molecular genetic testing by sequencing of the PAX3 gene (chromosomal locus 2q35) detects over 90% of disease-causing mutations. Such testing is available clinically. Molecular genetic testing can be used to confirm the diagnosis in atypical cases; however, it is primarily used for genetic counseling of at-risk family members. Genetic counseling. Waardenburg syndrome is inherited in an autosomal dominant manner. -

Comprehensive Inherited Cancer Precision Panel Overview
Comprehensive Inherited Cancer Precision Panel Overview Hereditary cancer syndromes are encountered in all medical specialties. Although they account for about 5% of all malignancies, it is of special importance to identify these patients because, unlike patients with sporadic cancers, they require special, long-term care as their predisposition can cause them to develop certain tumors at a relatively early age. These cancers can arise in the lungs, kidneys, liver, pancreas, skin, eyes, heart. Most hereditary cancers are associated with a “germline mutation” that will be present in every cell of the human body. Identification of patients at risk of inherited cancer susceptibility is dependent upon the ability to characterize genes and alterations associated with increased cancer risk as well as gathering a detailed personal and family history aiding in the identification of the mode of inheritance as well as other family members at risk of suffering from this susceptibility. Most hereditary cancer syndromes follow an autosomal dominant inheritance, and the penetrance is high. The Igenomix Comprehensive Inherited Cancer Precision Panel provides a comprehensive analysis of the most common hereditary cancer syndromes using next-generation sequencing (NGS) to fully understand the spectrum of relevant cancer predisposition genes. Indications The Igenomix Comprehensive Inherited Caner Precision Panel is indicated as a screening and diagnostic test in those cases where there are: ‐ Multiple relatives on the same side of the family with the same or related forms of cancer ‐ Cancer at an early age ‐ Early presentation of an aggressive cancer type ‐ Multiple primary cancers in an individual 1 Clinical Utility The clinical utility of this panel is: ‐ Early and accurate genetic diagnosis allowing the most appropriate clinical management of a patient with personal or family history suggestive of a hereditary cancer syndrome. -

Table I. Genodermatoses with Known Gene Defects 92 Pulkkinen
92 Pulkkinen, Ringpfeil, and Uitto JAM ACAD DERMATOL JULY 2002 Table I. Genodermatoses with known gene defects Reference Disease Mutated gene* Affected protein/function No.† Epidermal fragility disorders DEB COL7A1 Type VII collagen 6 Junctional EB LAMA3, LAMB3, ␣3, 3, and ␥2 chains of laminin 5, 6 LAMC2, COL17A1 type XVII collagen EB with pyloric atresia ITGA6, ITGB4 ␣64 Integrin 6 EB with muscular dystrophy PLEC1 Plectin 6 EB simplex KRT5, KRT14 Keratins 5 and 14 46 Ectodermal dysplasia with skin fragility PKP1 Plakophilin 1 47 Hailey-Hailey disease ATP2C1 ATP-dependent calcium transporter 13 Keratinization disorders Epidermolytic hyperkeratosis KRT1, KRT10 Keratins 1 and 10 46 Ichthyosis hystrix KRT1 Keratin 1 48 Epidermolytic PPK KRT9 Keratin 9 46 Nonepidermolytic PPK KRT1, KRT16 Keratins 1 and 16 46 Ichthyosis bullosa of Siemens KRT2e Keratin 2e 46 Pachyonychia congenita, types 1 and 2 KRT6a, KRT6b, KRT16, Keratins 6a, 6b, 16, and 17 46 KRT17 White sponge naevus KRT4, KRT13 Keratins 4 and 13 46 X-linked recessive ichthyosis STS Steroid sulfatase 49 Lamellar ichthyosis TGM1 Transglutaminase 1 50 Mutilating keratoderma with ichthyosis LOR Loricrin 10 Vohwinkel’s syndrome GJB2 Connexin 26 12 PPK with deafness GJB2 Connexin 26 12 Erythrokeratodermia variabilis GJB3, GJB4 Connexins 31 and 30.3 12 Darier disease ATP2A2 ATP-dependent calcium 14 transporter Striate PPK DSP, DSG1 Desmoplakin, desmoglein 1 51, 52 Conradi-Hu¨nermann-Happle syndrome EBP Delta 8-delta 7 sterol isomerase 53 (emopamil binding protein) Mal de Meleda ARS SLURP-1 -

Progress in Molecular Genetics of Heritable Skin Diseases: the Paradigms of Epidermolysis Bullosa and Pseudoxanthoma Elasticum
Progress in Molecular Genetics of Heritable Skin Diseases: The Paradigms of Epidermolysis Bullosa and Pseudoxanthoma Elasticum Jouni Uitto, Leena Pulkkinen, and Franziska Ringpfeil Departments of Dermatology and Cutaneous Biology, and Biochemistry and Molecular Pharmacology, Je¡erson Medical College, and Je¡erson Institute of Molecular Medicine,Thomas Je¡erson University, Philadelphia, Pennsylvania, U.S.A. The 42nd Annual Symposium on the Biology of the this meeting just caught the wave of early pioneering Skin, entitled ‘‘The Genetics of Skin Disease’’, was held studies that have helped us to understand the molecular in Snowmass Village, Colorado, in July 1993. That meet- basis of a large number of genodermatoses. This over- ing presented the opportunity to discuss how modern view presented in the 50th Annual Symposium on the approaches to molecular genetics and molecular biol- biology of the skin, highlights the progress made in ogy could be applied to understanding the mechanisms the molecular genetics of heritable skin diseases over of skin diseases. The published proceedings of this the past decade. Key words: Genodermatoses/epidermolysis meeting stated that ‘‘It is an opportune time to examine bullosa/pseudoxanthoma elasticum JID Symposium Proceed- the genetics of skin disease’’ (Norris et al, 1994). Indeed, ings 7:6^16,2002 he recent progress made in molecular genetics of the basis of clinical, histopathologic, immunohistochemical, and/ heritable skin diseases is abundantly evident from or ultrastructural analysis, to serve as candidate gene/protein sys- the present vantage point, as reviewed in the 50th tems. For example, in the case of EB, we initially postulated that Annual Montagna Symposium on the Biology of mutations in the structural genes expressed within the cutaneous Skin, also held in Snowmass Village, Colorado, in basement membrane zone (BMZ) could harbor mutations that TJuly 2001. -

Waardenburg Syndrome
PHOTO QUIZ What Is Your Diagnosis? Figure not available online This patient has a daughter with partial deafness. PLEASE TURN TO PAGE 45 FOR DISCUSSION Dirk M. Elston, MD, Departments of Dermatology and Laboratory Medicine, Geisinger Medical Center, Danville, Pennsylvania. 20 CUTIS® Photo Quiz Discussion The Diagnosis: Waardenburg Syndrome Figure not available online aardenburg syndrome is an autosomal- inner canthi is characteristic of Waardenburg syn- dominant disorder that affects 1 in 40,000 drome type I; normally located inner canthi are W individuals and accounts for more than characteristic of type II.6 Type III represents an 2% of cases of congenital deafness.1 Manifestations extreme presentation of type I with arm abnormali- include lateral displacement of the inner canthi; ties. Most patients with Waardenburg syndrome heterochromia of the irides; white forelock; and type III are homozygous for the trait.7 Patients with other sites of poliosis, piebaldism, and sensorineural Waardenburg syndrome type IV have an absence of deafness. Expression of the disease is variable, even colonic ganglia (Hirschsprung disease).8 between monozygotic twins.2 Partial anodontia, Waardenburg syndrome is the most common myelomeningocele, facial palsy, and lingua plicata syndromal cause of deafness.9 Most affected individ- have been reported.3-5 Lateral displacement of the uals probably have some inner ear abnormalities, but the incidence of clinically apparent hearing 10 The author reports no conflict of interest. loss is highly variable. Children with this condi- The images are in the public domain. tion should be evaluated early because hearing loss VOLUME 73, JANUARY 2004 45 Photo Quiz Discussion may result in poor performance in school. -
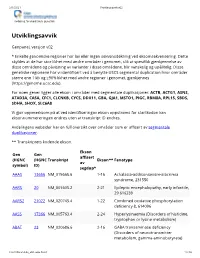
Utviklingsavvik V02
2/1/2021 Utviklingsavvik v02 Avdeling for medisinsk genetikk Utviklingsavvik Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). For noen gener ligger alle ekson i områder med segmentale duplikasjoner: ACTB, ACTG1, ASNS, ATAD3A, CA5A, CFC1, CLCNKB, CYCS, DDX11, GBA, GJA1, MSTO1, PIGC, RBM8A, RPL15, SBDS, SDHA, SHOX, SLC6A8 Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* AAAS 13666 NM_015665.6 1-16 Achalasia-addisonianism-alacrimia syndrome, 231550 AARS 20 NM_001605.2 2-21 Epileptic encephalopathy, early infantile, 29 616339 AARS2 21022 NM_020745.4 1-22 Combined oxidative phosphorylation deficiency 8, 614096 AASS 17366 NM_005763.4 2-24 Hyperlysinaemia (Disorders of histidine, tryptophan or lysine metabolism) ABAT 23 NM_020686.6 2-16 GABA transaminase deficiency (Disorders of neurotransmitter metabolism, gamma-aminobutyrate) -

MITF Gene Melanocyte Inducing Transcription Factor
MITF gene melanocyte inducing transcription factor Normal Function The MITF gene provides instructions for making a protein called melanocyte inducing transcription factor. This protein plays a role in the development, survival, and function of certain types of cells. To carry out this role, the protein attaches to specific areas of DNA and helps control the activity of particular genes. On the basis of this action, the protein is called a transcription factor. Melanocyte inducing transcription factor helps control the development and function of pigment-producing cells called melanocytes. Within these cells, this protein controls production of the pigment melanin, which contributes to hair, eye, and skin color. Melanocytes are also found in the inner ear and play an important role in hearing. Additionally, melanocyte inducing transcription factor regulates the development of specialized cells in the eye called retinal pigment epithelial cells. These cells nourish the retina, the part of the eye that detects light and color. Some research indicates that melanocyte inducing transcription factor also regulates the development of cells that break down and remove bone (osteoclasts) and cells that play a role in allergic reactions (mast cells). The structure of melanocyte inducing transcription factor includes three critically important regions. Two of the regions, called the helix-loop-helix motif and the leucine- zipper motif, are critical for protein interactions. These motifs allow molecules of melanocyte inducing transcription factor to interact with each other or with other proteins that have a similar structure, creating a two-protein unit (dimer) that functions as a transcription factor. The other region, known as the basic motif, binds to specific areas of DNA, allowing the dimer to control gene activity.