2012 – 13 District Health Society, Nalanda
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ground Water Year Book, Bihar (2015 - 2016)
का셍ााल셍 उप셍ोग हेतू For Official Use GOVT. OF INDIA जल ल MINISTRY OF WATER RESOURCES CENTRAL GROUND WATER BOARD जल ,, (2015-2016) GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) म鵍य पूर्वी क्षेत्र, पटना सितंबर 2016 MID-EASTERN REGION, PATNA September 2016 ` GOVT. OF INDIA जल ल MINISTRY OF WATER RESOURCES जल CENTRAL GROUND WATER BOARD ,, (2015-2016) GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) म鵍य पर्वू ी क्षेत्र, पटना MID-EASTERN REGION, PATNA सितंबर 2016 September 2016 GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) CONTENTS CONTENTS Page No. List of Tables i List of Figures ii List of Annexures ii List of Contributors iii Abstract iv 1. INTRODUCTION.............................................................................................................1 2. HYDROGEOLOGY..........................................................................................................1 3. GROUND WATER SCENARIO......................................................................................4 3.1 DEPTH TO WATER LEVEL........................................................................................8 3.1.1 MAY 2015.....................................................................................................................8 3.1.2 AUGUST 2015..............................................................................................................10 3.1.3 NOVEMBER 2015........................................................................................................12 3.1.4 JANUARY 2016...........................................................................................................14 -

Afu Srd Qoffir
qeio-ftocogofroelo/ lRMs- 10/2020, qi"...1.?.... fe-ax tcnffft-o gan frvn ffi (qrqrq s$rsq frqrrr) nso', sfi{r ts{ fu€r. frts o,d c-{ffi. ftErq crrfifto gun frvr ffi qe-+t ftr n, ftrm q-flDorfr. qfiIt qr.n. ftci--...a >ll.g.l.l..t:^ ftqq:- qrc-q ssrEFr c-{'Er{ c"nd (HRMS) clMn t-{r gkorot ovn rgqtqun-sqa iD't Scanning d tidq { t q{frl:- fr{H qr qiw-''titz. fr{ifr-1s.io.2o1s aefl q{i6-gol. fr{is- 29.05.2020 IT6ITq, sqEffi frqq-o' crciFro q'it d snr enc si-{q-d t fu rrq ofid oI \1otq-d srcrn{ d-fi oa qFit qa or eR-o G crrflff $ffiq-qf, qr+q \4qErt !-qtrr cqrfr (HRMs) ffi( o-{i d mq d fu S*Zo* qms q'r Digitisation aeTI e-tar gw ot ffiu fu sqcIcr qtrqr"qt (legacy oata) fr Data capture Format (DCFIi cfre o'-{i or ord srt i t 2. -cniFro' c=jl n +sI gRilor. ridl= 3IRs st 6ffi{it ErqI sqnrq orri rrc Efrqw q, ol Scanning 6{i d €dtl I arerrl i] oTd-6q +1 qaw frn qri ot s-de fu-ql .rqr t t q-c-{ o. tfl Sfu"ol r{ €dcun qr d scanning t-E ftrd d orufa-q-qR aTtroq frt q.ff *ia.{ tr (3r-flff-r) 4- Scanning 61 o,rd qqF-( 1'Ss lvs CBSL eRI ffiqr .rfi. f,a, 3Tq{ qfoq. .rfi Fmfur fuTFr d ory S qmi srd o.rt it ftcio-oa.o'r.zoz'r d qrtqt"-gef ro:oo ad t 3rq{rfl 6:00 cd ao ria.c o'd-6'q F-5{ff-r) o r5wn fu-qI qrvqrt 5. -

41629-013: Bihar State Highways II Project
Social Monitoring Report Project Number: 41629-013 / 44425-013 September 2019 Period: January 2018 – June 2018 IND: Bihar State Highway II Project SH – 78 Submitted by Bihar State Road Development Corporation Limited, Patna This social monitoring report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. Bihar State Highway Project Phase – II CONTRACT PACKAGE NO.1& 2 (SH-78) (Bihta – Sarmera) Monitoring and Implementation of Resettlement Plan (RP) Semi Annual Report January 2018 - June 2018 Submitted By Egis International S.A in JV with Egis India Consulting Engineers Pvt. Ltd. Plot No.66, Sec.32 Gurgaon-122001 CONTENTS Abbreviation ................................................................................................................................................... 2 GLOSSARY ...................................................................................................................................................... 3 1. PROJECT BACKGROUND ........................................................................................................................... 4 2. PROJECT DESCRIPTION .......................................................................................................................... -

State District Name of Bank Bank Branch/ Financial Literacy Centre
State District Name of Bank Branch/ Address ITI Code ITI Name ITI Address State District Phone Email Bank Financial Category Number Literacy Centre Bihar Araria State Araria Lead Bank Office, PR10000055 Al-Sahaba Industrial P Alamtala Forbesganj Bihar Araria NULL Bank of ADB Building, Training Institute India Araria, Pin- 854311 Bihar Arwal PNB ARWAL ARWAL PR10000083 Adarsh ITC P Umerabad Bihar Arwal NULL Bihar Arwal PNB ARWAL ARWAL PR10000284 Shakuntalam ITC P Prasadi English Bihar Arwal NULL Bihar Arwal PNB ARWAL ARWAL PR10000346 Aditya ITC P At. Wasilpur, Main Road, Bihar Arwal NULL P.O. Arwal, Bihar Arwal PNB ARWAL ARWAL PR10000396 Vikramshila Private P At. Rojapar, P.O. Arwal Bihar Arwal NULL ITI Bihar Arwal PNB ARWAL ARWAL PR10000652 Ram Bhaman Singh P At-Purani Bazar P.o+P.S- Bihar Arwal NULL Private ITI Arwal Bihar Arwal PNB ARWAL ARWAL PR10000677 Sukhdeo Institute Of P Kurtha, Arwal Bihar Arwal NULL Tecnology Private ITI, Bihar Arwal PNB ARWAL ARWAL PR10000707 Dr. Rajendra Prasad P Mubarkpur, Kurtha Arwal Bihar Arwal NULL Private ITI, Bihar Aurangabad PUNJAB DAUDNAGAR DAUDNAGAR PR10000027 New Sai Private ITI- P Aurangabad Road, Bihar Aurangabad NULL NATIONA Bhakharuan More, , Tehsil- L BANK Daudnagar , , Aurangabad - 824113 Bihar Aurangabad PUNJAB AURANGABAD AURANGABAD PR10000064 Adharsh Industrial P Josai More Udyog Bihar Aurangabad NULL NATIONA Training Centre Pradhikar Campus L BANK Bihar Aurangabad MADHYA DAUDNAGAR DAUDNAGAR PR10000108 Sardar Vallabh Bhai P Daudnagar Bihar Aurangabad NULL BIHAR Patel ITC, Daudnagar GRAMIN BANK Bihar Aurangabad MADHYA DAUDNAGAR DAUDNAGAR PR10000142 Adarsh ITC, P AT-,Growth centre ,Jasoia Bihar Aurangabad NULL BIHAR Daudnagar More Daudnagar GRAMIN BANK Bihar Aurangabad PUNJAB RATANUA RATANUA PR10000196 Progresive ITC P At-Growth Center Josia Bihar Aurangabad NULL NATIONA More L BANK Bihar Aurangabad MADHYA DAUDNAGAR DAUDNAGAR PR10000199 Arya Bhatt ITC P Patel Nagar, Daud Nagar Bihar Aurangabad NULL BIHAR GRAMIN BANK Bihar Aurangabad PUNJAB OLD GT RD. -

Unclaimed & Unpaid Dividend For
First Name Middle name Last Name Address Country State Dist. Pin code Folio No. Investment type Amount Due (in Rs.) Proposed Date of Transfer to IEPF RAVINDER NATH SHARMA 3382 DELHI GATE DELHI 110002 INDIA DELHI CENTRAL DELHI 110002 0000157 Amount for unclaimed and 300.00 23-OCT-2016 unpaid dividend HARISH KUMAR BISHT C/O NATIONAL INS. COM. LTD. EMCA HOUSE D.O.XX INDIA DELHI CENTRAL DELHI 110002 0008581 Amount for unclaimed and 30.00 23-OCT-2016 23/23B, ANSARI ROAD, DARYA GANJ DELHI 110002 unpaid dividend RAJINDER KUMAR SHARMA 1/2892 RAM NAGAR LONI ROAD SHAHDRA DELHI INDIA DELHI EAST DELHI 110032 0008669 Amount for unclaimed and 30.00 23-OCT-2016 110032 unpaid dividend SURESH KUMAR SHARMA 1/2892 RAM NAGAR LONI ROAD SHAHDRA DELHI INDIA DELHI EAST DELHI 110032 0008670 Amount for unclaimed and 30.00 23-OCT-2016 110032 unpaid dividend RAJESH SHARMA 1/2892 RAM NAGAR LONI ROAD SHAHDRA DELHI INDIA DELHI EAST DELHI 110032 0008671 Amount for unclaimed and 30.00 23-OCT-2016 110032 unpaid dividend PUSHPA GUPTA GP 13 MAURYA ENCLAVE PITAMPURA DELHI 110034 INDIA DELHI CENTRAL DELHI 110034 0001466 Amount for unclaimed and 30.00 23-OCT-2016 unpaid dividend PUSHPA JAIN 147 RISHAB VIHAR VIKAS MARG EXTENTION DELHI INDIA DELHI EAST DELHI 110092 0002395 Amount for unclaimed and 60.00 23-OCT-2016 DELHI 110092 unpaid dividend AMAN SHARMA H NO 7/607 ANIL NAGAR MAHAVIR COLONY INDIA HARYANA KARNAL 131001 0002953 Amount for unclaimed and 30.00 23-OCT-2016 SONEPAT HARYANA HARYANA 131001 unpaid dividend KOMAL JAIN HOUSE NO. -

Bhojpur District, Bihar State
भूजल सूचना पुस्तिका भोजपुर स्जला, बिहार Ground Water Information Booklet Bhojpur District, Bihar State 84° 15' 84° 30' 84° 45' BIHAR STATE ADMINISTRATIVE MAP N BHOJPUR DISTRICT, BIHAR. Ganga R. 25° 25° 45' 45' GANGA RIVER Barhara Gaura Bhagar N. Dehra N. Shahpur Gangi N. Koilwar Chher N. Bihiya ARA 25° Udawant 25° nagar 30' Gangi N. 30' Jagdishpur Garhani KumhariSandes N. Charpokhari Agiaon Banas N. Piro 25° Sahar 25° 15' SON RIVER 15' LEGEND Tarari District Boundary Block Boundary River District HQ. 0 5 10 15 20 Km Block HQ. Road Scale Railway 84° 15' 84° 30' 84° 45' के न्द्रीय भमू िजल िो셍 ड Central Ground water Board Ministry of Water Resources जल संसाधन िंत्रालय (Govt. of India) (भारि सरकार) Mid-Eastern Region िध्य-पर्वू ी क्षेत्र Patna पटना मसिंिर 2013 September 2013 1 PREPARED BY - Shri S. Sahu Sc. B UNDER SUPERVISION OF - Shri A.K.Agrawal, Scientist’D’ CARTOGRAPHY - Shri Lokendra Kumar, D/Man Gd-II 2 UPDATED BY - Shri S.N.Dwivedi, Sc- C & Dr. Fakhre Alam, STA (Hg) CONTENTS DISTRICT AT A GLANCE. 5-6 1. INTRODUCTION 7 - 10 1.1 Location, Area and Administrative Details 1.2 Basin/Sub-Basin and Drainage 1.3 Landuse, Agriculture and Irrigation Practices 1.4 Studies/Activities carried by CGWB 2. CLIMATE AND RAINFALL 10 3. GEOMORPHOLOGY AND SOIL 10-11 3.1 Geomorphology 3.2 Soil 4. GROUND WATER SCENARIO 11 - 17 4.1 Water Bearing Formations 4.2 Occurrence & Movement of Ground Water 4.3 Depth to Water Level 4.4 Ground Water Quality 4.4.1 Arsenic in Ground Water 4.5 Ground Water Resources 5. -

BIHARSHARIF.Pdf
IINNDDIIAANN MMEEDDIICCAALL AASSSSOOCCIIAATTIIOONN::: BBIIHHAARR SSTTAATTEE BBRRAANNCCHH LLIIISSTT OOFF LLIIIFFEE MMEEMMBBEERRSS OOFF III... MM... AA... (((BBIIIHHAARRSSHHAARRIIIFF BBRRAANNCCHH))) BBIIHHAARRSSHHAARRIIFF BBRRAANNCCHH 1. Dr. Om Prakash Prasad 10. Dr. Ram Kripal Singh BHR/7051/12/126/149466/2009-10/L BHR/1005/12/10/17466/90-91/L C/o Dr. Siya Sharan Prasad Ranchi Road Bhraopar, P.O. – Biharsharif P. O. Biharsharif-803 101 Dist. Nalanda (Bihar) Dist. Nalanda (Bihar) 2. Dr. Sanjay Kumar 11. Dr. Dinesh Prasad Singh BHR/4004/12/200/71549/99-2000/L BHR/1006/12/11/17367/90-91/L C/o Dr. Sita Ram Singh Dhaneshwar Ghat North West Masjid, Mogalkuan Near Congress Office P.O- Sohsarai – 803 118 P. O. Biharsharif-803 101 Dist. Nalanda (Bihar) Dist. Nalanda (Bihar) 3. Dr. Kamta Prasad 12. Dr. Arvind Kumar Sinha BHR/13/12/3/155/L 13. Dr. (Mrs.) Suniti Sinha At & P. O. Biharsharif-803 101 BHR/1007/12/12/17368/90-91/CL Dist. Nalanda (Bihar) Nalanda Netralaya, Garhpar P. O. Biharsharif-803 101 Dist. Nalanda (Bihar) 4. Dr. Rajesh Kumar 14. Dr. Umesh Kumar Sinha BHR/6884/12/118/144479/2009-10/L 15. Dr. (Mrs.) Nirmala Sinha Main Road, Patel Nagar BHR/1008/12/13/17369/90-91/CL At & P.O. Hilsa – 801 302. Professor Colony, Dhaneshwar Ghat Dist. Nalanda (Bihar) P. O. Biharsharif-803 101 Dist. Nalanda (Bihar) 5. Dr. Awadhesh Kumar Sinha 16. Dr. Bankey Bihari Sinha BHR/1154/12/201/17515/90-91/L BHR/1009/12/14/17370/90-91/L Doctors Colony, Khandakpar Bhainsasur P. O. – Biharsharif-803 101 P. -
Saran Introduction
DISTRICT PROFILE SARAN INTRODUCTION Saran district is one of the thirty-eight districts of Bihar. Saran district is a part of Saran division. Saran district is also known as Chhapra district because the headquarters of this district is Chhapra. Saran district is bounded by the districts of Siwan, Gopalganj, West Champaran, Muzaffarpur, Patna, Vaishali and Bhojpur of Bihar and Ballia district of Uttar Pradesh. Important rivers flowing through Saran district are Ganga, Gandak, and Ghaghra which encircle the district from south, north east and west side respectively. HISTORICAL BACKGROUND Saran was earlier known as ‘SHARAN’ which means refuge in English, after the name given to a Stupa (pillar) built by Emperor Ashoka. Another view is that the name Saran has been derived from SARANGA- ARANYA or the deer forest since the district was famous for its forests and deer in pre-historic times. In ancient days, the present Saran division, formed a part of Kosala kingdom. According to 'Ain-E-Akbari’, Saran was one of the six Sarkars/ revenue divisions, constituting the province of Bihar. By 1666, the Dutch established their trade in saltpetre at Chhapra. Saran was one of the oldest and biggest districts of Bihar. In 1829, Saran along with Champaran, was included in the Patna Division. Saran was separated from Champaran in 1866 when Champaran district was constituted. In 1981, the three subdivisions of the old Saran district namely Saran, Siwan and Gopalganj became independent districts which formed a part of Saran division. There are a few villages in Saran which are known for their historical and social significance. -

Assessment of Ground Water Resources for Irrigation in Nalanda District of South Bihar, India
Int.J.Curr.Microbiol.App.Sci (2018) 7(2): 1223-1232 International Journal of Current Microbiology and Applied Sciences ISSN: 2319-7706 Volume 7 Number 02 (2018) Journal homepage: http://www.ijcmas.com Original Research Article https://doi.org/10.20546/ijcmas.2018.702.150 Assessment of Ground Water Resources for Irrigation in Nalanda District of South Bihar, India Ravish Chandra*, S.K. Jain and A.K. Singh Dr. Rajendra Prasad Central Agricultural University, Pusa, Samastipur-848125, India *Corresponding author ABSTRACT Ground Water remains the lifeline of socioeconomic development in the Ganga Alluvial Plain (GAP) since the down of civilization in the Indian subcontinent. Assessment of groundwater resources yields knowledge necessary for their informed management and governance. Keeping the importance of the above points a study was conducted for assessment of ground water resources in Nalanda district of south Bihar. The aim for the assessment of groundwater in Nalanda district was to compute a complete evaluation of groundwater resources and produce information that can be incorporated for future requirement. The study was undertaken based on the K e yw or ds recommendation of groundwater estimation committee, 1997 (GEC-97). Methodology used the estimation of annual groundwater recharge from rainfall and other sources, Ganga alluvial including irrigation, water bodies and artificial recharge, determination of present plain, Ground water, GEC 97, status of groundwater utilization and categorization of assessment units based on the Watertable level of groundwater utilization and long-term water level trend. Water level Fluctuation fluctuation techniques and empirical norms were used for recharge estimation. The technique, data collected for investigation were water table fluctuation data, rainfall data Groundwater draft cropping pattern, number of groundwater structures, hydrogeology of area, specific Article Info yield, groundwater draft, pond area etc. -

Womens' Empowerment
Directory of Voluntary Organisations Women’s Empowerment 2010 Documentation Centre for Women and Children (DCWC) National Institute of Public Cooperation and Child Development 5, Siri Institutional Area, Hauz Khas, New Delhi – 110016 Number of Copies: 100 Copyright: National Institute of Public Cooperation and Child Development, 2010 Project Team Project In-charge : Mrs. Meenakshi Sood Project Team : Ms. Renu Banker Ms. Alpana Kumari Computer Assistance : Mrs. Sandeepa Jain Mr. Abhishek Tiwari Acknowledgements : Ministry of Women and Child Development Planning Commission Voluntary Organisations Ministry of Rural Development Ministry of Panchayati Raj Ministry of Tribal Affairs Ministry of Urban Development DISCLAIMER All efforts have been made to verify and collate information about organisations included in the Directory. Information has been collected from various sources, namely directories, newsletters, Internet, proforma filled in by organisations, telephonic verification, letter heads, etc. However, NIPCCD does not take any responsibility for any error that may inadvertently have crept in. The address of offices of organisations, telephone numbers, e-mail IDs, activities, etc. change from time to time, hence NIPCCD may not be held liable for any incorrect information included in the Directory. Foreword Voluntary organisations play a very important role in society. They take up activities in the area of their expertise and provide support to the community in whose welfare they have interest. Social development has been ranked high on the priority list of Government programmes since Independence, and voluntary organisations have been equal partners in accelerating the pace of development. Being in close proximity to the community, voluntary organisations have done pioneering work in many areas, rendered productive services, highlighted several social problems, undertaken advocacy, and lobbied for the rights of the underprivileged. -

Provisional Population Totals, Series-11, Bihar
CENSUS OF INDIA 2001 SERIES- 11 BIHAR PAPER 1 OF 2001 PROVISIONAL POPULATION TOTALS SUDHIR KUMAR RAKESH Director of Census Operations, Bihar Lord Buddha Dedicated to the people of Bihar and enumerators - the data producers. For the benefit of policy makers and research workers - the data consumers. CONTENTS SL. NO. PARTICULARS PAGE NO. 1. Foreword v 2 List of Officers! Officials involved in preparation of Provisional Population Totals vii 3 Figures at a Glance ix 4 State Highlights x 5 Map showing Administrative Division of India Highlighting State xi 6 Map showing Administrative Division of State, 2001 Census xiii 7 Introduction 1 8 Analysis of Results 7· 9 Provisional Population Tables 25 10 Maps 31 11 Diagrams and Charts 39 12 Organisational Chart of Census Hierarchy 49 13 Specimen Copy of Houselist Schedule 51 - 14 Specimen Copy of Household Schedule 53 15 Pictorial 55 FOREWORD After the successful completion of Census of India 2001, it gives me great pleasure to present these provisional population totals for the state of Bihar. This paper gives some basic characteristics of the population of Bihar as on 1st March, 2001 (00.00 hrs.) as recorded during the population enumeration related with the Census of India 2001. These figures are only provisional ones, compiled on the basis of the abstracts of population data prepared by the enumerators. These provisional population figures are being published with the intention of meeting the immediate need of the Government, various organisations, researchers and the general public. It would help provide them the basic population figures as quickly as possible after the population enumeration work has been completed. -
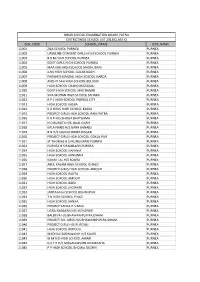
Sch Code School Name Dist Name 11001 Zila School
BIHAR SCHOOL EXAMINATION BOARD PATNA DISTRICTWISE SCHOOL LIST 2013(CLASS X) SCH_CODE SCHOOL_NAME DIST_NAME 11001 ZILA SCHOOL PURNEA PURNEA 11002 URSULINE CONVENT GIRLS HIGH SCHOOL PURNEA PURNEA 11003 B B M HIGH SCHOOL PURNEA PURNEA 11004 GOVT GIRLS HIGH SCHOOL PURNEA PURNEA 11005 MAA KALI HIGH SCHOOL MADHUBANI PURNEA 11006 JLNS HIGH SCHOOL GULAB BAGH PURNEA 11007 PARWATI MANDAL HIGH SCHOOL HARDA PURNEA 11008 ANCHIT SAH HIGH SCHOOL BELOURI PURNEA 11009 HIGH SCHOOL CHANDI RAZIGANJ PURNEA 11010 GOVT HIGH SCHOOL SHRI NAGAR PURNEA 11011 SIYA MOHAN HIGH SCHOOL SAHARA PURNEA 11012 R P C HIGH SCHOOL PURNEA CITY PURNEA 11013 HIGH SCHOOL KASBA PURNEA 11014 K D GIRLS HIGH SCHOOL KASBA PURNEA 11015 PROJECT GIRLS HIGH SCHOOL RANI PATRA PURNEA 11016 K G P H/S BHOGA BHATGAMA PURNEA 11017 N D RUNGTA H/S JALAL GARH PURNEA 11018 KALA NAND H/S GARH BANAILI PURNEA 11019 B N H/S JAGNICHAMPA NAGAR PURNEA 11020 PROJECT GIRLS HIGH SCHOOL GOKUL PUR PURNEA 11021 ST THOMAS H S MUNSHIBARI PURNEA PURNEA 11023 PURNEA H S RAMBAGH,PURNEA PURNEA 11024 HIGH SCHOOL HAFANIA PURNEA 11025 HIGH SCHOOL KANHARIA PURNEA 11026 KANAK LAL H/S SOURA PURNEA 11027 ABUL KALAM HIGH SCHOOL ICHALO PURNEA 11028 PROJECT GIRLS HIGH SCHOOL AMOUR PURNEA 11029 HIGH SCHOOL RAUTA PURNEA 11030 HIGH SCHOOL AMOUR PURNEA 11031 HIGH SCHOOL BAISI PURNEA 11032 HIGH SCHOOL JHOWARI PURNEA 11033 JANTA HIGH SCHOOL BISHNUPUR PURNEA 11034 T N HIGH SCHOOL PIYAZI PURNEA 11035 HIGH SCHOOL KANJIA PURNEA 11036 PROJECT KANYA H S BAISI PURNEA 11037 UGRA NARAYAN H/S VIDYAPURI PURNEA 11038 BALDEVA H/S BHAWANIPUR RAJDHAM