Appendix I: IPS Glossary of Terms and Definitions Absolute (Visual Field
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Radiometric and Photometric Concepts Based on Measurement Techniques C
Application Note No. 6 April 1982 Radiometric and Photometric Concepts Based on Measurement Techniques C. Richard Duda Senior Scientist, United Detector Technology 3939 Lanmark Street, Culver City, Cal. 90230 Abstract The value of the fundamental quality in radiometry, the bution of optical radiation. In 1937 the National Bureau watt, is presently realized by electrical substitution in of Standards transferred the luminous intensity produced which the temperature produced in a blackened mate- by a platinium blackbody to a series of lamps. This orig- rial due to absorption of radiant energy is balanced inal calibration has served to this date for standardiza- against that produced by electrical energy whose cur- tion of lamps used by industry to realize the photometric rent and voltage can accurately be measured. A new scale. Recently the fundamental unit in photometry was method to measure optical radiation is being explored changed from the candela, as defined by a blackbody, to by the National Bureau of Standards in which photons the lumen, as defined by the watt, uniting the conceptual are absorbed in a semiconductor and converted with ef- interrelationships between photometry and radiometry. 1 ficiency closely approaching the theoretical maximum Changes in the photometric scale due to redefinition of - 100 percent. its less than one percent difference in NBS lamp inten- sity values. 2 Other radiometric concepts, such as radiance, irradi- ance, and radiant intensity can easily be defined through Because Vλ , the mathematical representations of human simple geometric relationships. Photometry on the other visual spectral response is difficult to realize with a high hand, while sharing these identical relationships also in- degree of accuracy in a practical detector, comparison troduces detector response modeled after human visual of sources with a broad spectral distribution can best be traits; new measurement unit names, and reliance on accomplished with a reference source. -

Foot-Candles: Photometric Units
UPDATED EXTRACT FROM CREG JOURNAL. FILE: FOOT3-UP.DOC REV. 8. LAST SAVED: 01/02/01 15:14 PHOTOMETRICS Foot-Candles: Photometric Units More footnotes on optical topics. David Gibson describes the confusing range of photometric units. A discussion of photometric units may the ratio of luminous efficiency to luminous The non-SI unit mean spherical candle- seem out of place in an electronic journal but efficiency at the wavelength where the eye is power is the intensity of a source if its light engineers frequently have to use light sources most sensitive. Unfortunately, however, this output were spread evenly in all directions. It and detectors. The units of photometry are term can be confused with the term efficacy, is therefore equivalent to the flux [lm] ¸ 4p. some of the most confusing and least which is used to describe the efficiency at standardised of units. converting electrical to luminous power. Luminance Photometric units are not difficult to The candela measures the intensity of a understand, but can be a minefield to the Illumination, Luminous Emittance. point source. We also need to define the uninitiated since many non-SI units are still The illumination of a surface is the properties of an extended source. Each small in use, and there are subtle differences incident power flux density measured in element DS of a diffuse reflective surface will between quantities with similar names, such lumens per square metre. A formal definition scatter the incident flux DF and behave as if as illumination and luminance. would be along the lines of: if a flux DF is it were an infinitesimal point source. -

Notes: D=Distance in Meters A=Pupil Area in Mm2 = 3.14159 Eq
2. Physical and Physiological Optics I. Radiometry Energy (erg = dyne cm; joule = 107 erg) Power P (erg/sec, watt = joule/sec, horsepower, calorie) Radiant flux, also P (watts, passing through an area of a surface coming from one side of the surface) dP Irradiance E = radiant flux/area (watt/cm2) = where S is area e dS Primary/Secondary sources Solid angle ω (steradians) vs angle θ (radians) Point sources dP Radiant intensity I = (watts/steradian emitted in a particular direction) e dω 2 Therefore, irradiance Ee = Iecosθ/r on a surface situated along that direction Extended sources (the sky, a piece of paper, a monitor screen) dP 2 Radiant emittance Me = = watt/cm emitted in all directions A B dS S Next, consider the case when the source is a surface. ∆ Plane A is close to the source, and has a small hole ∆σ of size ∆σ small enough to be treated as a point source. The observer is at plane B a large distance r O x away. Thus, as seen from B, the hole subtends solid θ angle ∆ω=∆σ/r 2. The observers sees a patch of area ∆S of the surface through the hole. r 2 Radiance Le = watt/cm /steradian emitted by a patch in a particular direction = dIe /dσ = radiant intensity per area of hole = dEe /dω = received irradiance per solid angle of source (i.e., per steradian) 2 2 (because ∆Ee=∆Ie /r and ∆ω=∆σ/r ) Lambertian (source/surface), cosine law, here’s the derivation: ∆σ = ∆S cosθ ∆P = ∫Le∆σdω ω Me∆S = ∫Le∆σdω ω Me = ∫Lecosθdω ω Change integration to annuli around the normal, and for Lambertian surface, Le is independent of θ: dω = 2πsinθdθ π 2 Hence: Me = πLe ∫ sin2θdθ = πLe 0 Light as a wave speed of light c ∼ 3 × 1010 cm/sec wavelength λ = c /ν (in nm = 10−9 meters) (visible = blue 400 to red 700) Light as particles Photons, each of energy hν (h = 6.6245 × 10−27 erg sec; ν = cycles/sec) Expected number of quanta = energy/energy-per-photon Spectral content Spectral power distribution (e.g. -

Sept.-Oct., !962
I Milliard I MULLARD-AUSTRALIA PTY. LTD. (Mullardl VOL 5 — No. 5 SEPT.-OCT., !962 Editorial Office: 35-43 Clarence Street, Sydney. Telephone: 29 2006 “Oh, wad some Pow’r the giftie gie us, Editor: To see oursels as ithers see us.” JOERN BORK Robert Burns. All rights reserved by Mullard-Australia Pty. Ltd., Sydney. Information given in this pub lication does not imply a licence under any patent. Original articles or illustrations re produced in whole or in part must be The Insignia and the Image accompanied by full acknowledgement: Muliard Outlook, Australian Edition. Both noticed by the other fellow and always linked— the TABLE OF CONTENTS image more elusive with pulse and personality, for it can surge Editorial ........................ - .................................... 50 with the progress of the company, by its products and its Viewpoint w ith Muliard ............................... 51 The Range of Muliard Transmitting personnel, its aggressiveness and its humility, by its Service— or Valves for SSB ........................................... 52 Thermistors ............................................................ 53 wither for the lack of it! Repairing Ferroxcube Aerial Inductor Rods ........................................................................ 55 Use of Quarter-Track Heads with An insignia, perhaps a few minutes work by an artist, an Muliard Tape C irc u its .................................. 55 image evolved through the years from the painstaking efforts Muliard Semiconductors with CV Approval ........................................................... -

1. 2 Photometric Units
4 CHAPTERl INTRODUCTION 1. 2 Photometric units Before starting to describe photomultiplier tubes and their characteristics,this section briefly discusses photometric units commonly used to measurethe quantity of light. This section also explains the wavelength regions of light (spectralrange) and the units to denotethem, as well as the unit systemsused to expresslight intensity. Since information included here is just an overview of major photometric units, please refer to specialty books for more details. 1. 2. 1 Spectral regions and units Electromagneticwaves cover a very wide rangefrom gammarays up to millimeter waves.So-called "light" is a very narrow range of theseelectromagnetic waves. Table 1-1 showsdesignated spectral regions when light is classified by wavelength,along with the conver- sion diagram for light units. In general, what we usually refer to as light covers a range from 102to 106 nanometers(nm) in wavelength. The spectral region between 350 and 70Onmshown in the table is usually known as the visible region. The region with wavelengthsshorter than the visible region is divided into near UV (shorter than 35Onrn),vacuum UV (shorter than 200nm) where air is absorbed,and extremeUV (shorter than 100nm). Even shorter wavelengthsspan into the region called soft X-rays (shorter than IOnrn) and X- rays. In contrast, longer wavelengths beyond the visible region extend from near IR (750nm or up) to the infrared (severalmicrometers or up) and far IR (severaltens of micrometers) regions. Wavelength Spectral Range Frequency Energy nm (Hz) (eV) X-ray Soft X-ray 10 102 1016 ExtremeUV region 102 10 Vacuum UV region 200 Ultravioletregion 10'5 350 Visible region 750 103 Near infraredregion 1 1014 104 Infrared region 10-1 1013 105 10-2 Far infrared region 1012 106 10-3 . -
Functional Diagnostics 1 P8.1 Differential Light Sensitivity 1 P8.2 Luminance 1 Functional Diagnostics 1
Contents P8 Functional Diagnostics 1 P8.1 Differential light sensitivity 1 P8.2 Luminance 1 Functional Diagnostics 1 P8.1 Differential light sensitivity In the ZEISS Humphrey® Field Analyzer HFA II-i, the maximum luminance ® of the light stimulus is Lmax = 10; 000 asb. For the Haag–Streit Octopus , 2 we have Lmax = 1; 000 asb. In both devices a luminance Lb = 10 cd=m is used for background illumination. With the HFA II-i, the examiner measures a DLS value of 30 dB. What would be the corresponding DLS value of the Octopus® perimeter? Solution: Using Eq. (8.2), we find for the threshold differential luminance ∆Lth −2 ∆Lmax (in cd m ) DLS (in dB) = 10 log −2 (S8.1) ∆Lth (in cd m ) with ∆Lmax = Lmax. From Eq. (S8.1), we obtain −DLS=10 ∆Lth = ∆Lmax · 10 : Inserting the given values, we get 4 −30=10 ∆Lth = 10 asb · 10 = 10 asb : For the Octopus device, we calculate the DLS value for ∆Lth = 10 asb again using Eq. (S8.1). It follows that 1000 asb DLS (in dB) = 10 log = 20 dB : 10 asb P8.2 Luminance Consider a hot tungsten platelet with a luminating area of 1 mm2. The platelet has a temperature of 3500 K. Under the assumption that the platelet can be considered a black body, what is its luminance? Compare this re- sult with the maximum luminance of Lmax = 10; 000 asb for the ZEISS Humphrey® Field Analyzer HFA II-i. Solution: According to the Stefan–Boltzmann law about the radiant emittance (intensity) emit- ted by a black body, we know that 4 I(T) = σb T (S8.2) 2 Solutions to Problems – Optical Devices in Ophthalmology and Optometry 100 14 90 13 12 80 -1 11 70 10 60 9 8 50 7 40 6 5 30 4 luminous eciency (%) luminous ecacy (lm W ) luminous ecacy (lm 20 3 2 10 1 0 2000 4000 6000 8000 10000 12000 14000 16000 temperature (K) Figure S8.1 Luminous efficacy versus temperature for a black body radiator. -
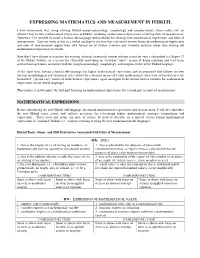
Here Is How Ithkuil Handles Mathematical Expressions and Units
EXPRESSING MATHEMATICS AND MEASUREMENT IN ITHKUIL I have determined that, using existing Ithkuil morpho-phonology, morphology and morpho-syntax, there really isn’t an efficient way to state mathematical expressions in Ithkuil, including mathematical expressions involving units of measurement. Therefore, I’ve decided to create a formal sub-language within Ithkuil for dealing with mathematical expressions and units of measurement. You can think of this as a verbal analogy to the way that real-world written forms of mathematical expressions and rates of measurement require their own formal set of written symbols and symbolic notation rather than writing out mathematical expressions in words. Note that I have chosen to maintain the existing informal centesimal system without a root for zero as described in Chapter 12 of the Ithkuil website, as a means for efficiently conveying an everyday “naïve” means of doing counting and very basic arithmetical operations consistent with the morpho-phonology, morphology, and morpho-syntax of the Ithkuil language. At the same time, having a formal sub-language for higher mathematical expressions and measurement that follows its own internal morphological and syntactical rules allows for a succinct means of verbal mathematical expression and underscores the formalized, “special case” nature of mathematical expressions, again analagous to the formal written notation for mathematical expressions in real-world languages. This treatise is in two parts; the first part focusing on mathematical expressions, the second part on units of mearurement. MATHEMATICAL EXPRESSIONS Before introducing the new Ithkuil sub-language for formal mathematical expressions and measurement, I will first introduce the new Ithkuil roots, stems, and suffixes necessary for referencing higher mathematical concepts, terminology and expressions. -
![SUPPLEMENT to ITHKUIL LEXICON [Latest Roots Added March 27, 2015, Shown in Blue]](https://docslib.b-cdn.net/cover/6907/supplement-to-ithkuil-lexicon-latest-roots-added-march-27-2015-shown-in-blue-6666907.webp)
SUPPLEMENT to ITHKUIL LEXICON [Latest Roots Added March 27, 2015, Shown in Blue]
SUPPLEMENT TO ITHKUIL LEXICON [latest roots added March 27, 2015, shown in blue] -BBR- FALSE (or SUPERSEDED) FUNDAMENTAL CONCEPTS OF SCIENCE INFORMAL Stems FORMAL Stems 1. false/superseded fundamental concept from physics 1. false/superseded fundamental concept from astronomy and cosmology 2. false/superseded fundamental concept from 2. false/superseded fundamental concept from geology chemistry 3. false/superseded fundamental concept from biology 3. false/superseded fundamental concept from medicine and psychology COMPLEMENTARY Stems COMPLEMENTARY Stems same as above 3 stems same as above 3 stems same as above 3 stems with same as above 3 stems with with focus on the with focus on the focus on the concept/entity focus on the concept/entity itself consequences/effect/impact itself consequences/effect/impact SSD Derivatives for Informal Stem 1: 5) phlogiston 7) caloric SSD Derivatives for Formal Stem 1: 1) lumiferous aether -BŽ - ECCENTRICITY/WEIRDNESS/UNORTHODOXY INFORMAL FORMAL 1. state of being eccentric/non-conforming to expected FORMAL stems are the same as INFORMAL stems societal norms except that for FORMAL stems, the party whom the stem 2. state of being weird/outlandish describes is seemingly or apparently (self-) aware of their 3. state of being unorthodox / “out of the box” / not per state, whereas when using INFORMAL stems, the party normative standards or guidelines is seemingly or apparently unaware or ignorant of their COMPLEMENTARY STEMS own state. Same as above 3 stems Same as above 3 stems with focus on the state or with focus on the feeling itself consequences of being in such a state -CC- DEGREE OF CAPACITY FOR EMOTION INFORMAL Stems FORMAL Stems 1. -

The Complete List of Measurement Units Supported
28.3.2019 The Complete List of Units to Convert The List of Units You Can Convert Pick one and click it to convert Weights and Measures Conversion The Complete List of Measurement Units Supported # A B C D E F G H I J K L M N O P Q R S T U V W X Y Z # ' (minute) '' (second) Common Units, Circular measure Common Units, Circular measure % (slope percent) % (percent) Slope (grade) units, Circular measure Percentages and Parts, Franctions and Percent ‰ (slope permille) ‰ (permille) Slope (grade) units, Circular measure Percentages and Parts, Franctions and Percent ℈ (scruple) ℔, ″ (pound) Apothecaries, Mass and weight Apothecaries, Mass and weight ℥ (ounce) 1 (unit, point) Apothecaries, Mass and weight Quantity Units, Franctions and Percent 1/10 (one tenth or .1) 1/16 (one sixteenth or .0625) Fractions, Franctions and Percent Fractions, Franctions and Percent 1/2 (half or .5) 1/3 (one third or .(3)) Fractions, Franctions and Percent Fractions, Franctions and Percent 1/32 (one thirty-second or .03125) 1/4 (quart, one forth or .25) Fractions, Franctions and Percent Fractions, Franctions and Percent 1/5 (tithe, one fifth or .2) 1/6 (one sixth or .1(6)) Fractions, Franctions and Percent Fractions, Franctions and Percent 1/7 (one seventh or .142857) 1/8 (one eights or .125) Fractions, Franctions and Percent Fractions, Franctions and Percent 1/9 (one ninth or .(1)) ångström Fractions, Franctions and Percent Metric, Distance and Length °C (degrees Celsius) °C (degrees Celsius) Temperature increment conversion, Temperature increment Temperature scale -
PHOTOMULTIPLIER TUBES Basics and Applications FOURTH EDITION Introduction
PHOTOMULTIPLIER TUBES Basics and Applications FOURTH EDITION Introduction Light detection technolgy is a powerful tool that provides deeper understanding of more sophisticated phe- nomena. Measurement using light offers unique advantages: for example, nondestructive analysis of a sub- stance, high-speed properties and extremely high detectability. Recently, in particular, such advanced fields as scientific measurement, medical diagnosis and treatment, high energy physics, spectroscopy and biotech- nology require development of photodetectors that exhibit the ultimate in various performance parameters. Photodetectors or light sensors can be broadly divided by their operating principle into three major categories: external photoelectric effect, internal photoelectric effect and thermal types. The external photoelectric effect is a phenomenon in which when light strikes a metal or semiconductor placed in a vacuum, electrons are emitted from its surface into the vacuum. Photomultiplier tubes (often abbreviated as PMT) make use of this external photoelectric effect and are superior in response speed and sensitivity (low- light-level detection). They are widely used in medical equipment, analytical instruments and industrial measurement systems. Light sensors utilizing the internal photoelectric effect are further divided into photoconductive types and photovoltaic types. Photoconductive cells represent the former, and PIN photodiodes the latter. Both types feature high sensitivity and miniature size, making them well suited for use as sensors in camera exposure meters, optical disk pickups and in optical communications. The thermal types, though their sensitivity is low, have no wavelength-dependence and are therefore used as temperature sensors in fire alarms, intrusion alarms, etc. This handbook has been structured as a technical handbook for photomultiplier tubes in order to provide the reader with comprehensive information on photomultiplier tubes. -

Light-Emitting Diodes
445.664 Light-Emitting Diodes Chapter 16. Human eye sensitivity and photometric quantities Euijoon Yoon 445.664 (Intro. LED) / Euijoon Yoon Human vision Ganglion cell (circadian receptor) • Cones: provide color sensitivity • Rods : color insensitive • Color perception depends on light intensity. • Photopic vision regime: High light level vision regime (during daylight) • Scotopic vision regime: Low light level vision regime (at night) 445.664 (Intro. LED) / Euijoon Yoon 1 Three different vision regime • Photopic vision : human vision at high ambient light level (daylight condition) • Scotopic vision : human vision at low ambient light level (at night) • Mesopic vision : light level between the photopic and scotopic vision regime 445.664 (Intro. LED) / Euijoon Yoon Normalized spectral sensitivity • Night-time vision is weaker in the red spectral range • Stronger in the blue spectral range as compared to day-time vision 445.664 (Intro. LED) / Euijoon Yoon 2 History of photometric units • Photograph shows plumber’s candle. • A plumber’s candle emits a luminous intensity of 1 candela (cd). The cd is historical origin of all photometric units. • photometric unit is relevant when it comes to light perception by a human being. • First definition (now obsolete) : The luminous intensity of a standardized candle is 1 cd. • Second definition (now obsolete) : 1 cm2 of platinum (Pt) at 1042K (temperature of solidification) has a luminous intensity of 20.17 cd. • Third definition (current) : A monochromatic light source emitting an optical power of (1/683)Watt at 555 nm into the solid angle of 1 steradian (sr) has a luminous intensity of 1 cd. • Candlepower and candle are obsolete units. -

Of Light, of Falling O N I Square Foot
surface measured in candelas per square tion of that surface, termed illu Jore technical information, metre. minance. The illuminance caused by I belp and advice. That was The light that a source emits is lumen uniform ly on 1 square metre is tbe clear message sent back termed its luminous flux and is defined as I Lux in the SI system *, alter by our readers in response measured in Lumens. A lumen is defin natively 1 Foot-candles for I lumen to our survey. But how to ed such that a point source of light, of falling o n I square foot. accomplish this when the on e candela intensity, radiating If we refer to the luminaire sectio ns knowledge and experience uniformly in all directions emits 4n of The Strandbook we find figures of il of our readers ranges from lumens. Section 6 of The Strandbook luminance quoted at selected distances s tudent to experienced reveals a staggering range of lamp fro m the luminaire. We w ill also note lumen 'packages' from a modest 5000 that illuminance reduces in proportion professional designers, lumens, for a 300W M38, to a massive to the square of the distance from the engineers and technicians? 1,100,000 lumens, for a 12kW HMI! source to the surface; generally referred And where interests vary This figure, for an individual lamp is the to as the inverse sq uare law. from Theatre to Television, rota! output measured by integrating or For fixed lighting installatio ns recom J-fotion Picture and summing the luminous flux output over mended illuminances for a wide varie Architectural Lighting.