Diving and Hyperbaric Medicine
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

VR Series Dive Computer Manual
VR Technology Limited To ensure your user information is up to date. Please check www.technologyindepth.com for updates to this manual. VR Series Dive Computer Manual VR Dive Computer Operations Manual 2009 rev E 28/01/2009 1 VR Technology Limited Model Name VRX/VR3 Manufactured by VR Technology Limited Unit 12 Blackhill Road West Holton Heath Industrial Estate Poole Dorset BH16 6LE England UK WARNING Diving is an adventurous sport and should not be undertaken without receiving the necessary training from a recognised training agency. VR Dive Computer Operations Manual 2009 rev E 28/01/2009 2 VR Technology Limited Table of Contents Model Name...................................................................................................................2 Manufactured by ............................................................................................................2 Getting Started ...............................................................................................................7 Battery............................................................................................................................7 Power Monkey charging option (VRx)..........................................................................8 Switches .....................................................................................................................8 Home Screen..................................................................................................................9 The Home Screen features.........................................................................................9 -

Supplementary Report to the Final Report of the Coral Reef Expert Group: S6
The Great Barrier Reef Marine Park Authority acknowledges the continuing sea country management and custodianship of the Great Barrier Reef by Aboriginal and Torres Strait Islander Traditional Owners whose rich cultures, heritage values, enduring connections and shared efforts protect the Reef for future generations. © Commonwealth of Australia (Australian Institute of Marine Science) 2020 Published by the Great Barrier Reef Marine Park Authority ISBN 9780648721406 This document is licensed for use under a Creative Commons Attribution-NonCommercial 4.0 International licence with the exception of the Coat of Arms of the Commonwealth of Australia, the logos of the Great Barrier Reef Marine Park Authority and the Queensland Government, any other material protected by a trademark, content supplied by third parties and any photographs. For licence conditions see: https://creativecommons.org/licenses/by-nc/4.0/ A catalogue record for this publication is available from the National Library of Australia This publication should be cited as: Gonzalez-Rivero, M., Roelfsema, C., Lopez-Marcano, S., Castro-Sanguino,C., Bridge, T., and Babcock, R. 2020, Supplementary Report to the Final Report of the Coral Reef Expert Group: S6. Novel technologies in coral reef monitoring, Great Barrier Reef Marine Park Authority, Townsville. Front cover image: Underwater reefscape view of Lodestone Reef, Townsville region © Commonwealth of Australia (GBRMPA), photographer: Joanna Hurford. DISCLAIMER While reasonable effort has been made to ensure that the contents of this publication are factually correct, the Commonwealth of Australia, represented by the Great Barrier Reef Marine Park Authority, does not accept responsibility for the accuracy or completeness of the contents, and shall not be liable for any loss or damage that may be occasioned directly or indirectly through the use of, or reliance on, the contents of this publication. -

Therapeutic Hypothermia: Where Do We Stand?
5/29/2015 Therapeutic Hypothermia: Where Do We Stand? Melina Aguinaga-Meza, MD Assistant Professor of Medicine Gill Heart Institute University of Kentucky Disclosure Information Melina Aguinaga-Meza, MD “Therapeutic Hypothermia: Where Do We Stand?” • FINANCIAL DISCLOSURE: – No relevant financial relationship exists • UNLABELED/UNAPPROVED USES DISCLOSURE: – No relevant relationship exists 1 5/29/2015 The Clinical Problem • Out-of-hospital cardiac arrest (OHCA) is a leading cause of death among adults in the US • Approx. 300,000 OHCA events occur each year in the US • Resuscitation is attempted in 100,000 of these arrests • Less than 40 000 survive to hospital admission MMWR / July 29, 2011 / Vol. 60 / No. 8 2 5/29/2015 Consequences From Cardiac Arrest Myocardial Brain injury dysfunction Post-Cardiac Arrest Syndrome Systemic ischemia Disorder that + reperfusion caused the cardiac responses arrest • The effects of this syndrome are severe and pervasive MMWR / July 29, 2011 / Vol. 60 / No. 8 Survival and Neurological Outcomes after OHCA • Only one third of patients admitted to the hospital survive to hospital discharge • Approx. one out of ten people who experience OHCA survive to hospital discharge • Only 2 out of 3 of them have a good/moderate neurologic recovery MMWR / July 29, 2011 / Vol. 60 / No. 8: CARES 3 5/29/2015 “Chain of Survival” • Actions needed to improve chances of survival from out-of-hospital cardiac arrest Circulation 2010; 122:S676-84 • Try to identify and treat the precipitating causes of the arrest and prevent recurrent -
2008 June;38(2)
9^k^c\VcY=neZgWVg^XBZY^X^cZKdajbZ(-Cd#'?jcZ'%%- EJGEDH:HD;I=:HD8>:I>:H IdegdbdiZVcY[VX^a^iViZi]ZhijYnd[VaaVheZXihd[jcYZglViZgVcY]neZgWVg^XbZY^X^cZ Idegdk^YZ^c[dgbVi^dcdcjcYZglViZgVcY]neZgWVg^XbZY^X^cZ IdejWa^h]V_djgcVaVcYidXdckZcZbZbWZghd[ZVX]HdX^ZinVccjVaanViVhX^Zci^ÄXXdc[ZgZcXZ HDJI=E68>;>8JC9:GL6I:G :JGDE:6CJC9:GL6I:G6C9 B:9>8>C:HD8>:IN 76GDB:9>86AHD8>:IN D;;>8:=DA9:GH D;;>8:=DA9:GH EgZh^YZci EgZh^YZci 9gB^`Z7ZccZii 1B#7ZccZii5jchl#ZYj#Vj3 Egd[#6a[7gjWV`` 1Va[#d#WgjWV``5cicj#cd3 EVhiçEgZh^YZci K^XZEgZh^YZci 9g8]g^h6Xdii 1XVXdii5deijhcZi#Xdb#Vj3 9gEZiZg<Zgbdceg 1eZiZg#\ZgbdcegZ5b^a#WZ3 HZXgZiVgn >bbZY^ViZEVhiEgZh^YZci 9gHVgV]AdX`aZn 1hejbhhZXgZiVgn5\bV^a#Xdb3 9gCdZb^7^iiZgbVc 1cdZb^W5im#iZX]c^dc#VX#^a3 IgZVhjgZg EVhiEgZh^YZci 9g<jnL^aa^Vbh 1hejbh5[VhibV^a#cZi3 9gGVb^gd8Va^"8dgaZd 1^gdXVa^5YVcZjgdeZ#dg\3 :YjXVi^dcD[ÄXZg =dcdgVgnHZXgZiVgn 9g9Vk^YHbVgi 1YVk^Y#hbVgi5Y]]h#iVh#\dk#Vj3 9g?dZg\HX]bjio 1_dZg\#hX]bjio5]^c#X]3 EjWa^XD[ÄXZg BZbWZgViAVg\Z'%%, 9gKVcZhhV=VaaZg 1kVcZhhV#]VaaZg5XYbX#Xdb#Vj3 9gE]^a7gnhdc 1e]^a#Wgnhdc5YYgX#dg\3 8]V^gbVc6CO=B< BZbWZgViAVg\Z'%%+ 9g9Vk^YHbVgi 1YVk^Y#hbVgi5Y]]h#iVh#\dk#Vj3 Egd[#BV^YZ8^bh^i 1bX^bh^i5^hiVcWja#ZYj#ig3 8dbb^iiZZBZbWZgh BZbWZgViAVg\Z'%%* 9g<aZc=Vl`^ch 1]Vl`ZnZ5hl^[iYha#Xdb#Vj3 9g6gb^c@ZbbZg 1Vgb^c5`ZbbZgh#YZ3 9gHVgV]H]Vg`Zn 1hVgV]#h]Vg`Zn5YZ[ZcXZ#\dk#Vj3 9gHXdiiHfj^gZh 1hXdii#hfj^gZh5YZ[ZcXZ#\dk#Vj3 69B>C>HIG6I>DC 69B>C>HIG6I>DC BZbWZgh]^e =dcdgVgnIgZVhjgZgBZbWZgh]^eHZXgZiVgn HiZkZ<dWaZ 1hejbhVYb5W^\edcY#cZi#Vj3 EVig^X^VLddY^c\ &+7jghZab6kZcjZ!=V^cVjai!>a[dgY B:B7:GH=>E :hhZm!><+(:=!Jc^iZY@^c\Ydb -
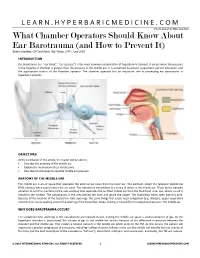
What Chamber Operators Should Know About Ear Barotrauma (And How to Prevent It) Robert Sheffield, CHT and Kevin “Kip” Posey, CHT / June 2018
LEARN.HYPERBARICMEDICINE.COM International ATMO Education What Chamber Operators Should Know About Ear Barotrauma (and How to Prevent It) Robert Sheffield, CHT and Kevin “Kip” Posey, CHT / June 2018 INTRODUCTION Ear barotrauma (i.e. “ear block”, “ear squeeze”) is the most common complication of hyperbaric treatment. It occurs when the pressure in the hyperbaric chamber is greater than the pressure in the middle ear. It is prevented by patient assessment, patient education, and the appropriate actions of the chamber operator. The chamber operator has an important role in preventing ear barotrauma in hyperbaric patients. OBJECTIVES At the conclusion of this article, the reader will be able to: Describe the anatomy of the middle ear Explain the mechanism of ear barotrauma Describe 3 techniques to equalize middle ear pressure ANATOMY OF THE MIDDLE EAR The middle ear is an air space that separates the external ear canal from the inner ear. The eardrum, called the tympanic membrane (TM), vibrates when sound enters the ear canal. The vibration is transmitted to a series of bones in the middle ear. These bones transmit vibration to another membrane (the oval window) that separates the air‐filled middle ear from the fluid‐filled inner ear, where sound is sensed in the cochlea. The nasopharynx is the area behind the nose and above the palate. The Eustachian tubes open into this area. Because of the location of the Eustachian tube openings, the same things that cause nasal congestion (e.g. allergies, upper respiratory infection) can cause swelling around the opening of the Eustachian tubes, making it more difficult to equalize pressure in the middle ear. -

Hypothermia and Respiratory Heat Loss While Scuba Diving
HYPOTHERMIA AND RESPIRATORY HEAT LOSS WHILE SCUBA DIVING Kateřina Kozáková Faculty of Physical Education and Sport, Charles University in Prague, Department of Biomedical Labo- ratory Abstract One of the factors affecting length of stay under water of a diver is heat comfort. During scuba diving there is an increased risk of hypothermia. Hypothermia is one of the most life threatening factors of a diver and significantly affects his performance. The body heat loss runs by different mechanisms. One of them is the respiratory mechanism, which is often overlooked. Compressed dry air or other media is coming out from the cylinder, which have to be heated and humidified to a suitable value. Thus the organism loses body heat and consequently energy. Based on literature search the article will describe safe dive time in terms of hypo- thermia in connection to respiratory heat loss. Key words: hypothermia, heat loss, respiration, scuba diving, water environment Souhrn Jedním z faktorů ovlivňujících délku pobytu potápěče pod vodou je tepelný komfort. Během výkonu přístro- jového potápění hrozí zvýšené riziko hypotermie. Hypotermie představuje jedno z nejzávažnějších ohrožení života potápěče a zásadně ovlivňuje jeho výkon. Ke ztrátám tělesného tepla dochází různými mechanismy. Jednou cestou tepelných ztrát je ztráta tepla dýcháním, která je často opomíjená. Z potápěčského přístroje vychází suchý stlačený vzduch nebo jiné médium, který je třeba při dýchání ohřát a zvlhčit na potřebnou hodnotu. Tím organismus ztrácí tělesné teplo a potažmo energii. Tento článek, na základě literární rešerše, popíše bezpečnou dobou ponoru z hlediska hypotermie a v souvislosti se ztrátou tepla dýcháním. Klíčová slova: hypotermie, ztráta tepla, dýchání, přístrojové potápění, vodní prostředí Introduction amount of body heat. -

Alterations in the Specific Gravity of the Blood Plasma with Onset of Diuresis in Heart Failure
MECHANISM OF DIURESIS: ALTERATIONS IN THE SPECIFIC GRAVITY OF THE BLOOD PLASMA WITH ONSET OF DIURESIS IN HEART FAILURE Harold J. Stewart J Clin Invest. 1941;20(1):1-6. https://doi.org/10.1172/JCI101189. Research Article Find the latest version: https://jci.me/101189/pdf MECHANISM OF DIURESIS: ALTERATIONS IN THE SPECIFIC GRAVITY OF THE BLOOD PLASMA WITH ONSET OF DIURESIS IN HEART FAILURE By HAROLD J. STEWART (From the Department of Medicine of.the New York Hospital and Cornell University Medical College and the Hospital of the Rockefeller Institute for Medical Research, New York) (Received for publication July 3, 1940) There are divergent views concerning the Moreover, its duration may be brief before res- mechanism by which diuresis is initiated. Many toration is attempted, or it may be long enough of the observations on this subject relate to mer- and of such magnitude that it can be detected. curial drugs. Crawford and McIntosh (1) con- On the other hand, if diuresis is initiated at cluded that novasurol induced primary dilution, the tissue side of the system so that fluid enters followed by concentration of the blood in edema- the blood stream first, dilution of the blood would tous patients. Bryan, Evans, Fulton, and Stead occur. Equilibrium would be disturbed until the (2) thought that salyrgan resulted in concentra- kidneys began to excrete the surplus fluid. If di- tion of the blood, since sustained rise in its spe- lution of the blood was of sufficient duration and cific gravity occurred coincident with diuresis in magnitude, it might be detected. -

Critical Care in the Monoplace Hyperbaric Chamber
Critical Care in the Monoplace Hyperbaric Critical Care - Monoplace Chamber • 30 minutes, so only key points • Highly suggest critical care medicine is involved • Pitfalls Lindell K. Weaver, MD Intermountain Medical Center Murray, Utah, and • Ventilator and IV issues LDS Hospital Salt Lake City, Utah Key points Critical Care in the Monoplace Chamber • Weaver LK. Operational Use and Patient Care in the Monoplace Chamber. In: • Staff must be certified and experienced Resp Care Clinics of N Am-Hyperbaric Medicine, Part I. Moon R, McIntyre N, eds. Philadelphia, W.B. Saunders Company, March, 1999: 51-92 in CCM • Weaver LK. The treatment of critically ill patients with hyperbaric oxygen therapy. In: Brent J, Wallace KL, Burkhart KK, Phillips SD, and Donovan JW, • Proximity to CCM services (ed). Critical care toxicology: diagnosis and management of the critically poisoned patient. Philadelphia: Elsevier Mosby; 2005:181-187. • Must have study patient in chamber • Weaver, LK. Critical care of patients needing hyperbaric oxygen. In: Thom SR and Neuman T, (ed). The physiology and medicine of hyperbaric oxygen therapy. quickly Philadelphia: Saunders/Elsevier, 2008:117-129. • Weaver LK. Management of critically ill patients in the monoplace hyperbaric chamber. In: Whelan HT, Kindwall E., Hyperbaric Medicine Practice, 4th ed.. • CCM equipment North Palm Beach, Florida: Best, Inc. 2017; 65-95. • Without certain modifications, treating • Gossett WA, Rockswold GL, Rockswold SB, Adkinson CD, Bergman TA, Quickel RR. The safe treatment, monitoring and management -

Diving Center Rates
IndividualIndividual RatesRates PackagePackage RatesRates Reservation and Transportation Information "LADY KEY DIVER" 40' Custom Dive Boat awaits your Charter at Special Low Rates COAST GUARD INSPECTED & APPROVED • QUALIFIED CREW LEAD-SHOT RENTAL WEIGHTS ON BOARD• FRESHWATER SHOWER SEATS WITH TANKS AT BACK AND GEAR STORAGE UNDER STEREO SOUND SYSTEM • EASY ENTRY AND EXIT • FAST • ROOMY • COMFORTABLE BobBob BrBraayman'syman's Where there are more things to do underwater than in any other place in the United States. OVER 40 SPECIES OF CORAL WRECK DIVING • SHALLOW OR DEEP DIVING • SHELTERED AREAS YEAR-ROUND SUMMER TEMPERATURES 5050 Overseas Highway • MM 50 SPEARFISH • LOBSTER • NIGHT DIVING Marathon, FL. Keys 33050 PLENTIFUL MARINE LIFE • NITROX 1-800-331-HALL(4255) TREASURE HUNTING • REBREATHERS FAX (305) 743-8168 TROPICAL FISH COLLECTING (305) 743-5929 E-Mail: [email protected] Volume 29 - June 2019 Website: www.Hallsdiving.com Reservations & Booking Diving Reef Trips Daily for Scuba or Snorkeling RESERVATIONS: Call (305) 743-5929 or 1-800-331-HALL Two Locations with Time for Diving Two Tanks of Air (4255), FAX (305)743-8168 • 9 A.M. to 6 P.M. For complete details, on the Dive Center offerings, see our complete maga- DAY DIVES: zine brochure. Sombrero, Delta Shoal Area, Thunderbolt Wreck, Coffins Patch DEPOSITS: A $100.00 deposit per person or the total amount or any area less than 10 miles away (4 hours trip time) (whichever is lower) is due 7 days from the request for Check-In: 9:00 A.M. or 1:00 in the afternoon reservations. Departs: 9:30 A.M. and 1:30 in the afternoon FINAL PAYMENT: The final payment is due 14 days before arrival. -

PROLOGUE If I Die, It Will Be in the Most Glorious Place That Nobody
PROLOGUE 2001 If I die, it will be in the most glorious place that nobody has ever seen. I can no longer feel the fingers in my left hand. The glacial Antarctic water has seeped through a tiny puncture in my formerly waterproof glove. If this water were one-tenth of a degree colder, the ocean would become solid. Fighting the knife-edged freeze is depleting my strength, my blood vessels throbbing in a futile attempt to deliver warmth to my extremities. The archway of ice above our heads is furrowed like the surface of a golf ball, carved by the hand of the sea. Iridescent blue, Wedgwood, azure, cerulean, cobalt, and pastel robin’s egg meld with chalk and silvery alabaster. The ice is vibrant, bright, and at the same time ghostly, shadowy. The beauty contradicts the danger. We are the first people to cave dive inside an iceberg. And we may not live to tell the story. It’s February, in the middle of what passes for summer in Antarctica. My job, for National Geographic, is to lead an advanced technical diving team in search of underwater caves deep within the largest moving object on earth, the B-15 iceberg. I had known that diving into tunnels inside this giant piece of ice would be difficult, but I hadn’t calculated that getting out would be nearly impossible. The tidal currents accelerated so quickly that they’ve caged us inside the ice. We’re trapped in this frozen fortress, and I have to figure out how to escape. -

T1, U-2 and L1 Transmitters™ Software V3.06 April 22, 2014
™ Air Integrated Dive Computer User Manual ™ Air Integrated Dive Computer Software v1.18 Ultrasonic software v1.11 And T1, U-2 and L1 Transmitters™ Software v3.06 April 22, 2014 Liquivision Products, Inc -1- Manual 1.6; Lynx 1.18; US 1.11; U-2 3.06 ™ Air Integrated Dive Computer User Manual CONTENTS IMPORTANT NOTICES ............................................................................................................................... 8 Definitions ..................................................................................................................................................... 9 User Agreement and Warranty ....................................................................................................................... 9 User Manual .................................................................................................................................................. 9 Liquivision Limitation of Liability ............................................................................................................... 10 Trademark Notice ........................................................................................................................................ 10 Patent Notice ............................................................................................................................................... 10 CE ............................................................................................................................................................... 10 LYNX -

THE PHYSICIAN's GUIDE to DIVING MEDICINE the PHYSICIAN's GUIDE to DIVING MEDICINE Tt",,.,,,,., , ••••••••••• ,
THE PHYSICIAN'S GUIDE TO DIVING MEDICINE THE PHYSICIAN'S GUIDE TO DIVING MEDICINE tt",,.,,,,., , ••••••••••• , ......... ,.", •••••••••••••••••••••••• ,. ••. ' ••••••••••• " .............. .. Edited by Charles W. Shilling Catherine B. Carlston and Rosemary A. Mathias Undersea Medical Society Bethesda, Maryland PLENUM PRESS • NEW YORK AND LONDON Library of Congress Cataloging in Publication Data Main entry under title: The Physician's guide to diving medicine. Includes bibliographies and index. 1. Submarine medicine. 2. Diving, Submarine-Physiological aspects. I. Shilling, Charles W. (Charles Wesley) II. Carlston, Catherine B. III. Mathias, Rosemary A. IV. Undersea Medical Society. [DNLM: 1. Diving. 2. Submarine Medicine. WD 650 P577] RC1005.P49 1984 616.9'8022 84-14817 ISBN-13: 978-1-4612-9663-8 e-ISBN-13: 978-1-4613-2671-7 DOl: 10.1007/978-1-4613-2671-7 This limited facsimile edition has been issued for the purpose of keeping this title available to the scientific community. 10987654 ©1984 Plenum Press, New York A Division of Plenum Publishing Corporation 233 Spring Street, New York, N.Y. 10013 All rights reserved No part of this book may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, microfilming, recording, or otherwise, without written permission from the Publisher Contributors The contributors who authored this book are listed alphabetically below. Their names also appear in the text following contributed chapters or sections. N. R. Anthonisen. M.D .. Ph.D. Professor of Medicine University of Manitoba Winnipeg. Manitoba. Canada Arthur J. Bachrach. Ph.D. Director. Environmental Stress Program Naval Medical Research Institute Bethesda. Maryland C. Gresham Bayne.