New Drug Evaluation Monograph Template
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Anthem Blue Cross Drug Formulary
Erythromycin/Sulfisoxazole (generic) INTRODUCTION Penicillins ...................................................................... Anthem Blue Cross uses a formulary Amoxicillin (generic) (preferred list of drugs) to help your doctor Amoxicillin/Clavulanate (generic/Augmentin make prescribing decisions. This list of drugs chew/XR) is updated quarterly, by a committee Ampicillin (generic) consisting of doctors and pharmacists, so that Dicloxacillin (generic) the list includes drugs that are safe and Penicillin (generic) effective in the treatment of diseases. If you Quinolones ..................................................................... have any questions about the accessibility of Ciprofloxacin/XR (generic) your medication, please call the phone number Levofloxacin (Levaquin) listed on the back of your Anthem Blue Cross Sulfonamides ................................................................ member identification card. Erythromycin/Sulfisoxazole (generic) In most cases, if your physician has Sulfamethoxazole/Trimethoprim (generic) determined that it is medically necessary for Sulfisoxazole (generic) you to receive a brand name drug or a drug Tetracyclines .................................................................. that is not on our list, your physician may Doxycycline hyclate (generic) indicate “Dispense as Written” or “Do Not Minocycline (generic) Substitute” on your prescription to ensure Tetracycline (generic) access to the medication through our network ANTIFUNGAL AGENTS (ORAL) _________________ of community -
2021 National Formulary 3Rd Quarter Edition
2021 National Formulary 3rd Quarter Edition Last Revised: 08/18/2021 Version 2021Q3c Table of Contents OVERVIEW 4 CARDIOVASCULAR (HEART) DRUGS 14 Alpha & Beta Blockers 14 COVERAGE LIMITATION 4 Antihypertensive Combinations 14 Calcium Channel Blockers (CCBs) 14 COMPOUNDED DRUGS 4 ACE Inhibitors without & with Diuretics 15 DRUG PLACEMENT DETERMINATION 4 ACE Inhibitors / CCB Combinations 15 ARBs without & with Diuretics 15 PREFERRED BRAND PRODUCTS 5 ARB Combinations 15 Naprilysin Inhibitors 15 GENERIC SUBSTITUTION 5 Diuretics 15 Renin Inhibtors 16 SINGLE & DUAL SOURCE GENERICS 5 Antiarrhythmics/Anti-Ischemic 16 Cardiac Glycosides 16 PRIOR AUTHORIZATIONS, STEP EDITS & QTY LIMITS 6 Vasodilators, Coronary, Nitrates/Vasodilators, Sympatholytics 16 EXCLUDED DRUGS 6 Other Drugs 16 NON-LISTED DRUGS & DRUG CATEGORIES 7 ANTIHYPERLIPIDEMIC (CHOLESTEROL) DRUGS 17 Statins & Statin/CCB Combinations 17 FORMULARY MODIFICATIONS & CHANGES 7 Bile Acid Sequestrants, Liver Drugs 17 Fibrates 17 BIOSIMILARS 7 ACL Inhibitors 17 Other Drugs 17 MAJOR CHANGES TO THE PDL 7 PANCREATIC DRUGS 18 ANTIBIOTICS 8 Penicillins & Cephalosporins 8 KIDNEY & URINARY / UROLOGICAL DRUGS 18 Tetracyclines 8 Benign Prostate Hyperplasia 18 Macrolides & Clindamycins 8 Urologic Drugs / Other Drugs 18 Sulfonamides, Sulfones & Ketolides 8 Erectile Dysfunction Drugs 18 Quinolones 8 Gout Drugs – Purine Inhibitors 19 Miscellaneous Antibiotics 8 Urinary Ph Modifiers 19 Potassium & Electrolytes 19 ANTI-VIRALS 9 Phosphorus/Calcium/Electrolyte Depleters 19 General Antivirals 9 HIV Antiviral Drugs 9 OSTEOPOROSIS (BONE) DRUGS 20 HIV Pre-Exposure Propylaxis Drugs 9 ANTI-INFLAMMATORY / ANALGESIC (PAIN) DRUGS 20 ANTI-INFECTIVES 10 Anti-Inflammatory Drugs (NSAIDS) 20 Anaerobic Anti-Infectives 10 COX-II Drugs 21 Antiparasitics 10 Analgesics, Narcotics (Opioids) 21 Antimalarials & Antiprotozoals 10 Analgesics, Salicylates, Non-Salicylates, Other 21 Antihelmintic Drugs 10 CENTRAL NERVOUS SYSTEM DRUGS 22 ANTIEMETICS 10 Anti-Anxiety Drugs (Benzodiazepines) 22 Sedative/Sleeping Drugs 22 NEUROLOGIC DRUGS 11 A.D.D. -

Estradiol Acetate Vaginal Ring) Rx Only
NDA 21-367/S-002 Page 3 PRESCRIBING INFORMATION Femring® (estradiol acetate vaginal ring) Rx Only ESTROGENS INCREASE THE RISK OF ENDOMETRIAL CANCER Close clinical surveillance of all women taking estrogens is important. Adequate diagnostic measures, including endometrial sampling when indicated, should be undertaken to rule out malignancy in all cases of undiagnosed persistent or recurring abnormal vaginal bleeding. There is no evidence that the use of “natural” estrogens results in a different endometrial risk profile than synthetic estrogens at equivalent estrogen doses. (See WARNINGS, Malignant neoplasms, Endometrial cancer.) CARDIOVASCULAR AND OTHER RISKS Estrogens with or without progestins should not be used for the prevention of cardiovascular disease or dementia. (See WARNINGS, Cardiovascular disorders and Dementia.) The Women’s Health Initiative (WHI) study reported increased risks of myocardial infarction, stroke, invasive breast cancer, pulmonary emboli, and deep vein thrombosis in postmenopausal women (50 to 79 years of age) during 5 years of treatment with oral conjugated estrogens (CE 0.625 mg) combined with medroxyprogesterone acetate (MPA 2.5 mg) relative to placebo. (See CLINICAL PHARMACOLOGY, Clinical Studies and WARNINGS, Cardiovascular disorders and Malignant neoplasms, Breast cancer.) The Women’s Health Initiative Memory Study (WHIMS), a substudy of WHI, reported increased risk of developing probable dementia in postmenopausal women 65 years of age or older during 4 years of treatment with oral conjugated estrogens -

Eraas for Menopause Treatment: Welcome the ‘Designer Estrogens’
REVIEW CME LEARNING OBJECTIVE: Readers will tailor hormone therapy to the needs of the patient CREDIT HEATHER D. HIRSCH, MD, MS, NCMP ELIM SHIH, MD, NCMP HOLLY L. THACKER, MD, NCMP Assistant Professor, Clinical Internal Medicine, Division Department of Obstetrics and Gynecology, Director of Center for Specialized Women’s Health, of General Internal Medicine, The Ohio State University, Women’s Health Institute, Cleveland Clinic Department of Obstetrics and Gynecology, Women’s Columbus, and Center for Women’s Health, Health Institute, Cleveland Clinic; Professor, Cleveland The Ohio State University Wexner Medical Center, Clinic Lerner College of Medicine of Case Western Upper Arlington, OH Reserve University, Cleveland, OH ERAAs for menopause treatment: Welcome the ‘designer estrogens’ ABSTRACT strogen receptor agonist-antagonists E(ERAAs), previously called selective es- Estrogen receptor agonist-antagonists (ERAAs) selec- trogen receptor modulators (SERMs), have tively inhibit or stimulate estrogen-like action in targeted extended the options for treating the vari- tissues. This review summarizes how ERAAs can be used ous conditions that menopausal women suffer in combination with an estrogen or alone to treat meno- from. These drugs act differently on estrogen pausal symptoms (vasomotor symptoms, genitourinary receptors in different tissues, stimulating re- syndrome of menopause), breast cancer or the risk of ceptors in some tissues but inhibiting them breast cancer, osteopenia, osteoporosis, and other female in others. This allows selective inhibition or midlife concerns. stimulation of estrogen-like action in various target tissues.1 KEY POINTS This article highlights the use of ERAAs Tamoxifen is approved to prevent and treat breast cancer. to treat menopausal vasomotor symptoms It may also have beneficial effects on bone and on car- (eg, hot flashes, night sweats), genitourinary diovascular risk factors, but these are not approved uses. -
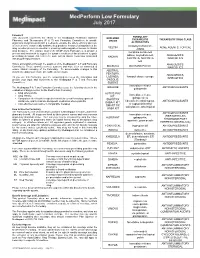
Medperform Low Formulary July 2017
MedPerform Low Formulary July 2017 Foreword FORMULARY This document represents the efforts of the MedImpact Healthcare Systems EXCLUDED THERAPEUTIC THERAPEUTIC DRUG CLASS Pharmacy and Therapeutics (P & T) and Formulary Committees to provide DRUGS physicians and pharmacists with a method to evaluate the safety, efficacy and cost- ALTERNATIVES effectiveness of commercially available drug products. A structured approach to the clindamycin/tretinoin, VELTIN ACNE AGENTS, TOPICAL drug selection process is essential in ensuring continuing patient access to rational ZIANA drug therapies. The ultimate goal of the MedPerform Formulary is to provide a morphine sulfate ER process and framework to support the dynamic evolution of this document to guide tablets, oxycodone ER, ANALGESICS, prescribing decisions that reflect the most current clinical consensus associated KADIAN with drug therapy decisions. NUCYNTA, NUCYNTA NARCOTICS ER This is accomplished through the auspices of the MedImpact P & T and Formulary ANALGESICS, BELBUCA BUTRANS PATCH Committees. These committees meet quarterly and more often as warranted to NARCOTICS ensure clinical relevancy of the Formulary. To accommodate changes to this ABSTRAL, document, updates are made accessible as necessary. FENTORA, ANALGESICS, LAZANDA, fentanyl citrate lozenge As you use this Formulary, you are encouraged to review the information and NARCOTICS provide your input and comments to the MedImpact P & T and Formulary ONSOLIS, Committees. SUBSYS immediate-release GRALISE ANTICONVULSANTS The MedImpact -

Printed Formulary Catalog Basic
Scripps Health Formulary July 2016 Foreword Pharmacy and Therapeutics Committee. MedImpact approves such multi- This document represents the efforts of the MedImpact Healthcare Systems source drugs for addition to the MAC list based on the following criteria: Pharmacy and Therapeutics (P & T) and Formulary Committees to provide physicians A multi-source drug product manufactured by at least one (1) nationally and pharmacists with a method to evaluate the safety, efficacy and cost-effectiveness marketed company. of commercially available drug products. A structured approach to the drug selection At least one (1) of the generic manufacturer’s products must have an “A” process is essential in ensuring continuing patient access to rational drug therapies. rating or the generic product has been determined to be unassociated with The ultimate goal of the Portfolio Formulary is to provide a process and framework to efficacy, safety or bioequivalency concerns by the MedImpact P & T support the dynamic evolution of this document to guide prescribing decisions that Committee. reflect the most current clinical consensus associated with drug therapy decisions. Drug product will be approved for generic substitution by the MedImpact P & T Committee. This is accomplished through the auspices of the MedImpact P & T and Formulary Committees. These committees meet quarterly and more often as warranted to ensure This list is reviewed and updated periodically based on the clinical literature and clinical relevancy of the Formulary. To accommodate changes to this document, pharmacokinetic characteristics of currently available versions of these drug updates are made accessible as necessary. products. As you use this Formulary, you are encouraged to review the information and provide If a member or physician requests a brand name product in lieu of an approved your input and comments to the MedImpact P & T and Formulary Committees. -

Estrogens, Estrogen Agonists/Antagonists, and Calcitonin Nelson B
48 Estrogens, Estrogen Agonists/Antagonists, and Calcitonin Nelson B. Watts Estrogen 408 Calcitonin 409 Estrogen Agonists/Antagonists (Selective Estrogen Receptor Summary 410 Modulators or Serms) 409 Selected Readings 410 Thus, it appears that estrogen has protective effects on ESTROGEN the skeleton only for as long as it is taken. However, women who take estrogen and then stop should be no It is well established that osteoporosis is more common worse off compared with women who have never taken in women than men and fracture risk increases dramati- estrogen at all. cally after menopause. The relationship between estro- Following results of the WHI, estrogen treatment is gen defi ciency and osteoporosis was fi rst suggested in the recommended for relief of menopausal symptoms, but in mid-1900s when Albright showed that treatment with the lowest dose and for the shortest time necessary. Most estrogen reversed the negative calcium balance in post- women are not suffi ciently symptomatic at menopause menopausal women. The positive effects of estrogen on to require estrogen therapy, and most who require estro- peak bone mass and on bone loss have been demon- gen will be able to stop after a few years. However, a strated in both men and women. For years, estrogen was minority will require estrogen long-term. For those considered the treatment of choice for postmenopausal women, estrogen may be suffi cient for prevention and/or women and widely advocated for prevention of bone loss, treatment of osteoporosis. with numerous trials showing prevention of bone loss Several different forms of estrogen are available for in recently menopausal women and increased of bone therapeutic use (e.g., estradiol, conjugated estrogen ester- mineral density (BMD) in women with postmenopausal ifi ed estrogens, etc.) as well as several routes of adminis- osteoporosis. -
Clinical Update on the Use of Ospemifene in the Treatment of Severe Symptomatic Vulvar and Vaginal Atrophy
Journal name: International Journal of Women’s Health Article Designation: Review Year: 2016 Volume: 8 International Journal of Women’s Health Dovepress Running head verso: Palacios and Cancelo Running head recto: The use of ospemifene in the treatment of severe symptomatic VVA open access to scientific and medical research DOI: http://dx.doi.org/10.2147/IJWH.S110035 Open Access Full Text Article REVIEW Clinical update on the use of ospemifene in the treatment of severe symptomatic vulvar and vaginal atrophy Santiago Palacios1 Abstract: The physiological decrease in vaginal estrogens is accountable for the emergence of María Jesús Cancelo2 vulvar and vaginal atrophy (VVA) and its related symptoms such as vaginal dryness, dyspareunia, vaginal and/or vulvar irritation or itching, and dysuria. The repercussion of these symptoms 1Palacios Institute of Women’s Health, Madrid, Spain; 2Gynecology and on quality of life often makes it necessary to initiate treatment. Up until now, the treatments Obstetrics Department, Guadalajara available included vaginal moisturizers and lubricants, local estrogens, and hormonal therapy. University Hospital, University of Alcalá, Spain However, therapeutic options have now been increased with the approval of 60 mg ospemifene, the first nonhormonal oral treatment with an agonist effect on the vaginal epithelium and an endometrial and breast safety profile which makes it unique. This is the first selective estrogen receptor modulator indicated in women with moderate-to-severe vaginal atrophy not eligible For personal use only. for local estrogen treatment. Considering that “local estrogen noneligible women” are those in whom such treatment cannot be administered either because it is contraindicated or due to skill issues, who are averse to the mode and convenience of vaginal products’ administration or to their use on account of potential systemic absorption, or those who demonstrate dissatisfac- tion in terms of efficacy and safety, it is clear that there is a significant unmet medical need in VVA management. -

Management of Women with Premature Ovarian Insufficiency
Management of women with premature ovarian insufficiency Guideline of the European Society of Human Reproduction and Embryology POI Guideline Development Group December 2015 1 Disclaimer The European Society of Human Reproduction and Embryology (hereinafter referred to as 'ESHRE') developed the current clinical practice guideline, to provide clinical recommendations to improve the quality of healthcare delivery within the European field of human reproduction and embryology. This guideline represents the views of ESHRE, which were achieved after careful consideration of the scientific evidence available at the time of preparation. In the absence of scientific evidence on certain aspects, a consensus between the relevant ESHRE stakeholders has been obtained. The aim of clinical practice guidelines is to aid healthcare professionals in everyday clinical decisions about appropriate and effective care of their patients. However, adherence to these clinical practice guidelines does not guarantee a successful or specific outcome, nor does it establish a standard of care. Clinical practice guidelines do not override the healthcare professional's clinical judgment in diagnosis and treatment of particular patients. Ultimately, healthcare professionals must make their own clinical decisions on a case-by-case basis, using their clinical judgment, knowledge, and expertise, and taking into account the condition, circumstances, and wishes of the individual patient, in consultation with that patient and/or the guardian or carer. ESHRE makes no warranty, express or implied, regarding the clinical practice guidelines and specifically excludes any warranties of merchantability and fitness for a particular use or purpose. ESHRE shall not be liable for direct, indirect, special, incidental, or consequential damages related to the use of the information contained herein. -

Ambetter 90-Day-Maintenance Drug List- 2020
Ambetter 90-Day-Maintenance Drug List Guide to this list: What is Ambetter 90‐Day‐Maintenance Drug List? Ambetter 90‐Day‐Supply Maintenance Drug List is a list of maintenance medications that are available for 90 day supply through mail order or through our Extended Day Supply Network. How do I find a pharmacy that is participating in Extended Day Supply Network? To find a retail pharmacy that is participating in our Extended Day Supply Network please consult information available under Pharmacy Resources tab on our webpage. Alternatively, you can utilize our mail order pharmacy. Information on mail order pharmacy is available in Pharmacy Resources tab on our webpage. Are all formulary drugs covered for 90 day supply? No, certain specialty and non‐specialty drugs are excluded from 90 day supply. Please consult 90‐Day‐ Supply Maintenance Drug List for information if your drug is included. A Amitriptyline HCl Acamprosate Calcium Amlodipine Besylate Acarbose Amlodipine Besylate-Atorvastatin Calcium Acebutolol HCl Amlodipine Besylate-Benazepril HCl Acetazolamide Amlodipine Besylate-Olmesartan Medoxomil Albuterol Sulfate Amlodipine Besylate-Valsartan Alendronate Sodium Amlodipine-Valsartan-Hydrochlorothiazide Alendronate Sodium-Cholecalciferol Amoxapine Alfuzosin HCl Amphetamine-Dextroamphetamine Aliskiren Fumarate Anagrelide HCl Allopurinol Anastrozole Alogliptin Benzoate Apixaban Alosetron HCl Arformoterol Tartrate Amantadine HCl Aripiprazole Amiloride & Hydrochlorothiazide Armodafinil Amiloride HCl Asenapine Maleate Amiodarone HCl Aspirin-Dipyridamole -

Hormonal and Non-Hormonal Management of Vasomotor Symptoms: a Narrated Review
Central Journal of Endocrinology, Diabetes & Obesity Review Article Corresponding authors Orkun Tan, Department of Obstetrics and Gynecology, Division of Reproductive Endocrinology Hormonal and Non-Hormonal and Infertility, University of Texas Southwestern Medical Center, 5323 Harry Hines Blvd. Dallas, TX 75390 and ReproMed Fertility Center, 3800 San Management of Vasomotor Jacinto Dallas, TX 75204, USA, Tel: 214-648-4747; Fax: 214-648-8066; E-mail: [email protected] Submitted: 07 September 2013 Symptoms: A Narrated Review Accepted: 05 October 2013 Orkun Tan1,2*, Anil Pinto2 and Bruce R. Carr1 Published: 07 October 2013 1Department of Obstetrics and Gynecology, Division of Reproductive Endocrinology Copyright and Infertility, University of Texas Southwestern Medical Center, USA © 2013 Tan et al. 2Department of Obstetrics and Gynecology, Division of Reproductive Endocrinology and Infertility, ReproMed Fertility Center, USA OPEN ACCESS Abstract Background: Vasomotor symptoms (VMS; hot flashes, hot flushes) are the most common complaints of peri- and postmenopausal women. Therapies include various estrogens and estrogen-progestogen combinations. However, both physicians and patients became concerned about hormone-related therapies following publication of data by the Women’s Health Initiative (WHI) study and have turned to non-hormonal approaches of varying effectiveness and risks. Objective: Comparison of the efficacy of non-hormonal VMS therapies with estrogen replacement therapy (ERT) or ERT combined with progestogen (Menopausal Hormone Treatment; MHT) and the development of literature-based guidelines for the use of hormonal and non-hormonal VMS therapies. Methods: Pubmed, Cochrane Controlled Clinical Trials Register Database and Scopus were searched for relevant clinical trials that provided data on the treatment of VMS up to June 2013. -

Table E-46. Therapies Used in Trials Comparing Hormone with Placebo Ar Est Study N Rxcat Dose Route Generic Trade M Dose Martin 1971 1 56 Plac Oral
Table E-46. Therapies used in trials comparing hormone with placebo Ar Est Study N RxCat Dose Route Generic Trade m Dose Martin 1971 1 56 Plac Oral Standar 2 53 EP seq 0.025 mg E + 1 mg P Oral mestranol + norethindrone d 3 56 EP seq 0.05 mg E + 1 mg P Oral mestranol + norethindrone High Campbell 1 68 Plac Oral 1977 2 68 Est 1.25 mg Oral conjugated equine estrogens Premarin High Baumgardner 1 42 Plac Oral 1978 2 42 Est 0.1 mg Oral quinestrol Estrovis Low Standar 3 35 Est 0.2 mg Oral quinestrol Estrovis d 4 37 Est 1.25 mg Oral conjugated estrogen Premarin High E-65 Ar Est Study N RxCat Dose Route Generic Trade m Dose Coope 1981 1 26 Plac Oral UltraLo 2 29 Est 0.3mg Oral piperazine estrone sulphate w Jensen 1983 1 90 Plac Oral estradiol + estriol + 2 41 EP seq 4 mg E + 1 mg P Oral Trisequens Forte High norethisterone acetate Foidart 1991 1 53 Plac VagPes Ortho-Gynest- 2 56 Est 1 mg VagPes estriol Low Depot Eriksen 1992 1 79 Plac VagTab 2 75 Est 0.025 mg VagTab estradiol Vagifem Low Wiklund 1993 11 1 Plac Patch 1 11 Standar 2 Est 0.05 mg Patch estradiol 2 d Derman 1995 1 42 Plac Oral Standar 2 40 EP seq 2 mg E + 1 mg P Oral estradiol + norethindrone acetate Trisequens d Saletu 1995 1 32 Plac Patch Standar 2 32 Est 0.05 mg Patch estradiol Estraderm d Good 1996 1 91 Plac Patch Standar 2 88 Est 0.05 mg Patch estradiol Alora d 3 94 Est 0.10 mg Patch estradiol Alora High Speroff (Study 1) 1 54 Plac Patch 1996 UltraLo 2 54 Est 0.02 mg Patch estradiol FemPatch w E-66 Ar Est Study N RxCat Dose Route Generic Trade m Dose Chung 1996 1 40 Plac Oral Standar