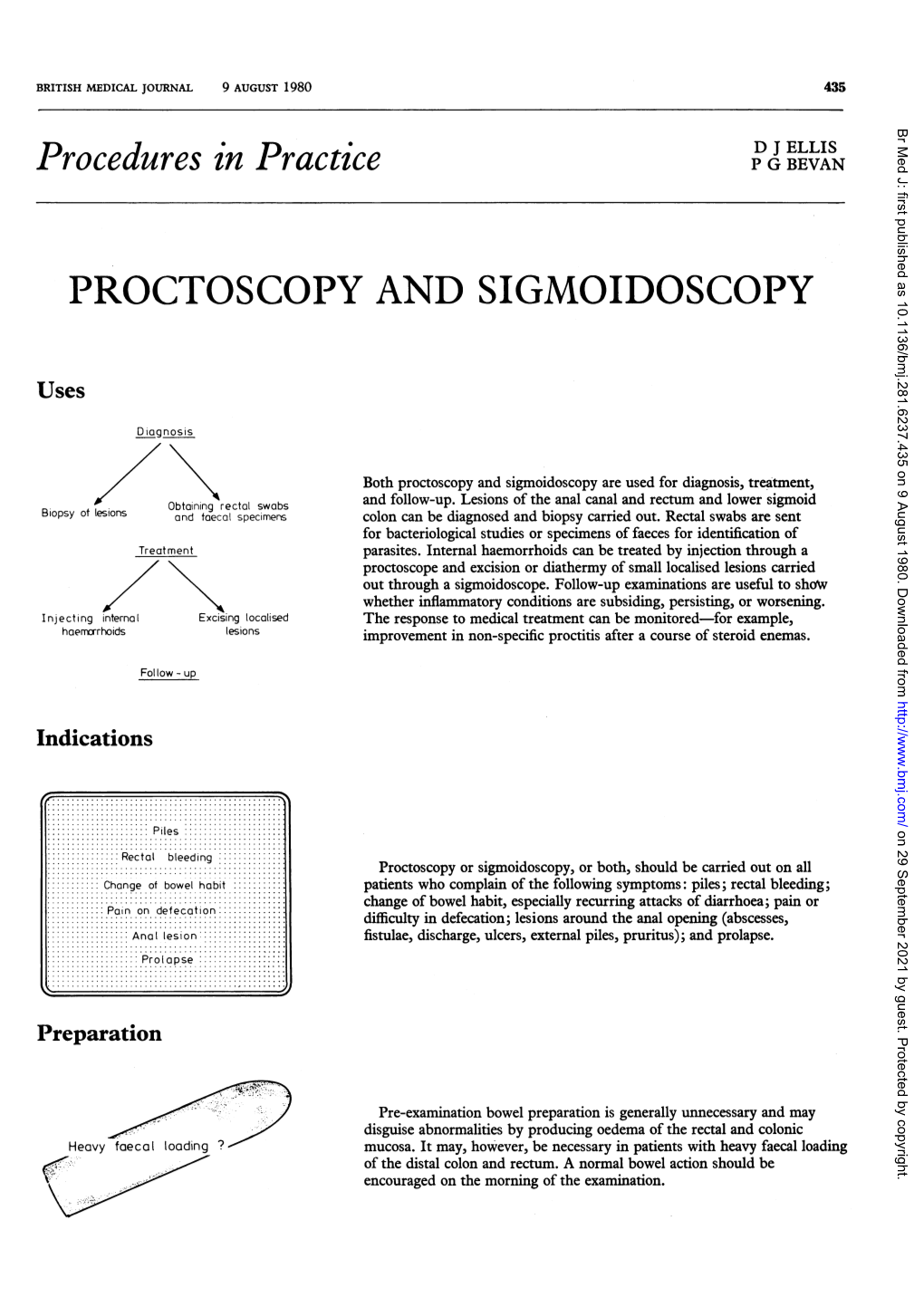
Procedures in Practice P G BEVAN
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Practice Parameters for the Treatment of Patients with Dominantly Inherited Colorectal Cancer
Practice Parameters For The Treatment Of Patients With Dominantly Inherited Colorectal Cancer Diseases of the Colon & Rectum 2003;46(8):1001-1012 Prepared by: The Standards Task Force The American Society of Colon and Rectal Surgeons James Church, MD; Clifford Simmang, MD; On Behalf of the Collaborative Group of the Americas on Inherited Colorectal Cancer and the Standards Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons is dedicated to assuring high quality patient care by advancing the science, prevention, and management of disorders and diseases of the colon, rectum, and anus. The standards committee is composed of Society members who are chosen because they have demonstrated expertise in the specialty of colon and rectal surgery. This Committee was created in order to lead international efforts in defining quality care for conditions related to the colon, rectum, and anus. This is accompanied by developing Clinical Practice Guidelines based on the best available evidence. These guidelines are inclusive, and not prescriptive. Their purpose is to provide information on which decisions can be made, rather than dictate a specific form of treatment. These guidelines are intended for the use of all practitioners, health care workers, and patients who desire information about the management of the conditions addressed by the topics covered in these guidelines. Practice Parameters for the Treatment of Patients With Dominantly Inherited Colorectal Cancer Inherited colorectal cancer includes two main syndromes in which predisposition to the disease is based on a germline mutation that may be transmitted from parent to child. -

Endoscopy Rotation Coordination and Goals and Objects Department of Surgery Stanford School of Medicine (8/15/17, Jnl)
Endoscopy Rotation Coordination And Goals and Objects Department of Surgery Stanford School of Medicine (8/15/17, jnl) Rotation Director: James Lau, MD ATTENDINGS and CONTACT INFORMATION Cell Phone E-mail Address James Lau, MD (702) 306-8780 [email protected] Homero Rivas, MD MBA (972) 207-2381 [email protected] Dan Azagury, MD (650) 248-3173 [email protected] Shai Friedland, MD [email protected] Andrew Shelton, MD [email protected] Natalie Kirilcuk, MD [email protected] Cindy Kin, MD [email protected] Laren Becker, MD [email protected] Jennifer Pan, MD [email protected] Suzanne Matsui, MD [email protected] Ramsey Cheung, MD [email protected] KEYPOINT The key for this rotation is that you need to show initiative. TEXT Practical Gastrointestinal Endoscopy: The Fundamentals. Sixth Edition. By Peter B. Cotton, Christopher B. Williams, Robert H. Hawes and Brian P. Saunders. You are responsible for the material to enhance your understanding and supplement your past experiences. Lots of pictures and tips and tricks. Quick read. Copy of text available for purchase on Amazon.com or for check out from the Lane Library. Procedure Schedule Monday Tuesday Wednesday Thursday Friday Laren Becker Jennifer Pan Shelton/Kirilcuk/Kin Ramsey Suzanne (VA (VA Colonoscopy 8:00 am Cheung (VA Matsui (VA Livermore) Livermore) (Stanford Endoscopy) Livermore) Livermore) Every other Tuesday Rivas/Lau alternating Upper/Occasional Lower 1 Endoscopy 9a-1p (Stanford Endoscopy) Suzanne Matsui (VA Livermore) The Staff Drs. Becker, Cheung, Pan, and Matsui are gastroenterologists that perform 75% colonoscopies and 25% upper endoscopies at the Livermore location for the Palo Alto VA. -

Colon and Rectal Surgery Case Log Instructions Review Committee for Colon and Rectal Surgery
Colon and Rectal Surgery Case Log Instructions Review Committee for Colon and Rectal Surgery Background The ACGME Case Log System is a data depository which provides a mechanism that supports programs in complying with requirements, and also provides a uniform mechanism to verify the clinical education of residents among programs. The Case Log System is designed to capture and categorize a resident’s experience with patient care. It was initially instituted in 2001, and the Review Committee for Colon and Rectal Surgery has required its use by accredited programs since 2005. It is the intention of the Review Committee for Colon and Rectal Surgery that each resident has a reasonably equivalent educational experience to prepare for the practice of the specialty. As part of the process, the case numbers for each resident completing a program are collected and analyzed. To accomplish this complex task, a structured database has been created using standard codes for diagnoses and procedures. The Case Log System helps assess the breadth and depth of clinical experience provided to each colon and rectal surgery resident by his or her program with the ultimate goal of improving the programs themselves. It is the responsibility of the individual residents to accurately and in a timely manner enter their case data. The data entered will be monitored by the program directors and analyzed by the Review Committee. Separate analysis reports are created annually for the Committee, for program directors, and for residents. Additionally, the ACGME provides information regarding individual residents’ experience to the American Board of Colon and Rectal Surgery (ABCRS) as one criterion for their admission to the ABCRS’s exam process. -
Flexible Sigmoidoscopy in Asymptomatic Patients with Negative Fecal Occult Blood Tests Joy Garrison Cauffman, Phd, Jimmy H
Flexible Sigmoidoscopy in Asymptomatic Patients with Negative Fecal Occult Blood Tests Joy Garrison Cauffman, PhD, Jimmy H. Hara, MD, Irving M. Rasgon, MD, and Virginia A. Clark, PhD Los Angeles, California Background. Although the American Cancer Society and tients with lesions were referred for colonoscopy; addi others haw established guidelines for colorectal cancer tional lesions were found in 14%. A total of 62 lesions screening, questions of who and how to screen still exist. were discovered, including tubular adenomas, villous Methods. A 60-crn flexible sigmoidoscopy was per adenomas, tubular villous adenomas (23 of the adeno formed on 1000 asymptomatic patients, 45 years of mas with atypia), and one adenocarcinoma. The high age or older, with negative fecal occult blood tests, est percentage of lesions discovered were in the sig who presented for routine physical examinations. Pa moid colon and the second highest percentage were in tients with clinically significant lesions were referred for the ascending colon. colonoscopy. The proportion of lesions that would not Conclusions. The 60-cm flexible sigmoidoscope was have been found if the 24-cm rigid or the 30-cm flexi able to detect more lesions than either the 24-cm or ble sigmoidoscope had been used was identified. 30-cm sigmoidoscope when used in asymptomatic pa Results. Using the 60-cm flexible sigmoidoscope, le tients, 45 years of age and over, with negative fecal oc sions were found in 3.6% of the patients. Eighty per cult blood tests. When significant lesions are discovered cent of the significant lesions were beyond the reach of by sigmoidoscopy, colonoscopy should be performed. -

What Is a Rigid Sigmoidoscopy?
Learning about . Rigid Sigmoidoscopy What is a rigid sigmoidoscopy? Rigid sigmoidoscopy is a procedure done to look at the rectum and lower colon. The doctor uses a special tube called a scope. The scope has a light and a small glass window at the end so the doctor can see inside. lower colon rectum anus or opening to rectum This procedure is done for many reasons. Some reasons are: • to look for the cause of rectal bleeding • a tissue sample to test called a biopsy When small growths of tissue called polyps are seen, these are removed. The procedure takes about 5 minutes but plan to be at the hospital for ½ hour. Are there any complications to this procedure? Your doctor will explain the problems that can occur before you sign a consent form. Problems are rare but include: The scope can damage the lining of the colon. The scope can cause severe bleeding by damaging the wall of the colon. You may have blood spotting if a biopsy is done or a polyp is removed. Since the doctor and nurse are with you all of the time, they can manage any problem that may occur. What do I need to do to get ready at home? 4 to 5 days before your procedure: Taking medications: Your doctor may want you to stop taking certain medications 4 to 5 days before the procedure. If you need to stop any medications, your doctor will tell you during the office visit. If you have any questions, call the doctor’s office. Buying a Fleet enema: Your bowel must be clean and empty of waste material before this procedure. -

04. EDITORIAL 1/2/06 10:34 Página 853
04. EDITORIAL 1/2/06 10:34 Página 853 1130-0108/2005/97/12/853-859 REVISTA ESPAÑOLA DE ENFERMEDADES DIGESTIVAS REV ESP ENFERM DIG (Madrid) Copyright © 2005 ARÁN EDICIONES, S. L. Vol. 97, N.° 12, pp. 853-859, 2005 Cost-effectiveness of abdominal ultrasonography in the diagnosis of colorectal carcinoma Colorectal cancer (CRC) is a most common neoplasm, and the second leading cause of cancer-related death. CRC was responsible for 11% of cancer-related deaths in males, and for 15% of cancer-related deaths in females according to data for year 2000. Most recent data reported in Spain on death causes in 2002 suggest that CRC was responsible for 12,183 deaths (6,896 males with a mean age of 70 years, and 5,287 women with a mean age of 71 years). In these tumors, mortality data do not reflect the true incidence of this disease, since survival has improved in recent years, particularly in younger individuals. In contrast to other European countries, Spain ranks in an intermediate position in terms of CRC-re- lated incidence and mortality. This risk clearly increases with age, with a notori- ous rise in incidence from 50 years of age on. Survival following CRC detection and management greatly depends upon tumor stage at the time of diagnosis; hence the importance of early detection and –because of their malignant poten- tial– of the recognition and excision of colorectal adenomas. Thus, polypectomy and then surveillance are the primary cornerstones in the prevention of CRC (1-4). For primary prevention, fiber-rich diets, physical exercising, and the avoidance of overweight, smoking, and alcohol have been recommended. -

Flexible Sigmoidoscopy with Haemorrhoid Banding
Flexible sigmoidoscopy with haemorrhoid banding You have been referred by your doctor to have a flexible sigmoidoscopy which may also include haemorrhoid banding. If you are unable to keep your appointment, please notify the department as soon as possible. This will allow staff to give your appointment to someone else and they will arrange another date and time for you. This booklet has been written to explain the procedures. This will help you make an informed decision in relation to consenting to the investigation. Please read the booklets and consent form carefully. You will need to complete the enclosed questionnaire. You may be contacted via telephone by a trained endoscopy nurse before the procedure, to go through the admission process and answer any queries you may have. If you are not contacted please come to your appointment at the time stated on your letter. If you have any mobility problems or there is a possibility you could be pregnant please telephone appointments staff on 01284 712748. Please note the appointment time is your arrival time on the unit, and not the time of your procedure. Please remember there will be other patients in the unit who arrive after you, but are taken in for their procedure before you. This is either for medical reasons or they are seeing a different Doctor. Due to the limited space available and to maintain other patients’ privacy and dignity, we only allow patients (and carers) through to the ward area. Relatives/escorts will be contacted once the person is available for collection. The Endoscopy Unit endeavours to offer single sex facilities, and we aim to make your stay as comfortable and stress free as possible. -
Flexible Sigmoidoscopy – Outpatients
Flexible sigmoidoscopy – Outpatients You have been referred by your doctor to have a flexible sigmoidoscopy. his information booklet has been written to explain the procedure. This will help you to make an informed decision before consenting to the procedure. If you are unable to attend your appointment please inform us as soon as possible. Please ensure you read this booklet and the enclosed consent form thoroughly. Please also complete the enclosed health questionnaire. You may be contacted by an endoscopy trained nurse before your procedure to go through the admission process and answer any queries you may have. If you are not contacted please come to your appointment at the time stated in your letter. Please note your appointment time is your arrival time on the unit and not the time of your procedure. If you have any mobility issues or if there is a possibility you could be pregnant, please contact the appointment staff on 01284 713551 Please remember there will be other patients in the unit who may arrive after you but are taken in for their procedure before you, this is for medical reasons or they are seeing a different doctor. Due to limited space available and to maintain other patients’ privacy and dignity, we only allow patients (and carers) through to the ward area. Relatives/ escorts will be contacted once you are ready for collection. The Endoscopy Unit endeavours to offer single sex facilities, and we aim to make you stay as comfortable and stress free as possible. Source: Endoscopy Reference No: 5035-14 Issue date: 8/1/21 Review date: 8/1/24 Page 1 of 11 Medication If you are taking WARFARIN, CLOPIDOGREL, RIVAROXABAN or any other anticoagulant (blood thinning medication), please contact the appointment staff on 01284 713551, your GP or anticoagulation nurse, as special arrangements may be necessary. -

Endoscopy Matrix
Endoscopy Matrix CPT Description of Endoscopy Diagnostic Therapeutic Code (Surgical) 31231 Nasal endoscopy, diagnostic, unilateral or bilateral (separate procedure) X 31233 Nasal/sinus endoscopy, diagnostic with maxillary sinusoscopy (via X inferior meatus or canine fossa puncture) 31235 Nasal/sinus endoscopy, diagnostic with sphenoid sinusoscopy (via X puncture of sphenoidal face or cannulation of ostium) 31237 Nasal/sinus endoscopy, surgical; with biopsy, polypectomy or X debridement (separate procedure) 31238 Nasal/sinus endoscopy, surgical; with control of hemorrhage X 31239 Nasal/sinus endoscopy, surgical; with dacryocystorhinostomy X 31240 Nasal/sinus endoscopy, surgical; with concha bullosa resection X 31241 Nasal/sinus endoscopy, surgical; with ligation of sphenopalatine artery X 31253 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including frontal sinus exploration, with removal of tissue from frontal sinus, when performed 31254 Nasal/sinus endoscopy, surgical; with ethmoidectomy, partial (anterior) X 31255 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior 31256 Nasal/sinus endoscopy, surgical; with maxillary antrostomy X 31257 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy 31259 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy, with removal of tissue from the sphenoid sinus 31267 Nasal/sinus endoscopy, surgical; with removal of -
Public Use Data File Documentation
Public Use Data File Documentation Part III - Medical Coding Manual and Short Index National Health Interview Survey, 1995 From the CENTERSFOR DISEASECONTROL AND PREVENTION/NationalCenter for Health Statistics U.S. DEPARTMENTOF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics CDCCENTERS FOR DlSEASE CONTROL AND PREVENTlON Public Use Data File Documentation Part Ill - Medical Coding Manual and Short Index National Health Interview Survey, 1995 U.S. DEPARTMENT OF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics Hyattsville, Maryland October 1997 TABLE OF CONTENTS Page SECTION I. INTRODUCTION AND ORIENTATION GUIDES A. Brief Description of the Health Interview Survey ............. .............. 1 B. Importance of the Medical Coding ...................... .............. 1 C. Codes Used (described briefly) ......................... .............. 2 D. Appendix III ...................................... .............. 2 E, The Short Index .................................... .............. 2 F. Abbreviations and References ......................... .............. 3 G. Training Preliminary to Coding ......................... .............. 4 SECTION II. CLASSES OF CHRONIC AND ACUTE CONDITIONS A. General Rules ................................................... 6 B. When to Assign “1” (Chronic) ........................................ 6 C. Selected Conditions Coded ” 1” Regardless of Onset ......................... 7 D. When to Assign -

Digestive Endoscopy in Five Decades
■ COLLEGE LECTURES Digestive endoscopy in five decades Peter B Cotton ABSTRACT – The world of gastroenterology scopy. So-called semi-flexible gastroscopes were changed forever when flexible endoscopes cumbersome and used infrequently by only a few became available in the 1960s. Diagnostic and enthusiasts. therapeutic techniques proliferated and entered the mainstream of medicine, not without some Diagnostic endoscopy controversy. Success resulted in a huge service demand, with the need to train more endo- The first truly flexible gastroscope was developed in 1 This paper is scopists and to organise large endoscopy units the USA, following pioneering work on fibre-optic 2 based on the Lilly and teams of staff. The British health service light transmission in the UK by Harold Hopkins. Lecture given at struggled with insufficient numbers of consul- However, commercial production of endoscopes was the Royal College tants, other staff and resources, and British rapidly dominated by Japanese companies, building of Physicians on endoscopy fell behind that of most other devel- on their earlier expertise with intragastric cameras. 12 April 2005 by oped countries. This situation is now being My involvement began in 1968, whilst doing bench Peter B Cotton addressed aggressively, with many local and research with Dr Brian Creamer at St Thomas’ MD FRCP FRCS, national initiatives aimed at improving access and Hospital, London. An expert in coeliac disease (and Medical Director, choice, and at promoting and documenting jejunal biopsy), he opined that gastroscopy might Digestive Disease quality. Many more consultants are needed and become useful and legitimate only if it became pos- Center, Medical some should be relieved of their internal medi- sible to take target biopsy specimens – since no one University of South Carolina, cine commitment to focus on their specialist seriously believed what endoscopists said that they Charleston, USA skills. -

Anesthesiology Services for Gastrointestinal Endoscopy Reference Number: CP.MP.161 Coding Implications Last Review Date: 05/19 Revision Log
Clinical Policy: Anesthesiology Services for Gastrointestinal Endoscopy Reference Number: CP.MP.161 Coding Implications Last Review Date: 05/19 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Conscious sedation for gastrointestinal (GI) endoscopic procedures is standard of care to relieve patient anxiety and discomfort, improve outcomes of the examination, and decrease the memory of the procedure. A combination of an opioid and benzodiazepine is the recommended regimen for achieving minimal to moderate sedation for upper endoscopy and colonoscopy in people without risk for sedation-related adverse events.5 Generally, the gastroenterologist performing the procedure and/or his/her qualified assistant can adequately manage the administration of conscious sedation and monitoring of the patient. In cases with sedation-related risk factors, additional assistance from an anesthesia team member is required to ensure the safest outcome for the patient. This policy outlines the indications for which anesthesia services are considered medically necessary. Policy/Criteria I. It is the policy of health plans affiliated with Centene Corporation® that anesthesiology services for GI endoscopic procedures is considered medically necessary for the following indications: A. Age < 18 years or ≥ 70 years; B. Pregnancy; C. Increased risk of complications due to physiological status as identified by the American Society of Anesthesiologist (ASA) physical status classification of ASA III or higher; D. Increased risk for airway obstruction because of anatomic variants such as dysmorphic facial features, oral abnormalities, neck abnormalities, or jaw abnormalities; E. History of or anticipated intolerance to conscious sedation (i.e. chronic opioid or benzodiazepine use); F.