HL7 Standards Manual
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Googling the Grey: Open Data, Web Services, and Semantics
Archaeologies: Journal of the World Archaeological Congress (Ó 2010) DOI 10.1007/s11759-010-9146-4 Googling the Grey: Open Data, Web Services, and Semantics Eric C. Kansa, School of Information, UC Berkeley, Berkeley, CA, USA E-mail: [email protected] RESEARCH Sarah Whitcher Kansa, Alexandria Archive Institute, San Francisco, CA, USA Margie M. Burton and Cindy Stankowski, San Diego Archaeological Center, Escondido, CA, USA ABSTRACT ________________________________________________________________ Primary data, though an essential resource for supporting authoritative archaeological narratives, rarely enters the public record. Lack of primary data publication is also a major obstacle to cultural heritage preservation and the goals of cultural resource management (CRM). Moreover, access to primary data is key to contesting claims about the past and to the formulation of credible alternative interpretations. In response to these concerns, experimental systems have implemented a variety of strategies to support online publication of primary data. Online data dissemination can be a powerful tool to meet the needs of CRM professionals, establish better communication and collaborative ties with colleagues in academic settings, and encourage public engagement with the documented record of the past. This paper introduces the ArchaeoML standard and its implementation in the Open Context system. As will be discussed, the integration and August 2010 online dissemination of primary data offer great opportunities for making archaeological knowledge creation more participatory and transparent. However, different strategies in this area involve important trade-offs, and all face complex conceptual, ethical, legal, and professional challenges. ________________________________________________________________ Volume 6 Number 2 Since Open Context is operated in the United States, the European Union’s database protection laws are less applicable. -

Foundations of Temporal Text Networks
Vega et al. Applied Network Science (2018) 3:25 Applied Network Science https://doi.org/10.1007/s41109-018-0082-3 RESEARCH Open Access Foundations of Temporal Text Networks Davide Vega* and Matteo Magnani *Correspondence: [email protected] Abstract InfoLab, Department of Information Three fundamental elements to understand human information networks are the Technology, Uppsala University, Uppsala, Sweden individuals (actors) in the network, the information they exchange, that is often observable online as text content (emails, social media posts, etc.), and the time when these exchanges happen. An extremely large amount of research has addressed some of these aspects either in isolation or as combinations of two of them. There are also more and more works studying systems where all three elements are present, but typically using ad hoc models and algorithms that cannot be easily transfered to other contexts. To address this heterogeneity, in this article we present a simple, expressive and extensible model for temporal text networks, that we claim can be used as a common ground across different types of networks and analysis tasks, and we show how simple procedures to produce views of the model allow the direct application of analysis methods already developed in other domains, from traditional data mining to multilayer network mining. Keywords: Network, Text, Time, Model, Temporal text network, Human information network Introduction A large amount of human-generated information is available online in the form of text exchanged between individuals at specific times. Examples include social network sites, online forums and emails. The public accessibility of several of these sources allows us to observe our society at various scales, from focused conversations among small groups of individuals to broad political discussions involving heterogeneous audiences from large geographical areas (Zhou et al. -

Database-Driven Web Mashups
Database-Driven Web Mashups Andrei Vancea Michael Grossniklaus Moira C. Norrie Institute for Information Systems ETH Zurich CH-8092 Zurich, Switzerland {vancea,grossniklaus,norrie}@inf.ethz.ch Abstract news feeds being combined into a single feed. An enterprise mashup uses the general mashup techniques within a com- In most web mashup applications, the content is gener- pany’s own internal applications. It usually combines data ated using either web feeds or an application programming from both internal and external sources. Finally, a business interface (API) based on web services. Both approaches mashup is a combination of all of the above that makes the have limitations. Data models provided by web feeds are result available for a business application. not powerful enough to permit complex data structures to In this paper, we argue that current approaches to the de- be transmitted. APIs based on web services are usually velopment of web mashup applications lack a powerful data different for each web application, and thus different im- model for data interchange. As mentioned above, in most plementations of the APIs are required for each web ser- cases, the content is generated using feeds or an applica- vice that a web mashup application uses. We propose a tion programming interface (API) based on web services. database-driven approach to web mashups that supports In the former case, the data models provided by web feeds integration at the database level and enables mashup de- (RSS or Atom) lack flexibility and do not permit complex velopers to work with a uniform abstract model and have data structures to be transmitted. -
Sturbridge, Brimfield, Holland and Wales
SPENCER FAMILY DENTAL Gentle Caring State of the Art Dentistry For The Whole Family Cosmetic Dentistry • Restorative Dentistry • Preventative Dentistry CROWNS • CAPS • BRIDGES • COMPLETE and PARTIAL DENTURES New We Strive NON SURGICAL GUM TREATMENT • ROOT CANAL THERAPY Patients SURGICAL SERVICES For Painless Welcome BREATH CLINIC-WE TREAT CHRONIC BAD BREATH Dentistry HERBAL DENTAL PRODUCTS • All Instruments Fully Sterilized • Most Insurances Accepted Dr. Nasser S. Hanna Conveniently Located On Route 9 • (Corner of Greenville St. & Main St.) 284 Main St., Spencer 508-885-5511 Mailed free to requesting homes in Sturbridge, Brimfield, Holland and Wales Vol. VII, No. 50 PROUD MEDIA SPONSOR OF RELAY FOR LIFE OF THE GREATER SOUTHBRIDGE AREA! COMPLIMENTARY HOME DELIVERY ONLINE: WWW.STURBRIDGEVILLAGER.NET Friday, December 13, 2013 THIS WEEK’S QUOTE Board fields “The only thing that OML complaint overcomes hard luck is CREAMER ACCUSED OF DEFAMATORY COMMENTS hard work.” BY CHELSEA DAVIS Photo courtesy John Shevlin Harry Golden VILLAGER STAFF WRITER This design represents the intersection of Route 20 and Route 131 STURBRIDGE — The Board of becoming a rotary after the proposed improvement plans. Selectmen addressed an Open Meeting Law complaint made against them at their INSIDE Monday, Dec. 2 meeting. “[The written response is] acknowledg- Residents get look ing it was a somewhat awkward discus- ALMANAC ............2 sion,” said Town Administrator Shaun Suhoski. “It addresses the five items that POLICE LOGS........5 were on page 2 of the complaint.” at Route 20 project OPINION ............10 The complaint made by Monique Marinelli, wife of Sturbridge Fire CALENDAR .........12 Lieutenant John Marinelli, mostly BY CHELSEA DAVIS walking distances to these VILLAGER STAFF WRITER OBITUARIES .......12 addressed the alleged fault of former Board facilities, [and] protects and of Selectmen Chairman Thomas Creamer STURBRIDGE — A pres- takes advantage of the SPORTS ............14 in a Nov. -
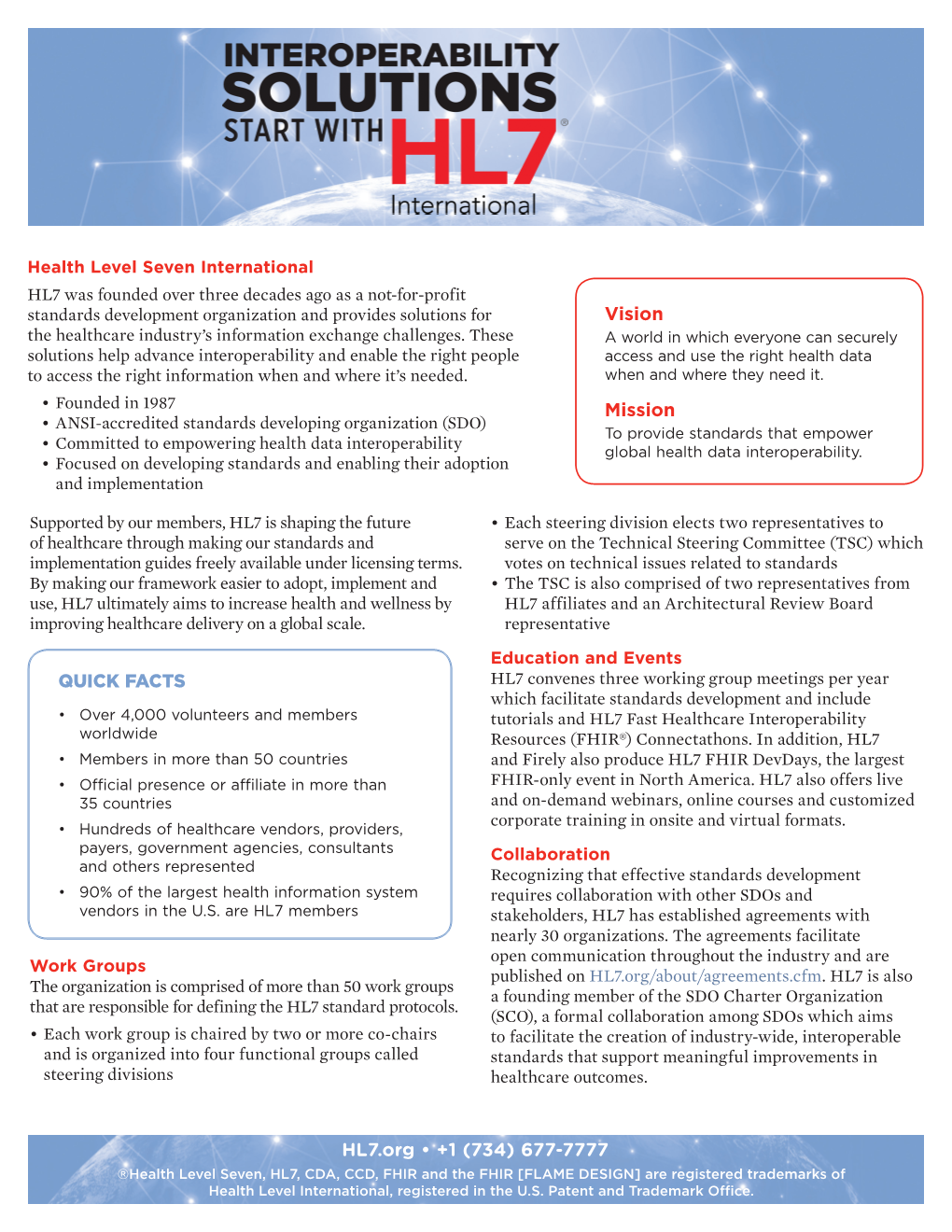
Open Meeting Law, Public Records Law and the Use of Technology
Open Meeting Law, Public Records Law and the Use of Technology Town of Wilmington Mark R. Reich, Esq. November 30, 2020 2 Disclaimer This information is provided as a service by KP Law, P.C. This information is general in nature and does not, and is not intended to, constitute legal advice as to particular issues. Neither the provision nor receipt of this information creates an attorney-client relationship between the presenter and the recipient. You are advised not to take, or to refrain from taking, any action based on this information without consulting legal counsel about the specific issue(s). 3 Municipal Use of Social Media – Legal Issues ■ Open Meeting Law, G.L. c.30A, §§18-25 ■ Communications among a quorum of board members on social media can constitute an open meeting law violation ■ Click here for a discussion of the OML and social media: http://www.k-plaw.com/wp-content/uploads/2017/01/Open- Meeting-Law-and-Social-Media-Potential-Pitfalls.pdf ■ Public Records Law, G.L. c.66, §10 ■ Records retention ■ Policy to retain copies of social media pages and posts ■ Current guidance recommends taking a periodic “snapshot” of the social media sites in order to meet records retention obligations ■ Do not post information that is not public record 4 Open Meeting Law – Overview Massachusetts Open Meeting Law - G.L. c. 30A, §§ 18-25 • Purpose of OML is to eliminate the secrecy surrounding deliberations and decisions on which public policy is based • Applies to “a deliberation by a public body with respect to any matter within the body’s -

Massachusetts Municipal Association Annual Meeting January, 2020 Disclaimer This Information Is Provided As a Service by KP Law, P.C
Massachusetts Municipal Association Annual Meeting January, 2020 Disclaimer This information is provided as a service by KP Law, P.C. This information is general in nature and does not, and is not intended to, constitute legal advice. Neither the provision nor receipt of this information creates an attorney-client relationship between the presenter and the recipient. You are advised not to take, or to refrain from taking, any action based on this information without consulting legal counsel about the specific issue(s). All materials © Copyright 2020 KP Law, P.C. All rights reserved. Overview– Sunshine Laws . Open meeting , public records and conflict of interest laws exist in virtually every state . Purpose of such laws is to eliminate much of the secrecy surrounding deliberations and decisions on which public policy is based . Under the Open Meeting Law (“OML”), public bodies can only conduct business through public meetings, held in accordance with the OML, unless an exemption allowing an executive session exists All materials © Copyright 2020 KP Law, P.C. All rights reserved. OML –Legal Requirements • Meeting Notices/Agendas • Meeting must be properly posted 1) timing 2) location 3) detail • Minutes • Accurate, timely prepared and approved • Verbatim transcripts not required, but significantly detailed • Guidance from AG on process for approving • Attorney General’s Office promulgated revisions to the Open Meeting Law regulations in 2017 All materials © Copyright 2020 KP Law, P.C. All rights reserved. OML –Meetings Meeting includes -

Multilingual Catalogue Strategies
CEN CWA 15992 WORKSHOP July 2009 AGREEMENT ICS 35.240.60 English version Harmonization of data interchange in tourism This CEN Workshop Agreement has been drafted and approved by a Workshop of representatives of interested parties, the constitution of which is indicated in the foreword of this Workshop Agreement. The formal process followed by the Workshop in the development of this Workshop Agreement has been endorsed by the National Members of CEN but neither the National Members of CEN nor the CEN Management Centre can be held accountable for the technical content of this CEN Workshop Agreement or possible conflicts with standards or legislation. This CEN Workshop Agreement can in no way be held as being an official standard developed by CEN and its Members. This CEN Workshop Agreement is publicly available as a reference document from the CEN Members National Standard Bodies. CEN members are the national standards bodies of Austria, Belgium, Bulgaria, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden, Switzerland and United Kingdom. EUROPEAN COMMITTEE FOR STANDARDIZATION COMITÉ EUROPÉEN DE NORMALISATION EUROPÄISCHES KOMITEE FÜR NORMUNG Management Centre: Avenue Marnix 17, B-1000 Brussels © 2009 CEN All rights of exploitation in any form and by any means reserved worldwide for CEN national Members. Ref. No.:CWA 15992:2009 E CWA 15992:2009 (E) Contents Contents -

11 Bio.Tools Studentships 145 11.1 Requirements
bio.tools Documentation Release latest Jul 21, 2021 Contents 1 What is bio.tools? 3 1.1 Objectives................................................3 1.2 Scope...................................................3 1.3 Technical components..........................................4 1.4 bio.tools Tool Identifiers.........................................4 1.5 Docs overview..............................................5 1.6 Getting involved : a quickstart guide...................................5 2 Contributors Guide 7 2.1 bio.tools community site.........................................7 2.2 Feature requests & issues........................................7 2.3 Mailing list................................................7 2.4 Hangouts.................................................8 2.5 Task management............................................8 2.6 Editing tool descriptions.........................................8 3 Quickstart guide 9 3.1 Create an account............................................9 3.2 Add content...............................................9 3.3 Update a resource............................................ 11 3.4 Remove a resource............................................ 12 3.5 Search for a tool............................................. 12 3.6 References................................................ 12 4 Curators Guide 13 4.1 General guidelines............................................ 14 4.2 Attribute guidelines........................................... 17 4.3 Tool type guidelines.......................................... -

Ualbertabusiness
SPRING 2017 THE FUTURE ISSUE LIVE. WORK. LEARN. ualbertabusiness BRIGHT SPOT AHEAD The upside of Canada’s electricity crisis PAGE 20 PAGE 13 PAGE 6 WHEELS OF FORTUNE NEW WORLD ORDER ENGINEERING THRILLS Will ride-shares and AI spell an Trade and turmoil in One man’s quest to build the end to the personal car? the age of Trump ultimate amusement park ride Make a world of difference. Donate and help our students experience life-changing opportunities during their studies. Donations to the Student Experience fund at the Alberta School of Business have an enormous impact. Your support provides students with opportunities that change the way they see the world, and inspires them to pursue their passions. To learn more visit ualberta.ca/business/give or call 1-877-992-7587. SPRING 2017 3 FRONT CONTENTS SPRING 2017 ISSUE A magazine for alumni and friends of the Alberta School of Business FRONT FEATURES DEAN Joseph Doucet 04 Message from the Dean 16 Leading Light SUPERVISING EDITOR 05 From the Web by Michael Hingston Heather Newton Canada’s electricity industry is at a EDITOR Omar Mouallem crossroads and the future is anyone’s guess ART DIRECTOR Make a world of difference. LIVE Sarah Jackson ASSOCIATE EDITOR 20 MaaS Effect Angela Johnston 06 Engineering an by Tim Querengesser ASSISTANT EDITOR Donate and help our students experience life-changing The private vehicle is looking costly, Mike Kendrick Adrenaline Rush wasteful, dirty and plain old passé as more How Guy Nelson got in the business CLASS NOTES EDITOR opportunities during their studies. people take advantage of the “mobility-as- Jacqueline Kokic of thrill rides a-service” ecosystem. -

Oversight of the Federal Communications Commission: the National Broadband Plan
OVERSIGHT OF THE FEDERAL COMMUNICATIONS COMMISSION: THE NATIONAL BROADBAND PLAN HEARING BEFORE THE SUBCOMMITTEE ON COMMUNICATIONS, TECHNOLOGY, AND THE INTERNET OF THE COMMITTEE ON ENERGY AND COMMERCE HOUSE OF REPRESENTATIVES ONE HUNDRED ELEVENTH CONGRESS SECOND SESSION MARCH 25, 2010 Serial No. 111–109 ( Printed for the use of the Committee on Energy and Commerce energycommerce.house.gov U.S. GOVERNMENT PRINTING OFFICE 76–021 WASHINGTON : 2012 For sale by the Superintendent of Documents, U.S. Government Printing Office Internet: bookstore.gpo.gov Phone: toll free (866) 512–1800; DC area (202) 512–1800 Fax: (202) 512–2104 Mail: Stop IDCC, Washington, DC 20402–0001 VerDate Mar 15 2010 04:07 Dec 12, 2012 Jkt 076021 PO 00000 Frm 00001 Fmt 5011 Sfmt 5011 E:\HR\OC\A021.XXX A021 smartinez on DSK6TPTVN1PROD with COMMITTEE ON ENERGY AND COMMERCE HENRY A. WAXMAN, California Chairman JOHN D. DINGELL, Michigan JOE BARTON, Texas Chairman Emeritus Ranking Member EDWARD J. MARKEY, Massachusetts RALPH M. HALL, Texas RICK BOUCHER, Virginia FRED UPTON, Michigan FRANK PALLONE, JR., New Jersey CLIFF STEARNS, Florida BART GORDON, Tennessee NATHAN DEAL, Georgia BOBBY L. RUSH, Illinois ED WHITFIELD, Kentucky ANNA G. ESHOO, California JOHN SHIMKUS, Illinois BART STUPAK, Michigan JOHN B. SHADEGG, Arizona ELIOT L. ENGEL, New York ROY BLUNT, Missouri GENE GREEN, Texas STEVE BUYER, Indiana DIANA DEGETTE, Colorado GEORGE RADANOVICH, California Vice Chairman JOSEPH R. PITTS, Pennsylvania LOIS CAPPS, California MARY BONO MACK, California MICHAEL F. DOYLE, Pennsylvania GREG WALDEN, Oregon JANE HARMAN, California LEE TERRY, Nebraska TOM ALLEN, Maine MIKE ROGERS, Michigan JANICE D. SCHAKOWSKY, Illinois SUE WILKINS MYRICK, North Carolina HILDA L. -

Edit Master Title Style DATA CENTER
DATAClick CENTER to edit Master title style DATA CENTER Make sense of your data David Brock, Founder and Director Data Center Massachusetts Institute of Technology SOLUTION XML PROBLEM <CallsPerDay> 2575 </CallsPerDay> PROBLEM “CallsPerDay” ? That’s not even a word ANOTHER PROBLEM <CompanyData> <CompanyName> Fidelity Employer Services Company </CompanyName> <Location> Merrimack </location> <CallData> <RecordDate> Tue Aug 11, 2004 </RecordDate> <CallsPerDay> 2575 </CallsPerDay> </CallData> </CompanyData> MORE PROBLEMS <CompanyData> <CompanyName> <CorporateRecords> Fidelity Employer <Company> Services Company Fidelity Employer </CompanyName> Services Company <Location> </Company> Merrimack <Records Data= “Tue Aug </location> ? 11, 2004” > <CallData> <Calls Units=“PerDay”> <RecordDate> 2575 Tue Aug 11, 2004 </Calls> </RecordDate> </CorporateRecords> <CallsPerDay> 2575 </CallsPerDay> </CallData> </CompanyData> OBSERVATION <CompanyData> “CallsPerDay” <CompanyName> Fidelity Services </CompanyName> <Location> vocabulary Merrimack </location> <CallData> grammar <RecordDate> Tue Aug 11,2005 </RecordDate> <CallsPerDay> 2575 </CallsPerDay> </CallData> </CompanyData> STANDARDS? 4ML ARMLARML BiblioML CIDX eBIS-XML HTTP-DRP MatML ODRL PrintTalk SHOE UML XML F AML ARMLARML BCXML xCIL ECML HumanML MathML OeBPS ProductionML SIF UBL XML Key AML ASMLASML BEEP CLT eCo HyTime MBAM OFX PSL SMML UCLP XMLife AML ASMLASML BGML CNRP EcoKnow IML MISML OIL PSI SMBXML UDDI XML MP AML ASTMASTM BHTML ComicsML edaXML ICML MCF OIM QML SMDL UDEF XML News AML ATMLATML -

Data Analytics Subgroup Report
Data Analytics Subgroup report Paolo Alcini - EMA (subgroup lead) Gianmario Candore – EMA (subgroup lead) Marek Lehmann - EMA Luis Pinheiro - EMA Antti Hyvärinen - Fimea Hans Ovelgonne – CBG-MED Mateja Sajovic - JAZMP Panagiotis Telonis - EMA Kevin Horan – HPRA (until May 2018) Massimiliano Falcinelli – EMA (from September 2018) See websites for contact details Heads of Medicines Agencies www.hma.eu European Medicines Agency www.ema.europa.eu An agency of the European Union Table of content Executive summary ..................................................................................................... 7 Data Standardisation ................................................................................................ 7 Information technology ............................................................................................ 8 Data manipulation ................................................................................................... 9 Artificial intelligence ................................................................................................. 9 Conclusions ........................................................................................................... 10 Acknowledgments .................................................................................................. 11 Data Analytics – Standardisation................................................................................. 12 1. Standardisation....................................................................................................