Are Sinus Node Dysfunction and Pacemaker Implantation More Common in Patients with Non Ablated Atrial Fibrillation ?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Syndrome of Alternating Bradycardia and Tachycardia by D
Br Heart J: first published as 10.1136/hrt.16.2.208 on 1 April 1954. Downloaded from THE SYNDROME OF ALTERNATING BRADYCARDIA AND TACHYCARDIA BY D. S. SHORT From the National Heart Hospita. Received September 15, 1953 Among the large number of patients suffering from syncopal attacks who attended the National Heart Hospital during a four-year period, there were four in whom examination revealed sinus bradycardia alternating with prolonged phases of auricular tachycardia. These patients presented a difficult problem in treatment. Each required at least one admission to hospital and in one case the symptoms were so intractable as to necessitate six admissions in five years. Two patients had mitral valve disease, one of them with left bundle branch block. One had aortic valve sclerosis while the fourth had no evidence of heart disease. THE HEART RATE The sinus rate usually lay between 30 and 50 a minute, a rate as slow as 22 a minute being observed in one patient (Table I). Sinus arrhythmia was noted in all four patients, wandering of TABLE I http://heart.bmj.com/ RATE IN SINus RHYTHM AND IN AURICULAR TACHYCARDIA Rate in Case Age Sex Associated Rate in auricular tachycardia heart disease sinus rhythm Auricular Venliicular 1 65 M Aortic valve sclerosis 28-48 220-250 60-120 2 47 F Mitral valve disease 35-75 180-130 90-180 on September 26, 2021 by guest. Protected copyright. 3 38 F Mitral valve disease 22-43 260 50-65 4 41 F None 35-45 270 110 the pacemaker in three, and periods of sinus standstill in two (Fig. -

Basic Rhythm Recognition
Electrocardiographic Interpretation Basic Rhythm Recognition William Brady, MD Department of Emergency Medicine Cardiac Rhythms Anatomy of a Rhythm Strip A Review of the Electrical System Intrinsic Pacemakers Cells These cells have property known as “Automaticity”— means they can spontaneously depolarize. Sinus Node Primary pacemaker Fires at a rate of 60-100 bpm AV Junction Fires at a rate of 40-60 bpm Ventricular (Purkinje Fibers) Less than 40 bpm What’s Normal P Wave Atrial Depolarization PR Interval (Normal 0.12-0.20) Beginning of the P to onset of QRS QRS Ventricular Depolarization QRS Interval (Normal <0.10) Period (or length of time) it takes for the ventricles to depolarize The Key to Success… …A systematic approach! Rate Rhythm P Waves PR Interval P and QRS Correlation QRS Rate Pacemaker A rather ill patient……… Very apparent inferolateral STEMI……with less apparent complete heart block RATE . Fast vs Slow . QRS Width Narrow QRS Wide QRS Narrow QRS Wide QRS Tachycardia Tachycardia Bradycardia Bradycardia Regular Irregular Regular Irregular Sinus Brady Idioventricular A-Fib / Flutter Bradycardia w/ BBB Sinus Tach A-Fib VT PVT Junctional 2 AVB / II PSVT A-Flutter SVT aberrant A-Fib 1 AVB 3 AVB A-Flutter MAT 2 AVB / I or II PAT PAT 3 AVB ST PAC / PVC Stability Hypotension / hypoperfusion Altered mental status Chest pain – Coronary ischemic Dyspnea – Pulmonary edema Sinus Rhythm Sinus Rhythm P Wave PR Interval QRS Rate Rhythm Pacemaker Comment . Before . Constant, . Rate 60-100 . Regular . SA Node Upright in each QRS regular . Interval =/< leads I, II, . Look . Interval .12- .10 & III alike .20 Conduction Image reference: Cardionetics/ http://www.cardionetics.com/docs/healthcr/ecg/arrhy/0100_bd.htm Sinus Pause A delay of activation within the atria for a period between 1.7 and 3 seconds A palpitation is likely to be felt by the patient as the sinus beat following the pause may be a heavy beat. -

Sinus Node Ischemia—A Unique Presentation
International Journal of Clinical Medicine, 2015, 6, 50-54 Published Online January 2015 in SciRes. http://www.scirp.org/journal/ijcm http://dx.doi.org/10.4236/ijcm.2015.61007 Sinus Node Ischemia—A Unique Presentation Jwalit Morakhia1, Padmakumar Ramachandran1, Naveen Chandra Ganiga Sanjeeva1, Harikrishna Damodaran2, Shivani Kothari3, Ashok Thakkar3 1Department of Cardiology, Kasturba Medical College & Hospital, Karnataka, India 2Department of Cardiology, Pariyaram Medical College, Kerala, India 3Department of Clinical Trials, Sahajanand Medical Technologies Pvt. Ltd., Gujarat, India Email: [email protected] Received 27 December 2014; accepted 13 January 2015; published 20 January 2015 Copyright © 2015 by authors and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract Sinus node dysfunction, as the sole manifestation of an acute coronary syndrome, is rare. We re- port a case of ischemic dysfunction of the sinus node in a patient who had previously undergone coronary artery bypass grafting for triple vessel disease. Intermittent rest angina with a junctional rhythm was noted in spite of patent grafts to all three vessels, which resolved after percutaneous revascularization of the right coronary artery. Keywords Sinus Node, Angina, Acute Coronary Syndrome, Thrombus Aspiration 1. Introduction Patients presenting with acute coronary syndromes, with atypical symptoms, are frequently misdiagnosed and under-treated. Embolic phenomena are sometimes overlooked by interventionalists as percutaneous coronary intervention is a specialty which primarily focuses on stenosis and occlusions [1]. We report a case of reversible sinus node dysfunction in the unique setting of post-coronary artery bypass grafting (CABG) status with patent grafts. -

Basic Cardiac Rhythms – Identification and Response Module 1 ANATOMY, PHYSIOLOGY, & ELECTRICAL CONDUCTION Objectives
Basic Cardiac Rhythms – Identification and Response Module 1 ANATOMY, PHYSIOLOGY, & ELECTRICAL CONDUCTION Objectives ▪ Describe the normal cardiac anatomy and physiology and normal electrical conduction through the heart. ▪ Identify and relate waveforms to the cardiac cycle. Cardiac Anatomy ▪ 2 upper chambers ▪ Right and left atria ▪ 2 lower chambers ▪ Right and left ventricle ▪ 2 Atrioventricular valves (Mitral & Tricuspid) ▪ Open with ventricular diastole ▪ Close with ventricular systole ▪ 2 Semilunar Valves (Aortic & Pulmonic) ▪ Open with ventricular systole ▪ Open with ventricular diastole The Cardiovascular System ▪ Pulmonary Circulation ▪ Unoxygenated – right side of the heart ▪ Systemic Circulation ▪ Oxygenated – left side of the heart Anatomy Coronary Arteries How The Heart Works Anatomy Coronary Arteries ▪ 2 major vessels of the coronary circulation ▪ Left main coronary artery ▪ Left anterior descending and circumflex branches ▪ Right main coronary artery ▪ The left and right coronary arteries originate at the base of the aorta from openings called the coronary ostia behind the aortic valve leaflets. Physiology Blood Flow Unoxygenated blood flows from inferior and superior vena cava Right Atrium Tricuspid Valve Right Ventricle Pulmonic Valve Lungs Through Pulmonary system Physiology Blood Flow Oxygenated blood flows from the pulmonary veins Left Atrium Mitral Valve Left Ventricle Aortic Valve Systemic Circulation ▪ Blood Flow Through The Heart ▪ Cardiology Rap Physiology ▪ Cardiac cycle ▪ Represents the actual time sequence between -

An Extremely Rare Cause of Wolff-Parkinson
108 Erciyes Med J 2019; 41(1): 108–10 • DOI: 10.14744/etd.2018.18165 An Extremely Rare Cause of Wolff-Parkinson-White Syndrome: Rhabdomyoma in Association With Tuberous Sclerosis CASE REPORT Özlem Elkıran , Cemşit Karakurt , Damla İnce ABSTRACT Rhabdomyomas are the most common primary cardiac tumors in infants and children. They are usually associated with tuberous sclerosis (TS). As the tumors tend to regress spontaneously, surgical intervention is not usually performed unless they become obstructive or cause incessant arrhythmias. We report an extremely rare case of rhabdomyoma serving as a substrate for Wolff-Parkinson-White (WPW) syndrome and intractable supraventricular tachycardia accompanied by TS. Our case is particularly interesting because it was diagnosed prenatally. The signs of WPW syndrome disappeared from the elec- trocardiogram with the regression of the tumor. Keywords: Wolff-Parkinson-White Syndrome, child, rhabdomyoma INTRODUCTION Rhabdomyomas are the most common cardiac tumors in infants and children, and they are closely related with tuberous sclerosis (TS). A significant part of rhabdomyomas is asymptomatic, and they regress on follow-up. However, symptoms of cardiac failure, arrhythmias, and obstruction can be observed depending on their location in the heart. They require urgent medical or surgical treatment (1, 2). Cite this article as: Elkıran Ö, Karakurt C, İnce D. An Extremely Rhabdomyoma-related arrhythmias are reported as premature atrial and ventricular contractions, supraventricular Rare Cause of and ventricular tachycardia, sinus node dysfunction, atrioventricular block, and Wolff-Parkinson-White (WPW) Wolff-Parkinson-White syndrome (1, 3, 4). There are only a few studies of WPW syndrome occurring in association with TS, with and Syndrome: Rhabdomyoma in Association With without rhabdomyoma. -

Case Report Chagas Cardiomyopathy Presenting As Symptomatic Bradycardia: an Underappreciated Emerging Public Health Problem in the United States
Hindawi Case Reports in Cardiology Volume 2017, Article ID 5728742, 5 pages https://doi.org/10.1155/2017/5728742 Case Report Chagas Cardiomyopathy Presenting as Symptomatic Bradycardia: An Underappreciated Emerging Public Health Problem in the United States Richard Jesse Durrance,1 Tofura Ullah,1 Zulekha Atif,1 William Frumkin,2 and Kaushik Doshi1 1 Department of Internal Medicine, Jamaica Hospital Medical Center, 8900 Van Wyck Expressway, Jamaica, NY 11418, USA 2Department of Cardiology, Jamaica Hospital Medical Center, 8900 Van Wyck Expressway, Jamaica, NY 11418, USA Correspondence should be addressed to Richard Jesse Durrance; [email protected] Received 13 February 2017; Accepted 18 July 2017; Published 16 August 2017 Academic Editor: Aiden Abidov Copyright © 2017 Richard Jesse Durrance et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Chagas cardiomyopathy (CCM) is traditionally considered a disease restricted to areas of endemicity. However, an estimated 300,000 people living in the United States today have CCM, of which its majority is undiagnosed. Wepresent a case of CCM acquired in an endemic area and detected in its early stage. A 42-year-old El Salvadoran woman presented with recurrent chest pain and syncopal episodes. Significant family history includes a sister inEl Salvador who also began suffering similar episodes. Physical exam and ancillary studies were only remarkable for sinus bradycardia. The patient was diagnosed with symptomatic sinus bradycardia and a pacemaker was placed. During her hospital course, Chagas serology was ordered given the epidemiological context from which she came. -

Sinus Bradycardia
British Heart Journal, I97I, 33, 742-749. Br Heart J: first published as 10.1136/hrt.33.5.742 on 1 September 1971. Downloaded from Sinus bradycardia Dennis Eraut and David B. Shaw From the Cardiac Department, Royal Devon and Exeter Hospital, Exeter, Devon This paper presents thefeatures of 46 patients with unexplained bradycardia. Patients were ad- mitted to the study if their resting atrial rate was below 56 a minute on two consecutive occasions. Previous electrocardiograms and the response to exercise, atropine, and isoprenaline were studied. The ages of thepatients variedfrom I3 to 88years. Only 8 had a past history ofcardiovascular disease other than bradycardia, but 36 hJd syncopal or dizzy attacks. Of the 46 patients, 35 had another arrhythmia in addition to bradycardia; at some stage, i6 had sinus arrest, i.5 hadjunc- tional rhythm, 12 had fast atrial arrhythmia, I6 had frequent extrasystoles, and 6 had atrio- ventricular block. None had the classical features of sinoatrial block. Arrhythmias were often produced by exercise, atropine, or isoprenaline. Drug treatment was rarely satisfactory, but only i patient needed a permanent pacemaker. It is suggested that the majority of the patients were suffering from a pathological form of sinus bradycardia. The aetiology remains unproven, but the most likely explanation is a loss of the inherent rhythmicity of the sinoatrial node due to a primary degenerative disease. The descriptive title of 'the lazy sinus syndrome' is suggested. copyright. Bradycardia with a slow atrial rate is usually attempt to define the clinical syndrome of regarded as an innocent condition common in bradycardia with a pathologically slow atrial certain types of well-trained athlete, but occa- rate and to clarify the nature of the arrhyth- sionally it may occur in patients with symp- mia. -
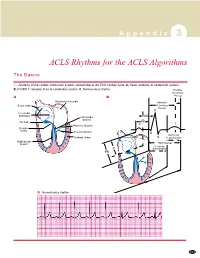
ACLS Rhythms for the ACLS Algorithms
A p p e n d i x 3 ACLS Rhythms for the ACLS Algorithms The Basics 1. Anatomy of the cardiac conduction system: relationship to the ECG cardiac cycle. A, Heart: anatomy of conduction system. B, P-QRS-T complex: lines to conduction system. C, Normal sinus rhythm. Relative Refractory A B Period Bachmann’s bundle Absolute Sinus node Refractory Period R Internodal pathways Left bundle AVN branch AV node PR T Posterior division P Bundle of His Anterior division Q Ventricular Purkinje fibers S Repolarization Right bundle branch QT Interval Ventricular P Depolarization PR C Normal sinus rhythm 253 A p p e n d i x 3 The Cardiac Arrest Rhythms 2. Ventricular Fibrillation/Pulseless Ventricular Tachycardia Pathophysiology ■ Ventricles consist of areas of normal myocardium alternating with areas of ischemic, injured, or infarcted myocardium, leading to chaotic pattern of ventricular depolarization Defining Criteria per ECG ■ Rate/QRS complex: unable to determine; no recognizable P, QRS, or T waves ■ Rhythm: indeterminate; pattern of sharp up (peak) and down (trough) deflections ■ Amplitude: measured from peak-to-trough; often used subjectively to describe VF as fine (peak-to- trough 2 to <5 mm), medium-moderate (5 to <10 mm), coarse (10 to <15 mm), very coarse (>15 mm) Clinical Manifestations ■ Pulse disappears with onset of VF ■ Collapse, unconsciousness ■ Agonal breaths ➔ apnea in <5 min ■ Onset of reversible death Common Etiologies ■ Acute coronary syndromes leading to ischemic areas of myocardium ■ Stable-to-unstable VT, untreated ■ PVCs with -

Long QT Syndrome in Neonates
View metadata, citation and similar papers at core.ac.uk brought to you by CORE Journal of the American College of Cardiology providedVol. by Elsevier 43, No. - 5,Publisher 2004 Connector © 2004 by the American College of Cardiology Foundation ISSN 0735-1097/04/$30.00 Published by Elsevier Inc. doi:10.1016/j.jacc.2003.09.049 Long QT Syndrome in Neonates Conduction Disorders Associated With HERG Mutations and Sinus Bradycardia With KCNQ1 Mutations Jean-Marc Lupoglazoff, MD, PHD,*† Isabelle Denjoy, MD,*†‡ Elisabeth Villain, MD,§ Ve´ronique Fressart, MD, Franc¸oise Simon, Andre´Bozio, MD,¶ Myriam Berthet,† Nawal Benammar,† Bernard Hainque, PHD,† Pascale Guicheney, PHD† Paris and Lyon, France OBJECTIVES We hypothesized that neonatal long QT syndrome (LQTS) with 2:1 atrioventricular block (AVB) could be related to HERG mutations. BACKGROUND Early onset of LQTS is rare but carries a high risk of life-threatening events such as ventricular arrhythmias and conduction disorders. There are no data on possible gene specificity. METHODS We analyzed the characteristics and outcomes of 23 neonate probands from our LQTS population. Samples of DNA were available in 18 cases. RESULTS Long QT syndrome was diagnosed because of corrected QT interval (QTc) prolongation (mean QTc of 558 Ϯ 62 ms) and neonatal bradycardia attributable to sinus bradycardia (n ϭ 8) or 2:1 AVB (n ϭ 15). Symptoms included syncope (n ϭ 2), torsades de pointes (n ϭ 7), and hemodynamic failure (n ϭ 6). Three infants with 2:1 AVB died during the first month of life. During the neonatal period, all living patients received beta-blockers (BB) and 13 had a combination of BB and permanent cardiac pacing. -
A Rare Case of Syncope Secondary to Sinus Node Dysfunction Associated with Brugada Syndrome Maya Khodor, MD1* and Joseph Chattahi, MD2
ISSN: 2378-2951 Khodor and Chattahi. Int J Clin Cardiol 2021, 8:223 DOI: 10.23937/2378-2951/1410223 Volume 8 | Issue 2 International Journal of Open Access Clinical Cardiology CASE REPORT A Rare Case of Syncope Secondary to Sinus Node Dysfunction Associated with Brugada Syndrome Maya Khodor, MD1* and Joseph Chattahi, MD2 1 American University of Caribbean, USA Check for 2Beaumont Hospital, Dearborn, Michigan, USA updates *Corresponding author: Maya Khodor, MD, American University of Caribbean, USA, Tel: 407-353-8875 diagnosed Brugada syndrome but was later found to Keywords have evidence of sinus node dysfunction. We review Brugada, Sinus node dysfunction, Syncope the relevant literature and discuss the management. Case Presentation Introduction A 31-year-old male with no significant past medi- Brugada Syndrome is a rare arrhythmogenic entity cal history presents after a witnessed syncopal episo- that poses a risk of sudden cardiac death due to ven- de. He denied any pre or post syncopal symptoms of tricular arrhythmias. Sinus node dysfunction is a less chest pain, palpitations, fevers, nausea, loss of bowel or recognized and acknowledged conduction abnormality associated with Brugada syndrome, but nevertheless bladder control or tongue biting. He does not take any an important potential manifestation that can alter ma- medications and denied any family history of sudden nagement. We present a case of a young patient who cardiac death. His physical exam and laboratory workup presented with syncope initially presumed to be secon- were unremarkable. His ECG showed sinus rhythm with dary to a ventricular arrhythmia in the setting of newly coved ST segment elevation and T wave inversions in Figure 1: ECG with normal sinus rhythm and type-1 Brugada pattern. -

The Bradycardia-Tachycardia Syndrome Treatment with Cardiac Drugs and Adrenal Corticosteroid Junichi FUJII, M.D., Nobumitsu TAKA
The Bradycardia-Tachycardia Syndrome Treatment with Cardiac Drugs and Adrenal Corticosteroid Junichi FUJII, M.D., Nobumitsu TAKAHASHI,M.D., and Kazuzo KATO, M.D. Seven patients of S-A block complicated by tachycardic paroxysms of atrial fibrillation or flutter were described and the medical treatment in this syndrome was reappraised. Damage to S-A node and adjacent atrial tissue was assumed in all patients. All the patients had syncopal attacks associated with cardiac arrest occurring especially at the termina- tion of tachycardia. Overdrive suppression of diseased S-A node and lower automatic pacemakers was demonstrated by ECG recordings. The term "bradycardia-tachycardia syndrome" or "syndrome of alternating bradycardia and tachycardia" seemed appropriate. In spite of difficulty of medical treatment reiterated by previous de- scriptions, 6 of 7 patients were improved with drug therapy, including adrenal corticosteroid. Adrenal corticosteroid in combination with or- ciprenaline or belladonna alkaloids was most helpful among the drugs used. Obviously, pacemaker implantation should be performed without delay in patients with frequent and prolonged attacks of syncope. But not all patients have need of pacemaker implantation. A trial of drug therapy may be permitted in many patients of this syndrome before in- troduction of pacemaker. Additional Indexing Words: Sick sinus syndrome S-A block Atrial tachyarrhythmias Syn- cope Overdrive suppression ECENTLY there have been some reports concerning the patients with S-A block or sinus bradycardia accompanied by paroxysmal atrial tachy- arrhythmias such as fibrillation, flutter and paroxysmal tachycardia. As pointed out by several authors, these patients repeatedly exhibited syncopal attacks associated with asystole following termination of the tachycardia. -

Sick Sinus Syndrome After the Maze Procedure Performed
ORIGINAL RESEARCH Sick Sinus Syndrome After the Maze Procedure Performed Concomitantly With Mitral Valve Surgery Min Soo Cho, MD; Ran Heo, MD; Xin Jin, MD; Jung-Bok Lee, PhD; Sahmin Lee, MD, PhD; Dae-Hee Kim, MD, PhD; Joon Bum Kim, MD, PhD; Jun Kim, MD, PhD; Sung-Ho Jung, MD, PhD; Suk Jung Choo, MD, PhD; Jong-Min Song, MD, PhD; Gi-Byoung Nam, MD, PhD; Kee-Joon Choi, MD, PhD; Duk-Hyun Kang, MD, PhD; Cheol Hyun Chung, MD, PhD; Jae Won Lee, MD, PhD; You-Ho Kim, MD, PhD; Jae-Kwan Song, MD, PhD Background-—To characterize the development of sick sinus syndrome (SSS) after the additive maze procedure (MP) during mitral valve surgery. Methods and Results-—Follow-up data (median, 3.6 years) of 750 patients with a prevalence of rheumatic cause of 57.6% were analyzed. SSS occurred in 35 patients with a time-dependent increase: the incidence rates at 1, 2, and 4 years after surgery were 2.9%, 3.7%, and 4.3%, respectively. The additive MP showed higher risks of SSS development (hazard ratio, 7.44; 95% confidence interval, 3.45–16.05; P<0.001) and pacemaker implantation (hazard ratio, 3.61; 95% confidence interval, 1.95–6.67; P<0.001). Patients who developed SSS showed higher 4-year rates of clinical events (death, stroke, and hospital admission) (67.5Æ8.5% versus 33.0Æ1.9%; P<0.001). After adjustment for age and preoperative peak systolic pulmonary artery pressure, the lesion extent (biatrial versus left atrial MP), not the underlying cause (rheumatic versus nonrheumatic), was independently associated with SSS development (hazard ratio, 3.58; 95% confidence interval, 1.08–11.86; P=0.037).