Four Cases of Right-Sided Bundle-Branch Block and One Case of Atrioventricular Block in Three Generations of a Family
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Postural Heart Block*
Br Heart J: first published as 10.1136/hrt.44.2.221 on 1 August 1980. Downloaded from Case reports Br Heart J 1980; 44: 221-3 Postural heart block* PETER E SEDA, JOHN H McANULTY, C JOE ANDERSON From the Department of Medicine, University of Oregon Health Sciences Center, Portland, Oregon, USA SUMMARY A patient presented with orthostatic dizziness and syncope caused by postural heart block. When the patient was supine, atrioventricular conduction was normal and he was asymptomatic; when he was standing he developed second degree type II block and symptoms. The left bundle-branch block on his electrocardiogram and intracardiac electrophysiological study findings suggest that this heart block occurred distal to the His bundle. Orthostatic symptoms are usually presumed to be secondary to an inappropriate distribution of intravascular volume or to autonomic nervous system abnormalities. As shown in this patient, these symptoms may be the result of orthostatic heart block. Ambulatory monitoring may be useful in patients with orthostatic neurological symptoms, particularly when conduction abnormalities are present on the electrocardiogram. Orthostatic neurological symptoms usually result minute and regular, and increased to 90 beats a from inadequate cerebral perfusion caused by minute with some irregularity when he was upright. disturbances of the autonomic nervous system,'-3 The carotid pulse was normal, and there were no ineffective or inappropriate shifts in volume carotid bruits. The cardiac impulse was normal. http://heart.bmj.com/ distribution,4 or drugs.5 We report a patient with The second heart sound was paradoxically split. orthostatic dizziness and syncope caused by inter- There was a grade 2/6 apical systolic murmur. -
The Frequency of Rhythm and Conduction Abnormalities and Benefits of 24-Hour Holter Electrocardiogram on Detecting These Abnormalities
ORIGINAL ARTICLE East J Med 24(3): 303-309, 2019 DOI: 10.5505/ejm.2019.31932 The Frequency of Rhythm and Conduction Abnormalities and Benefits of 24-Hour Holter Electrocardiogram on Detecting These Abnormalities In Patients With Acute Rheumatic Fever Serdar Epçaçan*, Yasemin Nuran Dönmez University of Health Sciences, Van Training and Research Hospital, Department of Pediatric Cardiology, Van, Turkey ABSTRACT During the acute phase of acute rheumatic fever (ARF), cardiac arrhythmias and conduction disorders may occur. Standard electrocardiogram (ECG) may be insufficient in the cases of possible paroxysmal rhythm or conduction abnormalities. The aim of this study is to evaluate arrhythmias and conduction disorders and benefits of 24-hour Holter ECG on detecting these disorders in children with ARF. Two hundred and ten patients who were diagnosed with ARF during a four-year period, were retrospectively analyzed. Demographic characteristics, clinical, laboratory, and echocardiographic findings of the patients were evaluated. Standard ECG and 24-hour Holter analysis were examined. First (47.8%), second (6.9%) and third degree (4.3%) atrioventricular (AV) blocks, bundle branch blocks (9.8%), intermittent pre-excitation (1.1%), accelerated nodal rhythm (15.2%), supraventricular (10.9%) and ventricular premature contractions (8.7%), as well as supraventricular (3.3%) and ventricular tachycardia (1.1%) were detected with 24 -hour Holter ECG. Frequency of both rhythm and conduction abnormalities were detected higher with Holter ECG than 12-lead ECG, and this was statistically significant (p<0.05). Second degree type II AV block and non-sustained supraventricular tachycardia as well as intermittent complete AV block were detected on 24-hour Holter analysis in patients with normal initial standard ECG. -

Answer: E) Atrial Fibrillation with Complete Heart Block Teaching Point
Answer: e) Atrial fibrillation with complete heart block Teaching Point: A slow regular ventricular rate in a patient with concurrent atrial fibrillation, as seen in this ECG, is diagnostic of complete heart block. Atrial fibrillation creates a diagnostic dilemma for identifying AV nodal disease or block. Close scrutiny should be placed on R-R intervals to identify patterns or regularity (1). Clinicians should be wary of a regular heart rate in a patient with persistent atrial fibrillation, especially in those using digitalis. If an AV nodal block is identified, it may be transient, and a search for reversible causes is indicated as in all cases of complete heart block prior to pacemaker placement. Electrolyte abnormalities, ischemia, and medications remain the leading reversible causes (2,3). The patient in this case was transferred to the Emergency Department and admitted for further observation. Ischemia was ruled out. Carvedilol was held, and he was diuresed. He continued to demonstrate adequate chronotropic response with exertion. The complete heart block soon resolved, and he was diuresed to euvolemia. Pacemaker placement was deferred given the transient nature of the AV block in the context of recent beta-blocker usage. He was discharged home with continuous heart rhythm monitoring without any further evidence of complete heart block. References: 1. Urbach JR, Grauman JJ, Straus SH. Quantitative Methods for the Recognition of Atrioventricular Junctional Rhythms in Atrial Fibrillation. Circulation. 1969; 39: 803- 817. 2. Kojic EM, Hardarson T, Sigfusson N, Sigvaldason H. The prevalence and prognosis of third-degree atrioventricular conduction block: the Reykjavik study. J Intern Med. -

Cardiac Pacing in Incomplete Atrioventricular Block with Atrial Fibrillation
Br Heart J: first published as 10.1136/hrt.35.11.1154 on 1 November 1973. Downloaded from British Heart journal, I973, 35, I154-1I60. Cardiac pacing in incomplete atrioventricular block with atrial fibrillation D. S. Reid, S. J. Jachuck, and C. B. Henderson From the Department of Cardiology, Newcastle General Hospital, Newcastle upon Tyne Three cases with a slow irregular ventricular response to atrialfibrillation, who benefitedfrom cardiac pacing, are described; two had ischaemic heart disease, and one had cardiomyopathy. In thefirst case the slow ventricu- lar response to atrialfibrillation was a result of incomplete atrioventricular nodal block, and in the other two His bundle electrograms demonstrated that the slow ventricular response was due to bilateral bundle-branch block. The association of atrial fibrillation and conduction delays in the atrioventricular node and bundle- branches is discussed. The value of His bundle recordings in the investigation of these cases is shown and the importance of cardiac pacing in treatment is stressed. Cardiac pacing is now a generally accepted method hypotension. Intravenous atropine given before transfer of treatment in patients with complete heart block or had resulted in a paroxysm of ventricular tachycardia. bilateral bundle-branch block who have Adam- On admission there was no evidence of cardiac failure Stokes attacks or a low output to and the blood pressure was I05/50 mmHg. An electro- syndrome leading cardiogram showed atrial fibrillation with an irregular angina or cardiac failure. cardiac is However, pacing ventricular response of 40 to 44 beats a minute and acute now also becoming more widely used in the treat- inferolateral myocardial infarction (Fig. -
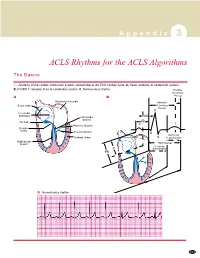
ACLS Rhythms for the ACLS Algorithms
A p p e n d i x 3 ACLS Rhythms for the ACLS Algorithms The Basics 1. Anatomy of the cardiac conduction system: relationship to the ECG cardiac cycle. A, Heart: anatomy of conduction system. B, P-QRS-T complex: lines to conduction system. C, Normal sinus rhythm. Relative Refractory A B Period Bachmann’s bundle Absolute Sinus node Refractory Period R Internodal pathways Left bundle AVN branch AV node PR T Posterior division P Bundle of His Anterior division Q Ventricular Purkinje fibers S Repolarization Right bundle branch QT Interval Ventricular P Depolarization PR C Normal sinus rhythm 253 A p p e n d i x 3 The Cardiac Arrest Rhythms 2. Ventricular Fibrillation/Pulseless Ventricular Tachycardia Pathophysiology ■ Ventricles consist of areas of normal myocardium alternating with areas of ischemic, injured, or infarcted myocardium, leading to chaotic pattern of ventricular depolarization Defining Criteria per ECG ■ Rate/QRS complex: unable to determine; no recognizable P, QRS, or T waves ■ Rhythm: indeterminate; pattern of sharp up (peak) and down (trough) deflections ■ Amplitude: measured from peak-to-trough; often used subjectively to describe VF as fine (peak-to- trough 2 to <5 mm), medium-moderate (5 to <10 mm), coarse (10 to <15 mm), very coarse (>15 mm) Clinical Manifestations ■ Pulse disappears with onset of VF ■ Collapse, unconsciousness ■ Agonal breaths ➔ apnea in <5 min ■ Onset of reversible death Common Etiologies ■ Acute coronary syndromes leading to ischemic areas of myocardium ■ Stable-to-unstable VT, untreated ■ PVCs with -

A Case of Long QT Syndrome
CASE REPORT A case of long QT syndrome: challenges on a bumpy road Peter Magnusson1,2 & Per-Erik Gustafsson2 1Cardiology Research Unit, Department of Medicine, Karolinska Institutet, Stockholm SE-171 76, Sweden 2Centre for Research and Development, Uppsala University/Region Gavleborg,€ Gavle€ SE-801 87, Sweden Correspondence Key Clinical Message Peter Magnusson, Cardiology Research Unit, Department of Medicine, Karolinska Beta-agonist treatment during pregnancy may unmask the diagnosis of long QT Institutet, Karolinska University Hospital/ syndrome. The QT prolongation can result in functional AV block. A history of Solna, SE-171 76 Stockholm, Sweden. Tel: seizure and/or sudden death in a family member should raise suspicion of ven- +46(0)705 089407; Fax: +46(0)26 154255; tricular tachycardia. More than one mutation may coexist. Refusal of beta- E-mail: [email protected] blocker therapy complicates risk stratification. Funding Information Keywords No sources of funding were declared for this Genetic, implantable cardioverter–defibrillator, long QT syndrome, pregnancy, study. premature ventricular complex, risk stratification, sudden cardiac death. Received: 16 December 2016; Revised: 29 March 2017; Accepted: 4 April 2017 Clinical Case Reports 2017; 5(6): 954–960 doi: 10.1002/ccr3.985 Introduction experienced palpitations, and her ECG was abnormal, revealing PVCs, atrioventricular (AV) 2:1 block and QT Long QT syndrome (LQTS) is linked to mutations in the prolongation (520 msec) in precordial lead V5 during ion channels, which can lead to disturbances in ventricu- sinus rhythm at 90 beats per minute (Fig. 1) and rhythm lar repolarization [1]. This condition puts patients at risk strip while walking (Fig. -
Neurological Associations of Chronic Heart Block
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.39.6.571 on 1 June 1976. Downloaded from Journal ofNeurology, Neurosurgery, andPsychiatry, 1976, 39, 571-575 Neurological associations of chronic heart block C. D. LAMBERT AND A. J. FAIRFAX From the Departments of Neurology and Cardiology, St. George's Hospital, London SYNOPSIS A large group of patients with chronic heart block was studied for evidence of neurological disorder. Six out of 892 patients were found who had neuromuscular disease related to the conduction disturbance. In four patients, cardiac involvement appeared selectively to affect the conducting tissues. Three of these patients had a scapuloperoneal syndrome, the fourth, the oculocraniosomatic syndrome. In the remaining two patients, one with limb girdle dystrophy and the other with dystrophia myotonica, cardiomyopathy was present in addition to the conduction disturbance. This paper reports the first comprehensive with incomplete heart block or transient heart study of the frequency and nature of neuro- block secondary to myocardial infarction were not Protected by copyright. logical disorders occurring in association with included. complete heart block. The most common Those cases with evidence of neuromuscular disease were examined in detail, a family history pathological cause of chronic heart block is taken, serum creatine phosphokinase levels meas- idiopathic bundle branch fibrosis (Davies, ured and, when possible, electromyography per- 1971) thought by Lenegre, who described it, to formed. Muscle biopsy specimens, obtained under be a selective myopathy of the cardiac con- local anaesthetic, were examined using conven- ducting 'tissues (Lenegre, 1964). His original tional morphological and histochemical techniques series of 66 cases contained two patients with (Dubowitz and Brooke, 1973). -

Where's the PAC?
Where’s the PAC? A junctional premature contraction (JPC) is a beat that originates prematurely in the AV node. It can occur sporadically or in a grouped pattern. Junctional If PR interval is present, it does NOT represent atrial stimulation of Premature the ventricles. Contraction (JPC) PVC What is this called? Bigeminy - every other beat Trigeminy - every third beat Quadrigeminy - every fourth beat Just how mad Couplets - two in a row are you?? Triplets - three in a row V-Tach - 5 or more PVC’s Multifocal – More than one focus PVC Couplet Multifocal Bigeminy Trigeminy Quadrageminy BBB Hemiblock You are driving into the EKG. You need to turn. You signal. Right or left. Bundle Branch BLOCKS J point: the junction between the end of the QRS segment and the beginning of the ST segment Turn signal theory - Courtesy of Mike Taigman Advanced Field Cardiology “Drive your car” Aortic stenosis Dilated cardiomyopathy LBBB AMI/Extensive CAD Causes Primary disease of the cardiac electrical conduction system Long standing hypertension leading to aortic root dilatation = aortic regurgitation •RVH / Cor pulmonale •PE RBBB •Ischemic heart disease Causes •Rheumatic heart disease •Myocarditis or cardiomyopathy •Degeneration of conduction system “Drive your car” AV Blocks What is actually blocked? A vessel? Is something really “blocked?” Heart Blocks Defined by PR Interval First-Degree Regularity: Regular Heart Block P wave: Normal PR interval: Prolonged >0.20 sec QRS width: Normal Syncopal episode – is this the culprit? First degree AV block is a constant and prolonged PR interval Insult to AV node, hypoxemia, Inferior MI, dig st toxicity, ischemia of the conduction system and 1 Degree AV increased vagal tone Block Criteria Rhythm: Regular PRI: > .20 Degree 2nd Regularity: Regularly irregular AV Block - P wave: Present Type I PR interval: Variable QRS width: Normal Dropped beats: Yes, patterned Long, Longer, Longest, DROP! Rinse and repeat. -

Pharmacological Treatment of Chronic Stable Angina Pectoris
■ DRUG THERAPIES IN... Clinical Medicine 2013, Vol 13, No 1: 63–70 Pharmacological treatment of chronic stable angina pectoris Jason M Tarkin and Juan Carlos Kaski ABSTRACT – Chronic stable angina is the most common Overview of chronic stable angina manifestation of ischaemic heart disease in the developed world and is associated with impaired quality of life and The term angina pectoris refers to William Heberden’s classic increased mortality. The pathogenesis of stable angina is description of the clinical symptoms of angina, as reported to 1 complex and often, albeit not always, involves flow-limiting the Royal College of Physicians in 1768. There is currently no epicardial coronary artery stenoses (atheromatous plaques) systematically agreed definition for angina pectoris and the that reduce the ability of the coronary circulation to deliver term is used to define both the typical chest pain associated appropriate blood supply to the myocardium. The coronary with myocardial ischaemia and the syndrome characterised by microcirculation can also play an important role. An imbal- chest pain, myocardial ischaemia and obstructive atheroscle- ance between myocardial oxygen supply and metabolic rotic coronary artery disease. In this article, we use the term oxygen demand causes the symptoms of angina pectoris ‘angina’ in relation to the occurrence of typical central chest and represents a major therapeutic target. Rational treat- pain associated with myocardial ischaemia, irrespective of the ment requires a multi-faceted approach combining lifestyle presence or absence of flow-limiting organic coronary artery changes, aggressive management of modifiable coronary stenosis. artery disease risk factors, pharmacological therapy and Angina is considered to be ‘chronic’ and ‘stable’ when symp- myocardial revascularisation when appropriate. -

Lyme Carditis Airley E
Infect Dis Clin N Am 22 (2008) 275–288 Lyme Carditis a b Airley E. Fish, MD, MPH , Yuri B. Pride, MD , a, Duane S. Pinto, MD * aDivision of Cardiology, Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, 1 Deaconess Road, Palmer 415, Boston, MA 02215, USA bDepartment of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, 330 Brookline Avenue, Deaconess 311, Boston, MA 02215, USA Lyme borreliosis, or Lyme disease, is a globally occurring, systemic disease caused by the spirochete Borrelia burgdorferi and transmitted by the Ixodes tick. The disease classically is divided into three stages. Stage 1, the early localized stage, generally occurs several days or up to 1 month after the initial tick bite. It is notable for an influenza-like illness and often is accompanied by the erythema migrans (EM) rash. Stage 2, the early dissem inated stage, occurs weeks to months after EM. Neurologic symptoms and musculoskeletal complaints are the hallmarks of this stage. Cardiac abnor malities, predominantly involving the conduction system and myocardium, also may manifest at this time. Stage 3 occurs several months to years after EM and is characterized by a monoarthritis or oligoarthritis affecting the large joints, and the development and progression of neurologic sequelae. Steere and colleagues first described the cardiovascular complications of Lyme disease nearly 30 years ago in a retrospective report of 20 North American cases. Australian and European cases were reported in the early to mid-1980s. The principal manifestation of Lyme carditis is self-limited conduction derangement, most commonly involving the atrioventricular node. -

Firstdegree AV Blockan Entirely Benign Finding Or a Potentially
REVIEW ARTICLE First-Degree AV Block—An Entirely Benign Finding or a Potentially Curable Cause of Cardiac Disease? ∗ ∗ Fredrik Holmqvist, M.D., Ph.D. † and James P. Daubert, M.D. ∗ From the Clinical Cardiac Electrophysiology, Duke University Medical Center, Durham, NC; and †Department of Cardiology, Lund University, Lund, Sweden First-degree atrioventricular (AV) block is a delay within the AV conduction system and is defined as a prolongation of the PR interval beyond the upper limit of what is considered normal (generally 0.20 s). Up until recently, first-degree AV block was considered an entirely benign condition. In fact, some complain that it is a misnomer since there is only delay and no actual block in the AV conduction system (usually within the AV node). However, it has long been acknowledged that extreme forms of first-degree AV block (typically a PR interval exceeding 0.30 s) can cause symptoms due to inadequate timing of atrial and ventricular contractions, similar to the so-called pacemaker syndrome. Consequently, the current guidelines state that permanent pacemaker implantation is reasonable for first-degree AV block with symptoms similar to those of pacemaker syndrome or with hemodynamic compromise, but also stresses that there is little evidence to suggest that pacemakers improve survival in patients with isolated first-degree AV block. Recent reports suggest that it may be time to revisit the impact of first-degree AV block. Also, several findings in post hoc analyses of randomized device trials give important insights in possible treatment options. The present review aims to provide an update on the current knowledge concerning the impact of first-degree AV block and also to address the issue of pacing in patients with this condition. -
Heart Rhythms
Heart rhythms Coronary heart disease is the UK’s single biggest killer. For over 50 years we’ve pioneered research that’s transformed the lives of people living with heart and circulatory conditions. Our work has been central to the discoveries of vital treatments that are changing the fight against heart disease. But so many people still need our help. From babies born with life-threatening heart problems to the many Mums, Dads and Grandparents who survive a heart attack and endure the daily battles of heart failure. Join our fight for every heartbeat in the UK. Every pound raised, minute of your time and donation to our shops will help make a difference to people’s lives. ©British Heart Foundation 2013, registered charity in England and Wales (225971) and in Scotland (SCO39426) HIS14/0512 About the British Heart Foundation The British Heart Foundation (BHF) is the nation’s heart charity, saving lives through pioneering research, patient care and vital information. What you can do for us We rely on donations of time and money to continue our life-saving work. If you would like to make a donation, please: • call our donation hotline on 0300 330 3322 • visit bhf.org.uk/donate, or • post it to us at the address on the back cover. If you wish to make a gift to the BHF in your will, call 0844 847 2787 or email [email protected] and ask for our free booklet, My generation. For other ways to support our work, see bhf.org.uk/ supportus You may find other useful information on our website at: bhf.org.uk Contents About this booklet .......................................................................