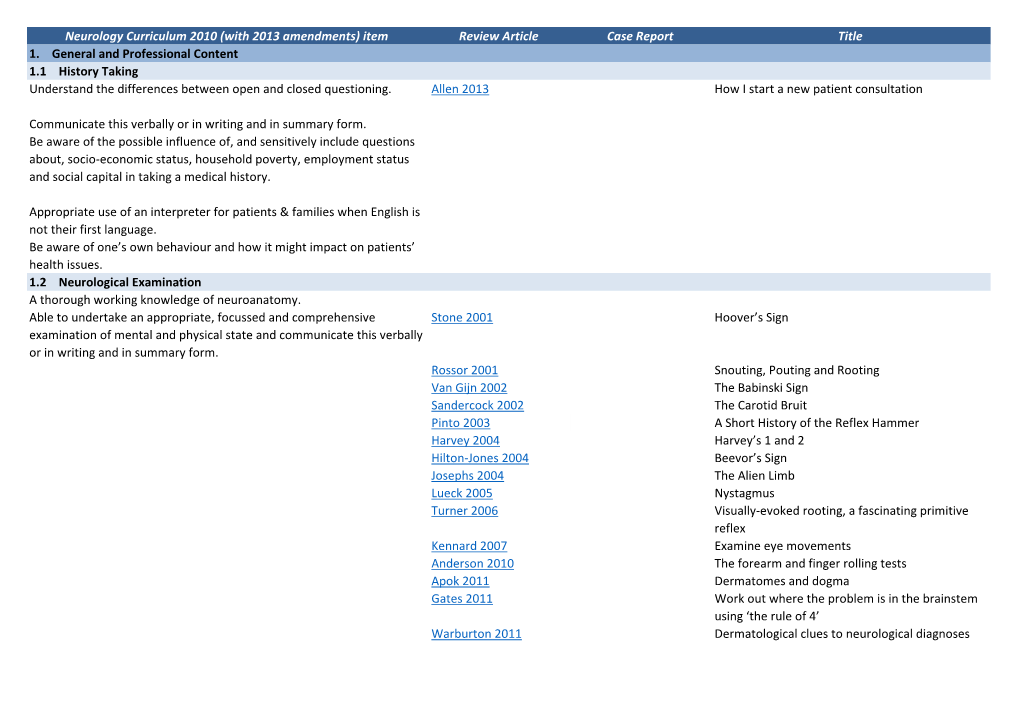
Neurology Curriculum 2010 (With 2013 Amendments) Item Review Article Case Report Title 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

107Th ENMC International Workshop: the Management of Cardiac Involvement in Muscular Dystrophy and Myotonic Dystrophy
Neuromuscular Disorders 13 (2003) 166–172 www.elsevier.com/locate/nmd Workshop report 107th ENMC International Workshop: the management of cardiac involvement in muscular dystrophy and myotonic dystrophy. 7th–9th June 2002, Naarden, the Netherlands K. Bushby*, F. Muntoni, J.P. Bourke Department of Neuromuscular Genetics, Institute of Human Genetics, International Centre for Life, Central Parkway, Newcastle upon Tyne NE1 3BZ, UK Received 1 August 2002; accepted 16 August 2002 1. Introduction symptomatic presentation [13,14]. Although evidence in these rare conditions of the effect of treatment is lacking Sixteen participants from Austria, France, Germany, [15], extrapolation from other conditions causing heart fail- Italy, the Netherlands and the UK met to discuss the cardiac ure with dilated cardiomyopathy means that there is a strong implications of the diagnosis of muscular dystrophy and case for the use of ACE inhibitors and potentially also beta myotonic dystrophy. The group included both myologists blockers, certainly in the presence of detectable abnormal- and cardiologists from nine different European centers. The ities and possibly preventatively [16–25]. aims of the workshop were to agree and report minimum The recommendations of the group are as follows. recommendations for the investigation and treatment of cardiac involvement in muscular and myotonic dystrophies, 2.1. DMD and define areas where further research is needed. During the workshop, all participants contributed to a review and † Patients should have a cardiac investigation (echo and assessment of the published evidence in each area and electrocardiogram (ECG)) at diagnosis. current practice amongst the group. Consensus statements † DMD patients should have cardiac investigations before for the management of dystrophinopathy, myotonic dystro- any surgery, every 2 years to age 10 and annually after phy, limb-girdle muscular dystrophy, Emery Dreifuss age 10. -

The Limb-Girdle Muscular Dystrophies and the Dystrophinopathies Review Article
Review Article 04/25/2018 on mAXWo3ZnzwrcFjDdvMDuzVysskaX4mZb8eYMgWVSPGPJOZ9l+mqFwgfuplwVY+jMyQlPQmIFeWtrhxj7jpeO+505hdQh14PDzV4LwkY42MCrzQCKIlw0d1O4YvrWMUvvHuYO4RRbviuuWR5DqyTbTk/icsrdbT0HfRYk7+ZAGvALtKGnuDXDohHaxFFu/7KNo26hIfzU/+BCy16w7w1bDw== by https://journals.lww.com/continuum from Downloaded Downloaded from Address correspondence to https://journals.lww.com/continuum Dr Stanley Jones P. Iyadurai, Ohio State University, Wexner The Limb-Girdle Medical Center, Department of Neurology, 395 W 12th Ave, Columbus, OH 43210, Muscular Dystrophies and [email protected]. Relationship Disclosure: by mAXWo3ZnzwrcFjDdvMDuzVysskaX4mZb8eYMgWVSPGPJOZ9l+mqFwgfuplwVY+jMyQlPQmIFeWtrhxj7jpeO+505hdQh14PDzV4LwkY42MCrzQCKIlw0d1O4YvrWMUvvHuYO4RRbviuuWR5DqyTbTk/icsrdbT0HfRYk7+ZAGvALtKGnuDXDohHaxFFu/7KNo26hIfzU/+BCy16w7w1bDw== Dr Iyadurai has received the Dystrophinopathies personal compensation for serving on the advisory boards of Allergan; Alnylam Stanley Jones P. Iyadurai, MSc, PhD, MD; John T. Kissel, MD, FAAN Pharmaceuticals, Inc; CSL Behring; and Pfizer, Inc. Dr Kissel has received personal ABSTRACT compensation for serving on a consulting board of AveXis, Purpose of Review: The classic approach to identifying and accurately diagnosing limb- Inc; as journal editor of Muscle girdle muscular dystrophies (LGMDs) relied heavily on phenotypic characterization and & Nerve; and as a consultant ancillary studies including muscle biopsy. Because of rapid advances in genetic sequencing for Novartis AG. Dr Kissel has received research/grant methodologies, -
Clinical Variability in Calpainopathy: What Makes the Difference?
European Journal of Human Genetics (2002) 10, 825 – 832 ª 2002 Nature Publishing Group All rights reserved 1018 – 4813/02 $25.00 www.nature.com/ejhg ARTICLE Clinical variability in calpainopathy: What makes the difference? Fla´via de Paula1, Mariz Vainzof1, Maria Rita Passos-Bueno1, Rita de Ca´ssia M Pavanello1, Sergio Russo Matioli1, Louise VB Anderson3, Vincenzo Nigro2 and Mayana Zatz*,1 1Human Genome Research Center-Departamento de Biologia, IB Universidade de Sa˜o Paulo, Brazil; 2TIGEM and Dipartimento di Patologia Generale, Seconda Universita’degli studi di Napoli, Italy; 3Neurobiology Department, University Medical School, Framlington Place, Newcastle upon Tyne, UK Limb girdle muscular dystrophies (LGMD) are a heterogeneous group of genetic disorders characterised by progressive weakness of the pelvic and shoulder girdle muscles and a great variability in clinical course. LGMD2A, the most prevalent form of LGMD, is caused by mutations in the calpain-3 gene (CAPN- 3). More than 100 pathogenic mutations have been identified to date, however few genotype : phenotype correlation studies, including both DNA and protein analysis, have been reported. In this study we screened 26 unrelated LGMD2A Brazilian families (75 patients) through Single-Stranded Conformation Polymorphism (SSCP), Denaturing high-performance liquid chromatography (DHPLC) and sequencing of abnormal fragments which allowed the identification of 47 mutated alleles (approximately 90%). We identified two recurrent mutations (R110X and 2362-2363AG4TCATCT) and seven novel pathogenic mutations. Interestingly, 41 of the identified mutations (approximately 80%) were concentrated in only 6 exons (1, 2, 4, 5, 11 and 22), which has important implications for diagnostic purposes. Protein analysis, performed in 28 patients from 25 unrelated families showed that with exception of one patient (with normal/slight borderline reduction of calpain) all others had total or partial calpain deficiency. -

Calcium Mechanisms in Limb-Girdle Muscular Dystrophy with CAPN3 Mutations
International Journal of Molecular Sciences Review Calcium Mechanisms in Limb-Girdle Muscular Dystrophy with CAPN3 Mutations Jaione Lasa-Elgarresta 1,2, Laura Mosqueira-Martín 1,2, Neia Naldaiz-Gastesi 1,2, Amets Sáenz 1,2, Adolfo López de Munain 1,2,3,4,* and Ainara Vallejo-Illarramendi 1,2,5,* 1 Biodonostia, Neurosciences Area, Group of Neuromuscular Diseases, 20014 San Sebastian, Spain; [email protected] (J.L.-E.); [email protected] (L.M.-M.); [email protected] (N.N.-G.); [email protected] (A.S.) 2 CIBERNED, Instituto de Salud Carlos III, Ministry of Science, Innovation and Universities, 28031 Madrid, Spain 3 Departmento de Neurosciencias, Universidad del País Vasco UPV/EHU, 20014 San Sebastian, Spain 4 Osakidetza Basque Health Service, Donostialdea Integrated Health Organisation, Neurology Department, 20014 San Sebastian, Spain 5 Grupo Neurociencias, Departmento de Pediatría, Hospital Universitario Donostia, UPV/EHU, 20014 San Sebastian, Spain * Correspondence: [email protected] (A.L.d.M.); [email protected] (A.V.-I.); Tel.: +34-943-006294 (A.L.d.M.); +34-943-006128 (A.V.-I.) Received: 4 August 2019; Accepted: 11 September 2019; Published: 13 September 2019 Abstract: Limb-girdle muscular dystrophy recessive 1 (LGMDR1), previously known as LGMD2A, is a rare disease caused by mutations in the CAPN3 gene. It is characterized by progressive weakness of shoulder, pelvic, and proximal limb muscles that usually appears in children and young adults and results in loss of ambulation within 20 years after disease onset in most patients. The pathophysiological mechanisms involved in LGMDR1 remain mostly unknown, and to date, there is no effective treatment for this disease. -

The Congenital and Limb-Girdle Muscular Dystrophies Sharpening the Focus, Blurring the Boundaries
NEUROLOGICAL REVIEW SECTION EDITOR: DAVID E. PLEASURE, MD The Congenital and Limb-Girdle Muscular Dystrophies Sharpening the Focus, Blurring the Boundaries Janbernd Kirschner, MD; Carsten G. Bo¨nnemann, MD uring the past decade, outstanding progress in the areas of congenital and limb- girdle muscular dystrophies has led to staggering clinical and genetic complexity. With the identification of an increasing number of genetic defects, individual enti- ties have come into sharper focus and new pathogenic mechanisms for muscular dys- Dtrophies, like defects of posttranslational O-linked glycosylation, have been discovered. At the same time, this progress blurs the traditional boundaries between the categories of congenital and limb- girdle muscular dystrophies, as well as between limb-girdle muscular dystrophies and other clini- cal entities, as mutations in genes such as fukutin-related protein, dysferlin, caveolin-3 and lamin A/C can cause a striking variety of phenotypes. We reviewed the different groups of proteins cur- rently recognized as being involved in congenital and limb-girdle muscular dystrophies, associ- ated them with the clinical phenotypes, and determined some clinical and molecular clues that are helpful in the diagnostic approach to these patients. Arch Neurol. 2004;61:189-199 Muscular dystrophies were first recog- phy. The age at onset may range from early nized as a disease entity with the detailed childhood to late adulthood.5 description of the clinical presentation of During the past decade, exciting Duchenne muscular dystrophy in 1852 and progress has been made in the field of CMD thereafter.1,2 About 50 years later, Batten3 and LGMD, emphasizing differences as published the first case reports of a con- well as commonalities between them. -

ACTA MYOLOGICA (Myopathies, Cardiomyopathies and Neuromyopathies)
ISSN 1128-2460 AC T Established in 1982 as Cardiomyology A M YOLOGICA ACTA MYOLOGICA (Myopathies, Cardiomyopathies and Neuromyopathies) Vol. XXXIII - May 2014 Official Journal of CB PISA D Mediterranean Society of Myology and Associazione Italiana di Miologia Founders: Giovanni Nigro and Lucia Ines Comi VOL. XXXIII N. 1 - 2014 XXXIII N. VOL. Four-monthly EDITOR-IN-CHIEF Giovanni Nigro ASSISTANT EDITOR managing EDITOR .L. 353/2003 conv. in L. 27/02/2004 n° 46 art. 1, comma 1, comma 1, 27/02/2004 1, in L. n° 46 art. 353/2003 .L. conv. D Vincenzo Nigro Luisa Politano CO-EDITORS Valerie Askanas Giuseppe Novelli Lefkos Middleton Reinhardt Rüdel HISTORical STUDIES EDITOR Georges Serratrice ALIANE SPA - Spedizione in Abbonamento Postale - Postale Abbonamento - Spedizione in ALIANE SPA T E I T POS Official Journal of Mediterranean Society of Myology and Associazione Italiana di Miologia Founders: Giovanni Nigro and Lucia Ines Comi Four-monthly EDITORIAL BOARD Ekram Abdel-Salam, Cairo Clemens Müller, Würzburg Corrado Angelini, Padova Francesco Muntoni, Londra Enrico Bertini, Roma Carmen Navarro, Vigo Serge Braun, Paris Gerardo Nigro, Napoli Kate Bushby, Newcastle upon Tyne Anders Oldfors, Göteborg Kevin P. Campbell, Iowa City Eijiro Ozawa, Tokyo Marinos Dalakas, Athens Heinz Reichmann, Dresden Feza Deymeer, Instanbul Serenella Servidei, Roma Salvatore Di Mauro, New York Piraye Serdaroglu, Instanbul Denis Duboc, Paris Yeuda Shapira, Jerusalem Victor Dubowitz, London Osman I. Sinanovic, Tuzla King W. Engel, Los Angeles Michael Sinnreich, Montreal Michel Fardeau, Paris Andoni J. Urtizberea, Hendaye Irena Hausmanowa-Petrusewicz, Warszawa Gert-Jan van Ommen, Leiden Fayçal Hentati, Tunis Lord John Walton of Detchant, Oxford Byron A. -
Noncyclic Chronic Pelvic Pain Therapies for Women: Comparative Effectiveness Comparative Effectiveness Review Number 41
Comparative Effectiveness Review Number 41 Noncyclic Chronic Pelvic Pain Therapies for Women: Comparative Effectiveness Comparative Effectiveness Review Number 41 Noncyclic Chronic Pelvic Pain Therapies for Women: Comparative Effectiveness Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. 290-2007-10065-I Prepared by: Vanderbilt Evidence-based Practice Center Nashville, Tennessee Investigators: Jeff Andrews, M.D. Amanda Yunker, D.O., M.S.C.R. W. Stuart Reynolds, M.D. Frances E. Likis, Dr.P.H., N.P., C.N.M. Nila A. Sathe, M.A., M.L.I.S. Rebecca N. Jerome, M.L.I.S., M.P.H. AHRQ Publication No. 11(12)-EHC088-EF January 2012 This report is based on research conducted by the Vanderbilt Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. HHSA 290-2007-10065-I). The findings and conclusions in this document are those of the authors, who are responsible for its contents; the findings and conclusions do not necessarily represent the views of AHRQ. Therefore, no statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help health care decisionmakers—patients and clinicians, health system leaders, and policymakers, among others—make well-informed decisions and thereby improve the quality of health care services. This report is not intended to be a substitute for the application of clinical judgment. -

Mutational Spectrum of Autosomal Recessive Limb-Girdle Muscular Dystrophies in a Cohort of 112 Iranian Patients and Reporting Of
CORE Metadata, citation and similar papers at core.ac.uk Provided by eprints Iran University of Medical Sciences Mojbafan et al. Orphanet Journal of Rare Diseases (2020) 15:14 https://doi.org/10.1186/s13023-020-1296-x RESEARCH Open Access Mutational spectrum of autosomal recessive limb-girdle muscular dystrophies in a cohort of 112 Iranian patients and reporting of a possible founder effect Marzieh Mojbafan1,2, Reza Bahmani1,3, Samira Dabbagh Bagheri4, Zohreh Sharifi4,5 and Sirous Zeinali4,6* Abstract Background: Limb-girdle muscular dystrophies are a group of genetically heterogeneous diseases that are inherited in both autosomal dominant (LGMDD) and autosomal recessive forms (LGMDR), the latter is more common especially in populations with high consanguineous marriages like Iran. In the present study, we aimed to investigate the genetic basis of patients who are suspicious of being affected by LGMDR. DNA samples of 60 families suspected of LGMD were extracted from their whole blood. Four short tandem repeat (STR) markers for each candidate genes related to LGMD R1 (calpain3 related)- R6 (δ-sarcoglycan-related) were selected, and all these 24 STRs were applied in two sets of multiplex PCR. After autozygosity mapping, Sanger sequencing and variant analysis were done. Predicting identified variants’ effect was performed using in-silico tools, and they were interpreted according to the American College of Medical Genomics and Genetics (ACMG) guideline. MLPA was used for those patients who had large deletions. Fresh muscle specimens were taken from subjects and were evaluated using the conventional panel of histochemical stains. Results: forty out of sixty families showed homozygote haplotypes in CAPN3, DYSF, SGCA, and SGCB genes. -

Clinical and Genomic Evaluation of 207 Genetic Myopathies in the Indian Subcontinent
medRxiv preprint doi: https://doi.org/10.1101/2020.09.15.20193425; this version posted September 18, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Clinical and Genomic Evaluation of 207 Genetic Myopathies in the Indian Subcontinent 1 Samya Chakravorty1, 2, 3, 4, *, Babi Ramesh Reddy Nallamilli5, Satish Khadilkar6, 7, 8, 2 Madhubala Singla6, 7, 8, Ashish Bhutada6, Rashna Dastur9, Pradnya Gaitonde9, Laura 3 Rufibach10, Logan Gloster1, 4, Madhuri Hegde4, 5,* 4 5 1 Emory University Department of Pediatrics, Atlanta, GA, USA 6 2 Emory University Department of Human Genetics, Atlanta, GA, USA 7 3 Division of Neurosciences, Children’s Healthcare of Atlanta, GA, USA 8 4 School of Biological Sciences, Georgia Institute of Technology, Atlanta, GA, USA 9 5 PerkinElmer Genomics, Global Laboratory Services, Waltham, MA, USA. 10 6 Department of Neurology, Bombay Hospital, Mumbai, Maharashtra, India 11 7 Department of Neurology, Sir J J Group of Hospitals, Grant Medical College, Mumbai, 12 Maharashtra, India 13 8 Bombay Hospital Institute of Medical Sciences, Mumbai, Maharashtra, India 14 9 Centre for Advanced Molecular Diagnostics in Neuromuscular Disorders (CAMDND) Mumbai, 15 Maharashtra, India 16 10 Jain Foundation, Seattle, WA, USA 98115 17 18 19 * Correspondence: 20 21 Samya Chakravorty 22 [email protected] 23 24 Madhuri Hegde 25 [email protected] 26 27 Lead Contact: Samya Chakravorty ([email protected]) 28 29 Manuscript word count: 5507, Number of Figures: 3, Number of Tables: 6 30 31 Keywords: Inherited Myopathies, LGMD, Exome Sequencing, Next Generation Sequencing, 32 Molecular Diagnostics, India 33 NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. -
Camptocormia As the Presenting Symptom in Sporadic Late Onset Nemaline Myopathy: a Case Report Matthias Türk1* , Armin M
Türk et al. BMC Musculoskeletal Disorders (2019) 20:553 https://doi.org/10.1186/s12891-019-2942-0 CASE REPORT Open Access Camptocormia as the presenting symptom in sporadic late onset nemaline myopathy: a case report Matthias Türk1* , Armin M. Nagel2, Frank Roemer3, Ursula Schlötzer-Schrehardt4, Christian T. Thiel5, Martin Winterholler6 and Rolf Schröder7 Abstract Background: Camptocormia has been reported in a plethora of diseases comprising disorders of the central nervous system, the peripheral nervous system, and the neuromuscular junction as well as hereditary and acquired myopathies. In sporadic late onset nemaline myopathy concomitant axial myopathy is common, but reports about camptocormia as the only presenting symptom in this condition are very rare. Notably, sporadic late onset nemaline myopathy is a potentially treatable condition in particular when associated with monoclonal gammopathy of unknown significance, HIV or rheumatological disorders. Case presentation: We report the case of a 62-year-old female patient, who presented with slowly progressive camptocormia. Comprehensive work-up including neurological work-up, laboratory tests, MR-imaging, muscle biopsy and genetic testing led to the diagnosis of sporadic late onset nemaline myopathy. Conclusions: Our case report highlights that sporadic late onset nemaline myopathy has to be considered in patients presenting with isolated camptocormia and comprehensive work-up of camptocormia is mandatory to ascertain the individual diagnosis, especially in consideration of treatable conditions. Keywords: Camptocormia, Axial myopathy, Muscle biopsy, Nemaline rods, Sporadic late onset nemaline myopathy, SLONM Background humeral muscle dystrophy, myotonic dystrophy type I/II, Camptocormia is characterized by involuntary forward dysferlinopathy, calpainopathy, myofibrillar myopathies) and flexion of the thoracolumbar spine. -

Molecular and Cellular Basis of Calpainopathy (Limb Girdle Muscular Dystrophy Type 2A) ⁎ Irina Kramerova A, Jacques S
Biochimica et Biophysica Acta 1772 (2007) 128–144 www.elsevier.com/locate/bbadis Review Molecular and cellular basis of calpainopathy (limb girdle muscular dystrophy type 2A) ⁎ Irina Kramerova a, Jacques S. Beckmann b, Melissa J. Spencer a, a Departments of Neurology and Pediatrics and UCLA Duchenne Muscular Dystrophy Research Center, University of California, Los Angeles, Neuroscience Research Building, 635 Young Dr. South, Los Angeles, CA 90095-7334, USA b Department of Medical Genetics, Faculty of Medicine, University of Lausanne, Lausanne, Switzerland Received 26 May 2006; received in revised form 7 July 2006; accepted 13 July 2006 Available online 15 July 2006 Abstract Limb girdle muscular dystrophy type 2A results from mutations in the gene encoding the calpain 3 protease. Mutations in this disease are inherited in an autosomal recessive fashion and result in progressive proximal skeletal muscle wasting but no cardiac abnormalities. Calpain 3 has been shown to proteolytically cleave a wide variety of cytoskeletal and myofibrillar proteins and to act upstream of the ubiquitin-proteasome pathway. In this review, we summarize the known biochemical and physiological features of calpain 3 and hypothesize why mutations result in disease. © 2006 Elsevier B.V. All rights reserved. Keywords: Calpain; Dystrophy; Muscle; Dysferlin; Titin Most autosomal recessive limb girdle muscular dystrophies dystrophin–glycoprotein complex (DGC), since all previously (LGMD) are due to mutations in genes encoding structural identified dystrophies had been shown to have some relation- proteins that make up the cytoskeletal scaffold of muscle. These ship to these proteins. The possible link to the DGC remains, LGMDs are slowly progressive and involve wasting in the however, cryptic. -

Diagnosis and Treatment of Limb-Girdle Muscular Dystrophy
Practice Guideline American Association of Neuromuscular & Electrodiagnostic Medicine EVIDENCE-BASED GUIDELINE: DIAGNOSIS AND TREATMENT OF LIMB-GIRDLE AND DISTAL DYSTROPHIES Report of the Guideline Development Subcommittee of the American Academy of Neurology and the Practice Issues Review Panel of the American Association of Neuromuscular & Electrodiagnostic Medicine Pushpa Narayanaswami, MBBS, DM, FAAN1; Michael Weiss, MD, FAAN2; Duygu Selcen, MD3; William David, MD, PhD4; Elizabeth Raynor, MD1; Gregory Carter, MD5; Matthew Wicklund, MD, FAAN6; Richard J. Barohn, MD, FAAN7; Erik Ensrud, MD8,10; Robert C. Griggs, MD, FAAN9; Gary Gronseth, MD, FAAN7; Anthony A. Amato, MD, FAAN10 (1) Department of Neurology, Beth Israel Deaconess Medical Center/Harvard Medical School, Boston, MA (2) Department of Neurology, University of Washington Medical Center, Seattle, WA (3) Department of Neurology, Mayo Clinic, Rochester, MN (4) Department of Neurology, Massachusetts General Hospital, Boston, MA/Harvard Medical School, Boston, MA (5) St Luke's Rehabilitation Institute, Spokane, WA (6) Department of Neurology, Penn State Hershey Medical Center, Hershey, PA (7) Department of Neurology, University of Kansas Medical Center, Kansas City, KS (8) Neuromuscular Center, Boston VA Medical Center, Boston, MA (9) Department of Neurology, University of Rochester Medical Center, Rochester, NY 1 (10) Department of Neurology, Brigham and Women’s Hospital, Boston, MA/Harvard Medical School, Boston, MA Correspondence to American Academy of Neurology: [email protected] Approved by the AAN Guideline Development Subcommittee on July 13, 2013; by the AAN Practice Committee on February 3, 2014; by the AANEM Board of Directors on July 10, 2014; and by the AANI Board of Directors on July 7, 2014.