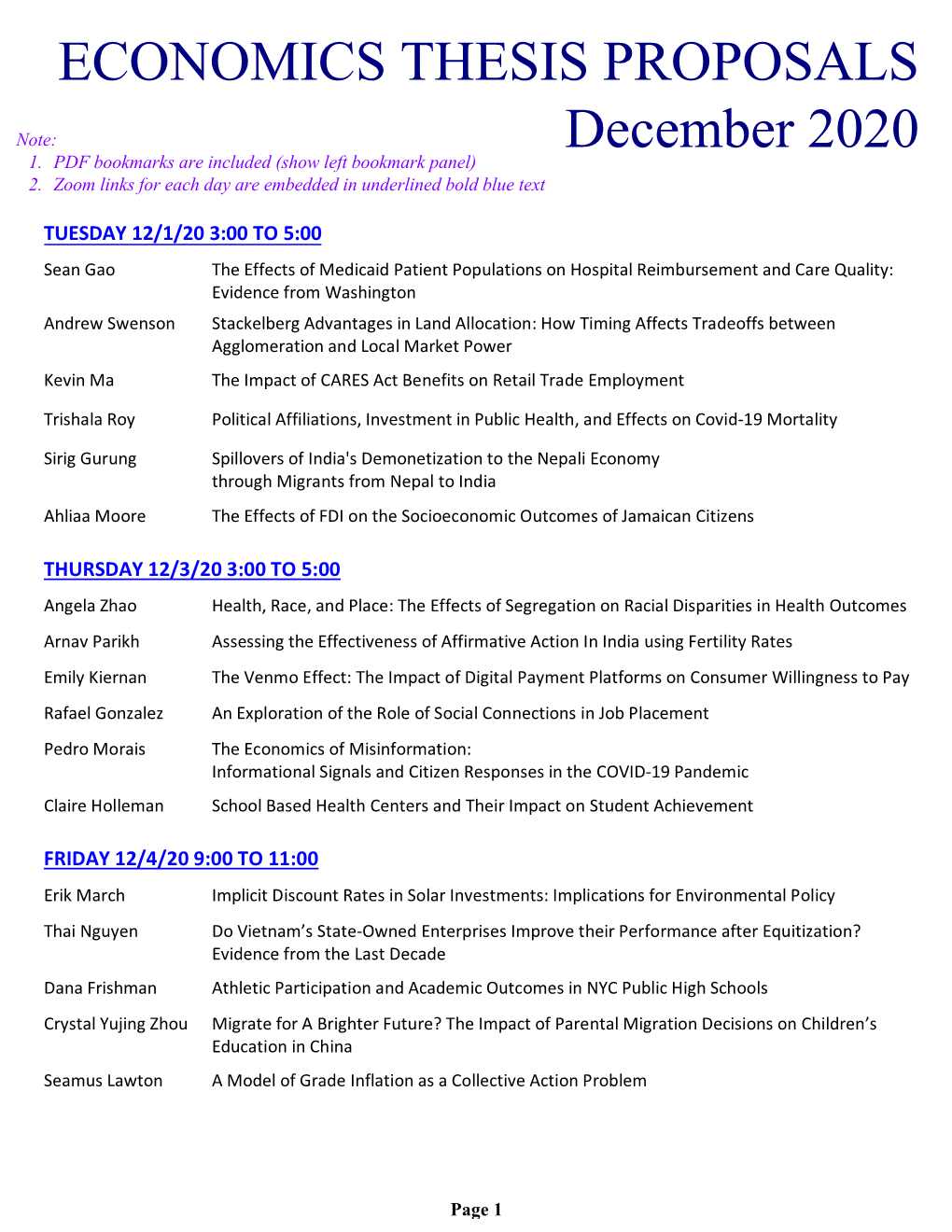
Economics Thesis Proposals December 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

National Letter in Support of Federal All-Payer Claims Database
National Letter in Support of Federal All-Payer Claims Database As health scholars, leaders of health organizations, and funders of health research, we are writing in support of establishing a federal all-payer claims database (APCD). APCDs regularly collect data on health insurance claims from all of the payers in a given area (typically a state). Because they include demographic and diagnostic data on patients as well as any treatment or drug paid for by insurance (private or public), APCDs can be immensely valuable for research. APCDs have been used by health scholars to study numerous issues about quality and cost, including the extent of long-term opioid use after surgery, the ability of Medicaid patients to access physicians, the amount of wasted medical spending ending on low-value care, the performance of new models to reduce health spending (such as patient-centered medical home programs), the rate of complications after routine surgeries, and the characteristics of the highest-cost Medicaid patients. In 2016, however, the Supreme Court rendered it all but impossible for states to establish comprehensive APCDs, on the grounds that the Employee Retirement Income Security Act (ERISA) preempted states from requiring reporting by self-insured health plans. As noted in the Journal of the American Medical Association, this Supreme Court decision has “far-reaching implications for the ability of states to access comprehensive health information to inform policy making.” In May 2019, the Senate Health, Education, Labor and Pensions Committee released a draft of the Lower Health Care Costs Act. Among other things, that Act would amend ERISA to create a federal APCD whose data would be available to “researchers and policymakers.” While we are not all able to take a position on specific federal legislation, we can all agree that a national APCD would be an enormous leap forward for the ability of health researchers to study the cost and quality of medical care across the U.S. -

Reporter NATIONAL BUREAU of ECONOMIC RESEARCH
NBER Reporter NATIONAL BUREAU OF ECONOMIC RESEARCH A quarterly summary of NBER research No. 4, December 2017 Program Report ALSO IN THIS ISSUE Employment Changes for Cognitive Occupations, 2000–2012 Industrial Organization Percentage change in STEM and other managerial or professional occupations -20 0 20 40 60 * Teachers (K-12) Liran Einav and Jonathan Levin Managers (All) Nurses Health Technicians Health Therapists Comp. Sci./Programming/Tech. Support Accounting And Finance Economists & Survey Researchers Social Workers, Counselors & Clergy Physicians College Instructors Researchers in the Program on Industrial Organization (IO) study Lawyers and Judges Other Business Support consumer and firm behavior, competition, innovation, and govern- Operations Researchers Physicians' Assistants Medical Scientists ment regulation. This report begins with a brief summary of general Legal Assistants and Paralegals Pharmacists developments in the last three decades in the range and focus of pro- Dental Hygienists Mathematicians/Statisticians/Actuaries gram members’ research, then discusses specific examples of recent Dentists Social Scientists And Urban Planners Artists, Entertainers, and Athletes work. Marketing, Advertising and PR Pilots/Air Traic Control When the program was launched in the early 1990s, two devel- Biological Scientists Physical Scientists Architects opments had profoundly shaped IO research. One was development Writers, Editors, and Reporters Engineering And Science Technicians of game-theoretic models of strategic behavior by firms with market Draers And Surveyors 1 Engineers (All) power, summarized in Jean Tirole’s classic textbook. The initial wave -20 0 20 40 60 of research in this vein was focused on applying new insights from eco- Source: D. Deming, NBER Working Paper No. 21473 nomic theory; empirical applications came later. -

We, the Undersigned Economists, Represent a Broad Variety of Areas of Expertise and Are United in Our Opposition to Donald Trump
We, the undersigned economists, represent a broad variety of areas of expertise and are united in our opposition to Donald Trump. We recommend that voters choose a different candidate on the following grounds: . He degrades trust in vital public institutions that collect and disseminate information about the economy, such as the Bureau of Labor Statistics, by spreading disinformation about the integrity of their work. He has misled voters in states like Ohio and Michigan by asserting that the renegotiation of NAFTA or the imposition of tariffs on China would substantially increase employment in manufacturing. In fact, manufacturing’s share of employment has been declining since the 1970s and is mostly related to automation, not trade. He claims to champion former manufacturing workers, but has no plan to assist their transition to well-compensated service sector positions. Instead, he has diverted the policy discussion to options that ignore both the reality of technological progress and the benefits of international trade. He has misled the public by asserting that U.S. manufacturing has declined. The location and product composition of manufacturing has changed, but the level of output has more than doubled in the U.S. since the 1980s. He has falsely suggested that trade is zero-sum and that the “toughness” of negotiators primarily drives trade deficits. He has misled the public with false statements about trade agreements eroding national income and wealth. Although the gains have not been equally distributed—and this is an important discussion in itself—both mean income and mean wealth have risen substantially in the U.S. -

INAUGURAL CARIBBEAN HEALTH ECONOMICS SYMPOSIUM Bitter
INAUGURAL CARIBBEAN HEALTH ECONOMICS SYMPOSIUM Bitter End Yacht Club Virgin Gorda, British Virgin Islands Agenda – As of December 8, 2015 Sunday, December 13, 2015 Pre-Symposium Necker Island Tour Tour of Richard Branson’s personal island and nature park: 1:00pm to 3:30pm Personal invite from the Richard with opportunity to meet him personally at end of tour. Space is limited. Will leave from BEYC dock on symposia boats or motor launch to Necker Island. Welcome reception, 6:00pm, BEYC Town & Gown Exchange, 7:00pm, BEYC “Publications, Patents and Privacy: Holy Trinity or Bermuda Triangle of Health Economics Research”: Informal forum between policy makers, academics and industry Monday, December 14, 2014 Breakfast at BEYC 7:00 to 8:30 Paper - 8:30 to 9:30: Switching Costs and Plan Loyalty in Medicare Part C. Adam Atherly, University of Colorado, Denver Roger Feldman, University of Minnesota Bryan Dowd, University of Minnesota E. Van den Broek, University of Colorado, Denver Paper - 9:30 to 10:30: Insurer Competition in Health Care Markets Kate Ho, Columbia University Robin S. Lee, Harvard University Coffee and electronic catch-up 10:30 to 11:00 Paper - 11:00 to Noon: Marginal Treatment Effects and the External Validity of the Oregon Health Insurance Experiment Amanda Kowalski, Yale University Afternoon choices and preferences o Afternoon Activities arranged independently by BEYC staff - OR - o Sail excursion to The Baths on Virgin Gorda (with a possible race back) Happy Hour Town & Gown Exchange, 7:00pm, BEYC Has pharmacoeconomics lost its way? Panel discussion featuring work from Andrew Briggs (Glasgow, UK), Adrian Levy (Dalhousie, Canada) and David Henry (Toronto, Canada) paper. -

Download This
25th Annual Health Economics Conference (A H E C) Thursday ± F riday, October 16-17, 2014 Dore Commons, Baker Institute for Public Policy Agenda General Presentation Timeline: Sessions will last approximately 50 minutes. Speakers will present for 35 minutes, followed by 10 minutes of questions from the discussant and 5 minutes for general questions. Thursday, October 16, 2014 Session 1: Medicare Reform Moderator: Vivian Ho 5LFH8QLYHUVLW\¶V%DNHU,QVWLWXWH 8:15 a.m. BREAKFAST 9:15 a.m. Welcome & Introduction 9LYLDQ+R 5LFH8QLYHUVLW\¶V%DNHUInstitute) 9:30 a.m. ³Does Privatized Health Insurance Benefit Patients or Producers? Evidence from Medicare Advantage´ Authors: Marika Cabral (University of Texas at Austin, presenting), Michael Geruso (University of Texas at Austin), and Neale Mahoney (University of Chicago) Discussant: Jason Abaluck (Yale University) 10:20 a.m. ´7KH,PSDFWRI&RQVXPHU,QDWWHQWLRQRQ,QVXUHU3ULFLng in the Medicare Part D 3URJUDP´ Authors: Kate Ho (Columbia University, presenting), Joseph Hogan (Columbia University), and Fiona Scott Morton (Yale University) Discussant: John Romley (University of Southern California) Paper not available online. 11:10 a.m. BREAK 11:30 a.m. ³Upcoding or Selection? Evidence from Medicare on Squishy Risk Adjustment´ Authors: Michael Geruso (Harvard University, University of Texas at Austin) and Timothy Layton (Harvard Medical School, presenting) Discussant: Colleen Carey (University of Michigan) 12:20 p.m. LUNCH Session 2: Improving Health Outcomes Moderator: Aimee Chin (University of Houston) 1:30 -

NBER WORKING PAPER SERIES DO INCREASING MARKUPS MATTER? LESSONS from EMPIRICAL INDUSTRIAL ORGANIZATION Steven T. Berry Martin Ga
NBER WORKING PAPER SERIES DO INCREASING MARKUPS MATTER? LESSONS FROM EMPIRICAL INDUSTRIAL ORGANIZATION Steven T. Berry Martin Gaynor Fiona Scott Morton Working Paper 26007 http://www.nber.org/papers/w26007 NATIONAL BUREAU OF ECONOMIC RESEARCH 1050 Massachusetts Avenue Cambridge, MA 02138 June 2019 We wish to thank Al Klevorick and editors at the Journal of Economics Perspectives—Enrico Moretti, Gordon Hanson, and managing editor Tim Taylor—for helpful comments and suggestions that substantially improved the paper. The usual caveat applies. The views expressed herein are those of the authors and do not necessarily reflect the views of the National Bureau of Economic Research. At least one co-author has disclosed a financial relationship of potential relevance for this research. Further information is available online at http://www.nber.org/papers/w26007.ack NBER working papers are circulated for discussion and comment purposes. They have not been peer-reviewed or been subject to the review by the NBER Board of Directors that accompanies official NBER publications. © 2019 by Steven T. Berry, Martin Gaynor, and Fiona Scott Morton. All rights reserved. Short sections of text, not to exceed two paragraphs, may be quoted without explicit permission provided that full credit, including © notice, is given to the source. Do Increasing Markups Matter? Lessons from Empirical Industrial Organization Steven T. Berry, Martin Gaynor, and Fiona Scott Morton NBER Working Paper No. 26007 June 2019 JEL No. L0,L1,L4 ABSTRACT This paper considers the recent literature on firm markups in light of both new and classic work in the field of Industrial Organization. We detail the shortcomings of papers that rely on discredited approaches from the “structure-conduct-performance” literature. -

Leemore S. Dafny
LEEMORE S. DAFNY www.kellogg.northwestern.edu/faculty/dafny/personal Department of Management and Strategy [email protected] Kellogg School of Management, Northwestern University (847) 467-7511 (phone) 2001 Sheridan Road, Evanston, Illinois 60208-2001 (847) 467-1777 (fax) EMPLOYMENT AND APPOINTMENTS NORTHWESTERN UNIVERSITY, KELLOGG SCHOOL OF MANAGEMENT Evanston, IL 2012- present Herman Smith Research Professor in Hospital and Health Services, Department of Management and Strategy 2010- present Associate Professor with tenure, Department of Management and Strategy 2002 - 2009 Assistant Professor, Department of Management and Strategy 2003- present Faculty Research Fellow/Associate, Institute for Policy Research NATIONAL BUREAU OF ECONOMIC RESEARCH Cambridge, MA 2010-present Faculty Research Associate, NBER Programs on Aging and Health Care 2002 - 2009 Faculty Research Fellow, NBER Programs on Aging and Health Care 2001 - 2002 Post-Doctoral Fellow in Health and Aging Economics 1999 - 2000 Pre-Doctoral Fellow in Health and Aging Economics MCKINSEY AND COMPANY Washington, DC 1995 - 1997 Business Analyst. EDUCATION 1997 - 2001 MASSACHUSETTS INSTITUTE OF TECHNOLOGY Cambridge, MA Ph.D. in Economics. Dissertation entitled “The Impact of Market Forces and Public Health Insurance on Inpatient Care.” 1991 - 1995 HARVARD UNIVERSITY Cambridge, MA A.B. in Economics, summa cum laude. HONORS, FELLOWSHIPS, GRANTS 2011 Sidney J. Levy Teaching Award 2010, 2011 Faculty Impact Award for excellence in teaching 2007 - 2008 Searle Center on Law, -

Health Economics Jonathan Gruber, MIT
AEA Continuing Education Program Health Economics Jonathan Gruber, MIT January 5-7, 2015 Health Care in the U.S.: The Demand Side Jonathan Gruber AEA Continuing Education Insurance Coverage in the U.S. - Background Why is Most Private Insurance from Employers? • Risk pooling and Economies of Scale • 99% of firms > 200 employees offer • 48% of firms <10 employees offer • Tax-subsidy to employer-provided insurance • $250 billion in foregone income/payroll tax • Subsidy to employees, not employers • (Pre-ACA) Failure in non-group insurance market • Pre-existing conditions exclusions & rejection • Hendren: Can be optimal if private info correlated with costs • Risk rating • Experience rating • No dynamic insurance Medicare • Insurance for post 65 (85%) and disabled (15%) • Payroll tax of 1.45% each on employer/employee (uncapped) • Ten year work requirement • Part A: Hospital & LTC • Financed by payroll tax • Deductible for first 60 days & more thereafter • Part B: Docs & outpatient • Voluntary – 25% of costs enrollee premium, rest from general revenues • Small deductible but uncapped coinsurance • Part D: Drugs (since 2006) • Variety of plan designs & premiums – about 75% general revenues Medicaid • Really two programs, administered by state • Variation in eligibility (lots), provider reimbursement (lots), benefits (little) • First is for low income families • Very low income families • Pregnant women & kids up to 200% FPL or higher • (if state expands Medicaid) all up to 138% FPL • Free, comprehensive insurance • Second is for low income -

Labor Market Monopsony: Trends, Consequences, and Policy Responses
COUNCIL OF ECONOMIC ADVISERS ISSUE BRIEF OCTOBER 2016 LABOR MARKET MONOPSONY: TRENDS, CONSEQUENCES, AND POLICY RESPONSES Introduction Figure 1: Labor Share of Income, Nonfarm Business Sector, 1948-2016 Percent In September, the U.S. Census Bureau reported that 68 in 2015, the typical household saw its income grow 66 by $2,800, or 5.2 percent, the fastest rate on record. 64 Over the course of this business cycle, average annual wage growth has been higher than any 62 business cycle since the early 1970s. This is real 60 2016:Q2 progress toward higher incomes for working 58 Americans—a central goal of many of the policy initiatives the Obama Administration has undertaken 56 since 2009. 54 1948 1958 1968 1978 1988 1998 2008 Note: Shading denotes recession. But while these gains are a step in the right direction, Source: Bureau of Labor Statistics, Productivity and Costs more work remains to fully address long-term challenges of slow wage growth and rising inequality. At the same time, labor income itself has become Over the past several decades, only the highest increasingly unequally divided. Researchers have earners have seen steady wage gains; for most focused on the divergence between worker skills and workers, wage growth has been sluggish and has employer needs—a challenge brought about by failed to keep pace with gains in productivity (CEA technological change and a trend in educational 2015, Ch. 3). Though the slowdown in wage growth investments that, while rising, has not kept pace with is partly due to a slowdown in productivity growth demand, which has risen even faster (Autor 2014; since the 1970s, the share of income accruing to Katz and Murphy 1992; Goldin and Katz 2007). -

The Effect of Fees for Musical Performance Rights on the Commerci
Dynamic Product Positioning in Di¤erentiated Product Markets: The E¤ect of Fees for Musical Performance Rights on the Commercial Radio Industry Andrew Sweeting Duke University and NBER July 2012 Abstract This article predicts how radio station formats would change if, as was recently proposed, music stations were made to pay fees for musical performance rights. It does so by estimating and solving, using parametric approximations to …rms’value functions, a dynamic model which captures important features of the industry such as vertical and horizontal product di¤erentia- tion, demographic variation in programming tastes and multi-station ownership. The estimated model predicts that high fees would cause the number of music stations to fall signi…cantly and quite quickly. For example, a fee equal to 10% of revenues would cause a 4.6% drop in the 1 number of music stations within 2 2 years, and a 9.4% drop in the long-run. The size of the change is limited, however, by the fact that many listeners, particularly in demographics that are valued by advertisers, have strong preferences for music programming. Please send comments to [email protected]. I would like to thank Jerry Hausman, Igal Hendel, Aviv Nevo, Amil Petrin, Ariel Pakes, Rob Porter, Steve Berry, Pat Bayer, Peter Arcidiacono, Kate Ho, Allan Collard-Wexler, Paul Ellickson, Arie Beresteanu, three referees and seminar participants for valuable comments. I would like to thank the National Association of Broadcasters and the Center for the Study of Industrial Organization at Northwestern University for …nancial support. All errors are my own. 1 1 Introduction This article develops and estimates a dynamic oligopoly model to predict the e¤ect on product variety of legislation (the Performance Rights Act1), introduced into Congress in 2009 with the support of the Obama Administration and members of both parties, requiring music radio stations to pay fees for musical performance rights. -

Moral Hazard in Health Insurance: Do Dynamic Incentives Matter?
Moral Hazard in Health Insurance: Do Dynamic Incentives Matter? The MIT Faculty has made this article openly available. Please share how this access benefits you. Your story matters. Citation Aron-Dine, Aviva, Liran Einav, Amy Finkelstein, and Mark Cullen. “Moral Hazard in Health Insurance: Do Dynamic Incentives Matter?” Review of Economics and Statistics 97, no. 4 (October 2015): 725– 741. As Published http://dx.doi.org/10.1162/REST_a_00518 Publisher MIT Press Version Final published version Citable link http://hdl.handle.net/1721.1/110640 Terms of Use Article is made available in accordance with the publisher's policy and may be subject to US copyright law. Please refer to the publisher's site for terms of use. MORAL HAZARD IN HEALTH INSURANCE: DO DYNAMIC INCENTIVES MATTER? Aviva Aron-Dine, Liran Einav, Amy Finkelstein, and Mark Cullen* Abstract—Using data from employer-provided health insurance and Medi- One aspect of this literature that we find remarkable is the care Part D, we investigate whether health care utilization responds to the dynamic incentives created by the nonlinear nature of health insurance con- near consensus on the nature of the endeavor: the attempt to tracts. We exploit the fact that because annual coverage usually resets every quantify the response of medical spending with respect to its January, individuals who join a plan later in the year face the same initial (out-of-pocket) price to the consumer. For example, in their (“spot”) price of health care but a higher expected end-of-year (“future”) price. We find a statistically significant response of initial utilization to the chapter on health insurance in Handbook of Health Econom- future price, rejecting the null that individuals respond only to the spot price. -

Is There a VA Advantage? Evidence from Dually Eligible Veterans
Is There a VA Advantage? Evidence from Dually Eligible Veterans David C. Chan David Card Lowell Taylor* March 2021 Abstract Societies face a difficult choice between private and public provision of health care, and there is a shortage of credible evidence to guide this choice. The structure of health care delivery to US veterans provides a distinctive research setting to study this issue. Specifically, veterans aged 65 and older are dually eligible for care in private hospitals (financed by Medicare) or in public- sector hospitals operated by the US Department of Veterans Affairs (VA) in the nation’s largest integrated health care delivery system. We utilize the ambulance design of Doyle et al. (2015) to examine the effect of VA vs. non-VA emergency care on mortality in this high-risk population. We find a VA advantage: a 28-day mortality reduction of 46% (4.5 percentage points, with a 95% confidence interval of 1.1 to 8.0). Survival gains persist for at least a year after the initial ambulance ride, and they accrue despite lower spending in the VA. Evidence suggests that the VA advantage arises in part from some combination of continuity of care and health IT. These results have policy relevance—as the federal government is deciding whether to maintain the existing VA system or to expand financing of private care outside of the VA—and they shed light on sources of inefficiency in private-sector health care in the US. JEL Codes: I10, I18 Keywords: VA, Medicare, mortality, dual eligibility *Chan: Stanford University, Department of Veterans Affairs, and NBER, [email protected]; Card: UC Berke- ley and NBER, [email protected]; Taylor: Carnegie Mellon University and NBER, [email protected].