L.A. CARE FORMULARY Healthy Families
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anthem Blue Cross Drug Formulary
Erythromycin/Sulfisoxazole (generic) INTRODUCTION Penicillins ...................................................................... Anthem Blue Cross uses a formulary Amoxicillin (generic) (preferred list of drugs) to help your doctor Amoxicillin/Clavulanate (generic/Augmentin make prescribing decisions. This list of drugs chew/XR) is updated quarterly, by a committee Ampicillin (generic) consisting of doctors and pharmacists, so that Dicloxacillin (generic) the list includes drugs that are safe and Penicillin (generic) effective in the treatment of diseases. If you Quinolones ..................................................................... have any questions about the accessibility of Ciprofloxacin/XR (generic) your medication, please call the phone number Levofloxacin (Levaquin) listed on the back of your Anthem Blue Cross Sulfonamides ................................................................ member identification card. Erythromycin/Sulfisoxazole (generic) In most cases, if your physician has Sulfamethoxazole/Trimethoprim (generic) determined that it is medically necessary for Sulfisoxazole (generic) you to receive a brand name drug or a drug Tetracyclines .................................................................. that is not on our list, your physician may Doxycycline hyclate (generic) indicate “Dispense as Written” or “Do Not Minocycline (generic) Substitute” on your prescription to ensure Tetracycline (generic) access to the medication through our network ANTIFUNGAL AGENTS (ORAL) _________________ of community -
2021 National Formulary 3Rd Quarter Edition
2021 National Formulary 3rd Quarter Edition Last Revised: 08/18/2021 Version 2021Q3c Table of Contents OVERVIEW 4 CARDIOVASCULAR (HEART) DRUGS 14 Alpha & Beta Blockers 14 COVERAGE LIMITATION 4 Antihypertensive Combinations 14 Calcium Channel Blockers (CCBs) 14 COMPOUNDED DRUGS 4 ACE Inhibitors without & with Diuretics 15 DRUG PLACEMENT DETERMINATION 4 ACE Inhibitors / CCB Combinations 15 ARBs without & with Diuretics 15 PREFERRED BRAND PRODUCTS 5 ARB Combinations 15 Naprilysin Inhibitors 15 GENERIC SUBSTITUTION 5 Diuretics 15 Renin Inhibtors 16 SINGLE & DUAL SOURCE GENERICS 5 Antiarrhythmics/Anti-Ischemic 16 Cardiac Glycosides 16 PRIOR AUTHORIZATIONS, STEP EDITS & QTY LIMITS 6 Vasodilators, Coronary, Nitrates/Vasodilators, Sympatholytics 16 EXCLUDED DRUGS 6 Other Drugs 16 NON-LISTED DRUGS & DRUG CATEGORIES 7 ANTIHYPERLIPIDEMIC (CHOLESTEROL) DRUGS 17 Statins & Statin/CCB Combinations 17 FORMULARY MODIFICATIONS & CHANGES 7 Bile Acid Sequestrants, Liver Drugs 17 Fibrates 17 BIOSIMILARS 7 ACL Inhibitors 17 Other Drugs 17 MAJOR CHANGES TO THE PDL 7 PANCREATIC DRUGS 18 ANTIBIOTICS 8 Penicillins & Cephalosporins 8 KIDNEY & URINARY / UROLOGICAL DRUGS 18 Tetracyclines 8 Benign Prostate Hyperplasia 18 Macrolides & Clindamycins 8 Urologic Drugs / Other Drugs 18 Sulfonamides, Sulfones & Ketolides 8 Erectile Dysfunction Drugs 18 Quinolones 8 Gout Drugs – Purine Inhibitors 19 Miscellaneous Antibiotics 8 Urinary Ph Modifiers 19 Potassium & Electrolytes 19 ANTI-VIRALS 9 Phosphorus/Calcium/Electrolyte Depleters 19 General Antivirals 9 HIV Antiviral Drugs 9 OSTEOPOROSIS (BONE) DRUGS 20 HIV Pre-Exposure Propylaxis Drugs 9 ANTI-INFLAMMATORY / ANALGESIC (PAIN) DRUGS 20 ANTI-INFECTIVES 10 Anti-Inflammatory Drugs (NSAIDS) 20 Anaerobic Anti-Infectives 10 COX-II Drugs 21 Antiparasitics 10 Analgesics, Narcotics (Opioids) 21 Antimalarials & Antiprotozoals 10 Analgesics, Salicylates, Non-Salicylates, Other 21 Antihelmintic Drugs 10 CENTRAL NERVOUS SYSTEM DRUGS 22 ANTIEMETICS 10 Anti-Anxiety Drugs (Benzodiazepines) 22 Sedative/Sleeping Drugs 22 NEUROLOGIC DRUGS 11 A.D.D. -
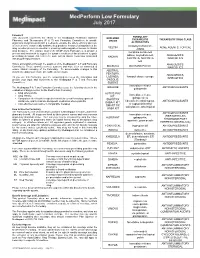
Medperform Low Formulary July 2017
MedPerform Low Formulary July 2017 Foreword FORMULARY This document represents the efforts of the MedImpact Healthcare Systems EXCLUDED THERAPEUTIC THERAPEUTIC DRUG CLASS Pharmacy and Therapeutics (P & T) and Formulary Committees to provide DRUGS physicians and pharmacists with a method to evaluate the safety, efficacy and cost- ALTERNATIVES effectiveness of commercially available drug products. A structured approach to the clindamycin/tretinoin, VELTIN ACNE AGENTS, TOPICAL drug selection process is essential in ensuring continuing patient access to rational ZIANA drug therapies. The ultimate goal of the MedPerform Formulary is to provide a morphine sulfate ER process and framework to support the dynamic evolution of this document to guide tablets, oxycodone ER, ANALGESICS, prescribing decisions that reflect the most current clinical consensus associated KADIAN with drug therapy decisions. NUCYNTA, NUCYNTA NARCOTICS ER This is accomplished through the auspices of the MedImpact P & T and Formulary ANALGESICS, BELBUCA BUTRANS PATCH Committees. These committees meet quarterly and more often as warranted to NARCOTICS ensure clinical relevancy of the Formulary. To accommodate changes to this ABSTRAL, document, updates are made accessible as necessary. FENTORA, ANALGESICS, LAZANDA, fentanyl citrate lozenge As you use this Formulary, you are encouraged to review the information and NARCOTICS provide your input and comments to the MedImpact P & T and Formulary ONSOLIS, Committees. SUBSYS immediate-release GRALISE ANTICONVULSANTS The MedImpact -

Printed Formulary Catalog Basic
Scripps Health Formulary July 2016 Foreword Pharmacy and Therapeutics Committee. MedImpact approves such multi- This document represents the efforts of the MedImpact Healthcare Systems source drugs for addition to the MAC list based on the following criteria: Pharmacy and Therapeutics (P & T) and Formulary Committees to provide physicians A multi-source drug product manufactured by at least one (1) nationally and pharmacists with a method to evaluate the safety, efficacy and cost-effectiveness marketed company. of commercially available drug products. A structured approach to the drug selection At least one (1) of the generic manufacturer’s products must have an “A” process is essential in ensuring continuing patient access to rational drug therapies. rating or the generic product has been determined to be unassociated with The ultimate goal of the Portfolio Formulary is to provide a process and framework to efficacy, safety or bioequivalency concerns by the MedImpact P & T support the dynamic evolution of this document to guide prescribing decisions that Committee. reflect the most current clinical consensus associated with drug therapy decisions. Drug product will be approved for generic substitution by the MedImpact P & T Committee. This is accomplished through the auspices of the MedImpact P & T and Formulary Committees. These committees meet quarterly and more often as warranted to ensure This list is reviewed and updated periodically based on the clinical literature and clinical relevancy of the Formulary. To accommodate changes to this document, pharmacokinetic characteristics of currently available versions of these drug updates are made accessible as necessary. products. As you use this Formulary, you are encouraged to review the information and provide If a member or physician requests a brand name product in lieu of an approved your input and comments to the MedImpact P & T and Formulary Committees. -

Estrogens, Estrogen Agonists/Antagonists, and Calcitonin Nelson B
48 Estrogens, Estrogen Agonists/Antagonists, and Calcitonin Nelson B. Watts Estrogen 408 Calcitonin 409 Estrogen Agonists/Antagonists (Selective Estrogen Receptor Summary 410 Modulators or Serms) 409 Selected Readings 410 Thus, it appears that estrogen has protective effects on ESTROGEN the skeleton only for as long as it is taken. However, women who take estrogen and then stop should be no It is well established that osteoporosis is more common worse off compared with women who have never taken in women than men and fracture risk increases dramati- estrogen at all. cally after menopause. The relationship between estro- Following results of the WHI, estrogen treatment is gen defi ciency and osteoporosis was fi rst suggested in the recommended for relief of menopausal symptoms, but in mid-1900s when Albright showed that treatment with the lowest dose and for the shortest time necessary. Most estrogen reversed the negative calcium balance in post- women are not suffi ciently symptomatic at menopause menopausal women. The positive effects of estrogen on to require estrogen therapy, and most who require estro- peak bone mass and on bone loss have been demon- gen will be able to stop after a few years. However, a strated in both men and women. For years, estrogen was minority will require estrogen long-term. For those considered the treatment of choice for postmenopausal women, estrogen may be suffi cient for prevention and/or women and widely advocated for prevention of bone loss, treatment of osteoporosis. with numerous trials showing prevention of bone loss Several different forms of estrogen are available for in recently menopausal women and increased of bone therapeutic use (e.g., estradiol, conjugated estrogen ester- mineral density (BMD) in women with postmenopausal ifi ed estrogens, etc.) as well as several routes of adminis- osteoporosis. -

AHFS Therapeutic
AHFS Therapeutic AHFS Therapeutic Class Description HICL HICL Description Program Edit Criteria 1 Edit Criteria 2 Edit Criteria 3 Edit Criteria 4 Edit Criteria 5 Class 240408 CARDIOTONIC AGENTS 000004 DIGOXIN PACE MAX DAILY UNITS : 0.667000 240408 CARDIOTONIC AGENTS 000004 DIGOXIN PACE MAX DAILY UNITS : 0.750000 240408 CARDIOTONIC AGENTS 000004 DIGOXIN PACE MAX DAILY UNITS : 1.500000 240408 CARDIOTONIC AGENTS 000004 DIGOXIN PACE MAX DAILY UNITS : 2.000000 240408 CARDIOTONIC AGENTS 000004 DIGOXIN PACE MAX DAILY UNITS : 2.500000 240408 CARDIOTONIC AGENTS 000004 DIGOXIN PACE MAX DAILY UNITS : 3.000000 240408 CARDIOTONIC AGENTS 000004 DIGOXIN PACE MAX DAILY UNITS : 3.750000 240408 CARDIOTONIC AGENTS 000004 DIGOXIN PACE MAX DAILY UNITS : 6.000000 240408 CARDIOTONIC AGENTS 000004 DIGOXIN PACE MAX DAILY UNITS : 7.500000 240408 CARDIOTONIC AGENTS 000004 DIGOXIN PACE Medical Exception Required 282032 RESPIRATORY AND CNS STIMULANTS 000007 CAFFEINE/DEXTROSE PACE Cannnot co‐administer inhaled Insulin and Asthma/COPD/Smoking Cessation agents 282032 RESPIRATORY AND CNS STIMULANTS 000008 CAFFEINE/MULTIVITAMIN PACE Cannnot co‐administer inhaled Insulin and Asthma/COPD/Smoking Cessation agents 282032 RESPIRATORY AND CNS STIMULANTS 000009 CAFFEINE/ETHYL ALCOHOL PACE Cannnot co‐administer inhaled Insulin and Asthma/COPD/Smoking Cessation agents 282032 RESPIRATORY AND CNS STIMULANTS 000010 CAFFEINE/SODIUM BENZOATE PACE Cannnot co‐administer inhaled Insulin and Asthma/COPD/Smoking Cessation agents 282032 RESPIRATORY AND CNS STIMULANTS 000011 CAFFEINE CITRATE -

REVIEW Estrogens and Atherosclerosis
R13 REVIEW Estrogens and atherosclerosis: insights from animal models and cell systems Jerzy-Roch Nofer1,2 1Center for Laboratory Medicine, University Hospital Mu¨nster, Albert Schweizer Campus 1, Geba¨ude A1, 48129 Mu¨nster, Germany 2Department of Medicine, Endocrinology, Metabolism and Geriatrics, University of Modena and Reggio Emilia, Modena, Italy (Correspondence should be addressed to J-R Nofer at Center for Laboratory Medicine, University Hospital Mu¨nster; Email: [email protected]) Abstract Estrogens not only play a pivotal role in sexual development but are also involved in several physiological processes in various tissues including vasculature. While several epidemiological studies documented an inverse relationship between plasma estrogen levels and the incidence of cardiovascular disease and related it to the inhibition of atherosclerosis, an interventional trial showed an increase in cardiovascular events among postmenopausal women on estrogen treatment. The development of atherosclerotic lesions involves complex interplay between various pro- or anti-atherogenic processes that can be effectively studied only in vivo in appropriate animal models. With the advent of genetic engineering, transgenic mouse models of atherosclerosis have supplemented classical dietary cholesterol- induced disease models such as the cholesterol-fed rabbit. In the last two decades, these models were widely applied along with in vitro cell systems to specifically investigate the influence of estrogens on the development of early and advanced atherosclerotic lesions. The present review summarizes the results of these studies and assesses their contribution toward better understanding of molecular mechanisms underlying anti- and/or pro-atherogenic effects of estrogens in humans. Journal of Molecular Endocrinology (2012) 48, R13–R29 Introduction circumstances, these hormones promote the develop- ment of atherosclerosis. -
Custom-Drug-List-Formulary.Pdf
!"#$%ÿ'(!)ÿ12"# ÿ ÿ ÿ ÿ 3435 Blue Cross and BCN Custom Drug List - September 2021 Table of contents Blue Cross and BCN Custom Drug List (Formulary) 6 Specific information for Blue Cross Members 14 Blue Cross/BCN Preferred Alternatives List Appendix A Anti-infectives 1A Antifungals 16 1B Antimalarials 16 1C Antiparasitics and antihelmintics 16 1D Antiretrovirals 17 1E Antituberculars 18 1F Antivirals 18 1G Cephalosporins 19 1H Macrolides 19 1I Penicillins 19 1J Quinolones 19 1K Sulfonamides and combinations 19 1L Tetracyclines 20 1M Urinary tract agents 20 1N Miscellaneous anti-infectives 20 Cardiovascular, hypertension, cholesterol 2A ACE-Inhibitors and combinations 21 2B Alpha-adrenergic agents 21 2C Angiotensin II Receptor Blockers and combinations 22 2D Anticoagulants and hemostasis agents 22 2E Beta blockers and combinations 23 2F Calcium channel blockers and combinations 23 2G Cardiovascular treatment 24 2H Diuretics 24 2I Lipid-lowering agents 25 2J Nitrates and combinations 26 2K Renin-inhibitors and combinations 26 2L Miscellaneous antihypertensives 26 Page 1 Central nervous system 3A Alzheimer's therapy 27 3B Anticonvulsants 28 3C Antidepressants 29 3D Antipsychotics 30 3E Anxiolytics 31 3F CNS stimulants 31 3G Migraine therapy 32 3H Myasthenia gravis 32 3I Narcotic antagonists and withdrawal management 32 3J Narcotic mixed agonist and antagonist 33 3K Narcotic and analgesic combinations 33 3L Narcotics 34 3M Nonsteroidal anti-inflammatory drugs 35 3N Parkinsons disease and related disorders 36 3O Salicylates 36 -

Mclane Group Employees Formulary 1St Quarter 2018
McLane Group Employees Formulary 1st Quarter 2018 LAST REVISED 12/20/2017 P a g e | 2 Table of Contents What is my prescription drug coverage? ........................................................................ 3 What is the Scott & White Health Plan formulary? ........................................................ 3 How was the formulary created and how are new medications reviewed? ................... 3 Does the formulary ever change? ................................................................................... 4 How am I notified of changes to the formulary? ............................................................ 4 What are brand-name and generic drugs? ..................................................................... 4 What is generic substitution? ......................................................................................... 5 What are Specialty drugs? .............................................................................................. 5 What are pharmaceutical management procedures? .................................................... 5 Are there any restrictions on my coverage? ................................................................... 5 How do I request an exception to the SWHP formulary? ............................................... 5 What drugs are not covered by my prescription drug benefit? ...................................... 6 How much medication does my copayment cover and does my plan cover maintenance medications? ............................................................................................ -

<Document Name>
Indiana Health Coverage Programs PROVIDER BULLETIN BT200409 MAY 3, 2004 To: All Pharmacy Providers and Prescribing Practitioners Subject: New Policy – Mandatory 90-Day Supply for Selected Maintenance Medications Note: The information referenced below is not directed to those providers rendering services in the risk-based managed care (RBMC) delivery system. Overview and Background In Indiana Health Coverage Program (IHCP) provider bulletin BT200406 dated March 26, 2004, the Office of Medicaid Policy and Planning (OMPP) announced a new policy requiring pharmacy providers to dispense at least a 90 day supply of selected maintenance medications (see Table 1). That policy change was announced to be effective on May 11, 2004. The purpose of this bulletin is to announce a change in the implementation date of the new policy, which is now May 25, 2004. This bulletin also contains changes to the policy’s parameters,and, as such, will serve to clarify and outline the new policy. Affected Recipients All fee-for-service Medicaid recipients will be affected by this policy, with the exception of those individuals residing in nursing facilities and intermediate care facilities for the mentally retarded (ICFs/MR); the new policy does not apply to those recipients. The identification of a Medicaid recipient as belonging to one of these excluded categories will be by way of the recipient’s eligibility information on file with ACS, the State’s Pharmacy Benefits Manager. Details The provider will be prompted to dispense a 90-day supply of a selected maintenance medication if 30 days or greater of therapy with one of the selected maintenance medications within the last 180 days is found in the patient’s medication claims history. -

WO 2013/074910 Al 23 May 2013 (23.05.2013) W P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2013/074910 Al 23 May 2013 (23.05.2013) W P O P C T (51) International Patent Classification: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, A61K 38/26 (2006.01) A61K 31/56 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, A61K 38/00 (2006.01) DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (21) International Application Number: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, PCT/US20 12/065492 ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (22) International Filing Date: NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, 16 November 2012 (16.1 1.2012) RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, (25) Filing Language: English ZM, ZW. (26) Publication Language: English (84) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of regional protection available): ARIPO (BW, GH, 61/561,094 17 November 201 1 (17. 11.201 1) US GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (71) Applicant: INDIANA UNIVERSITY RESEARCH AND TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, TECHNOLOGY CORPORATION [US/US]; 35 1 West EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, LV, 10th Street, Indianapolis, Indiana 46202 (US). -

Customer Drug List Formulary
2017 ® Confidence comes with every card. Custom Drug List Blue Cross and BCN Custom Drug List - August 2017 Table of contents Blue Cross and BCN Custom Drug List (Formulary) 6 Specific information for Blue Cross Members 8 Specific information for Blue Care Network Members 13 How to read the Blue Cross/BCN Custom Drug List 16 Blue Cross/BCN Preferred Alternatives List Appendix A Anti-infectives 1A Antifungals 17 1B Antimalarials 17 1C Antiparasitics and anthelmintics 17 1D Antiretrovirals 18 1E Antituberculars 19 1F Antivirals 19 1G Cephalosporins 20 1H Macrolides 20 1I Penicillins 20 1J Quinolones 20 1K Sulfonamides and combinations 21 1L Tetracyclines 21 1M Urinary tract agents 21 1N Miscellaneous anti-infectives 22 Cardiovascular, hypertension, cholesterol 2A ACE-Inhibitors and combinations 23 2B Alpha-adrenergic agents 23 2C Angiotensin II Receptor Blockers and combinations 24 2D Anticoagulants and hemostasis agents 25 2E Beta blockers and combinations 26 2F Calcium channel blockers and combinations 27 2G Cardiovascular treatment 27 2H Diuretics 28 2I Lipid-lowering agents 29 2J Nitrates and combinations 29 2K Renin-inhibitors and combinations 30 2L Miscellaneous antihypertensives 30 Page 1 Central nervous system 3A Alzheimer's therapy 31 3B Anticonvulsants 32 3C Antidepressants 33 3D Antipsychotics 34 3E Anxiolytics 34 3F CNS stimulants 35 3G Migraine therapy 36 3H Myesthenia gravis 36 3I Narcotic antagonists 36 3J Narcotic mixed agonist and antagonist 37 3K Narcotic and analgesic combinations 37 3L Narcotics 38 3M Nonsteroidal anti-inflammatory