A Novel Anatomy Education Method Using a Spatial Reality Display Capable of Stereoscopic Imaging with the Naked Eye
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Claycomo Master List Updated 5.18.21.Xlsx
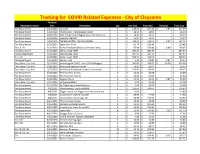
Tracking for COVID Related Expenses - City of Claycomo Purchase Department Name Date Description Qty Unit Cost Extended Shipping Total Cost Fire Department 3/12/2020Cavicide 2$ 128.56 $ 257.12 $ 0.87 $ 257.99 Fire Department 3/18/2020 Thermoscan Thermometer Covers 1$ 18.09 $ 18.09 $ 18.09 Fire Department 3/18/2020 ADC Temple Touch Digital Fever Thermometer 3$ 14.41 $ 43.23 $ 43.23 Fire Department 3/18/2020 Lysol Disinfectant 1$ 45.94 $ 45.94 $ 45.94 Fire Department 3/18/2020 THERMOMETER, EAR PRO 6000W 1$ 240.64 $ 240.64 $ 0.87 $ 241.51 Fire Department 3/23/2020 Super Sani-Cloth 2$ 61.74 $ 123.48 $ 123.48 FD, CH, PD 3/23/2020 Remon Newest 60W UV Germicidal Lamp 2$ 69.99 $ 139.98 $ 8.99 $ 148.97 Fire Department 3/23/2020 Dell Latitude 7290 1$ 487.47 $ 487.47 $ 487.47 Police Department 3/24/2020 Dell Latitude 7290 1$ 487.47 $ 487.47 $ 487.47 City Hall 3/24/2020 Dell Latitude 7290 1$ 558.57 $ 558.57 $ 558.57 Fire Department 3/25/2020Gloves - XLG 4$ 5.45 $ 21.80 $ 0.87 $ 22.67 Fire, Police, City Hall 3/25/2020 VectorFog Go Z200 5 Liter ULV Cold Fogger 1$ 595.00 $ 595.00 $ 35.38 $ 630.38 Fire, Police, City Hall 3/26/2020 3x silicone keyboard cover 3$ 8.99 $ 26.97 $ 26.97 Fire, Police, City Hall 3/27/2020 Mediclean Germicidal Cleaner Concentrate 1$ 174.95 $ 174.95 $ 174.95 Fire Department 3/29/2020 Thermometer Covers 2$ 12.49 $ 24.98 $ 24.98 Fire Department 3/29/2020 Thermometer Covers 2$ 13.80 $ 27.60 $ 27.60 Fire Department 3/30/2020 Surgical Masks 3$ 11.51 $ 34.53 $ 0.87 $ 35.40 Fire, Police, City Hall 3/31/2020 UV Lamp Holders 2$ 9.99 $ -

Evaluating Performance Benefits of Head Tracking in Modern Video
Evaluating Performance Benefits of Head Tracking in Modern Video Games Arun Kulshreshth Joseph J. LaViola Jr. Department of EECS Department of EECS University of Central Florida University of Central Florida 4000 Central Florida Blvd 4000 Central Florida Blvd Orlando, FL 32816, USA Orlando, FL 32816, USA [email protected] [email protected] ABSTRACT PlayStation Move, TrackIR 5) that support 3D spatial in- teraction have been implemented and made available to con- We present a study that investigates user performance ben- sumers. Head tracking is one example of an interaction tech- efits of using head tracking in modern video games. We nique, commonly used in the virtual and augmented reality explored four di↵erent carefully chosen commercial games communities [2, 7, 9], that has potential to be a useful ap- with tasks which can potentially benefit from head tracking. proach for controlling certain gaming tasks. Recent work on For each game, quantitative and qualitative measures were head tracking and video games has shown some potential taken to determine if users performed better and learned for this type of gaming interface. For example, Sko et al. faster in the experimental group (with head tracking) than [10] proposed a taxonomy of head gestures for first person in the control group (without head tracking). A game ex- shooter (FPS) games and showed that some of their tech- pertise pre-questionnaire was used to classify participants niques (peering, zooming, iron-sighting and spinning) are into casual and expert categories to analyze a possible im- useful in games. In addition, previous studies [13, 14] have pact on performance di↵erences. -

Bachelorscriptie De Waarde Van Virtual Reality in Het Toekomstige Ontwerpproces
Bachelorscriptie De waarde van virtual reality in het toekomstige ontwerpproces Auteurs Student T. de Haas 568847 Student R. Versloot 566305 Afstudeerbegeleiders Bedrijfsbegeleider 1e begeleider ir. J. Janssen ABT ir. T. van Dooren 2e begeleider ing. M.A.A. van Muijden MSc Onderwijsinstelling Hogeschool van Arnhem en Nijmegen Afstudeerbedrijf ABT 29 mei 2018, Velp Bachelorscriptie De waarde van virtual reality in het toekomstige ontwerpproces Auteurs Student T. de Haas Studentnummer 568847 Opleiding Bouwkunde Afstudeerrichting Architectuur Student R. Versloot Studentnummer 566305 Opleiding Bouwkunde Afstudeerrichting Architectuur 29 mei 2018, Velp Voorwoord Bij dezen willen wij graag ABT bedanken voor het bieden van de ruimte en ondersteuning in het bepalen van de richting Dit is de scriptie: De waarde van virtual reality in het van het afstudeeronderzoek. toekomstige ontwerpproces. Het onderzoek is gedaan in het kader van het afstuderen aan de opleiding bouwkunde Nadrukkelijk willen wij graag de bedrijfsbegeleider T. van aan de Hogeschool van Arnhem en Nijmegen en is Dooren bedanken voor het mede mogelijk maken van de uitgevoerd in opdracht van ABT. Dit is een multidisciplinair afstudeerplaats binnen ABT en de prettige samenwerking ingenieursbureau met een breed scala aan projecten, zoals: die van het begin tot eind van het afstuderen heeft terminals, rechtbanken, musea en woon/werk complexen. plaatsgevonden. Wij hebben vaak de gelegenheid gekregen om te sparren, wat tot veel waardevolle input voor de scriptie Van februari tot en met mei zijn wij, Reinder Versloot en Timmo heeft geleid. de Haas, bezig geweest met het opstellen, onderzoeken en uitschrijven van de scriptie. Daarnaast willen wij graag de respondenten van de interviews bedanken. -
Whitepaper Head Mounted Displays & Data Glasses Applications and Systems
Whitepaper Head Mounted Displays & Data Glasses Applications and Systems Dr.-Ing. Dipl.-Kfm. Christoph Runde Virtual Dimension Center (VDC) Fellbach Auberlenstr. 13 70736 Fellbach www.vdc-fellbach.de © Competence Centre for Virtual Reality and Cooperative Engineering w. V. – Virtual Dimension Center (VDC) System classes Application fields Directions of development Summary Content . System classes Head Mounted Display (HMD) – Video glasses – Data glasses . Simulator disease / Cyber Sickness . Application fields HMDs: interior inspections, training, virtual hedging engineering / ergonomics . Application fields data glasses: process support, teleservice, consistency checks, collaboration . Directions of development: technical specifications, (eye) tracking, retinal displays, light field technology, imaging depth sensors . Application preconditions information & integration (human, IT, processes) . Final remark 2 SystemSystem classes classes Application fields Directions of development Summary Head Mounted Displays (HMDs) – Overview . 1961: first HMD on market . 1965: 3D-tracked HMD by Ivan Sutherland . Since the 1970s a significant number of HMDs is applied in the military sector (training, additional display) Table: Important HMD- projects since the 1970s [Quelle: Li, Hua et. al.: Review and analysis of avionic helmet-mounted displays. In : Op-tical Engineering 52(11), 110901, Novembre2013] 3 SystemSystem classes classes Application fields Directions of development Summary Classification HMD – Video glasses – Data glasses Head Mounted Display -
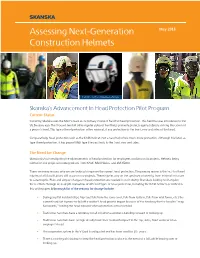
Assessing Next-Generation Construction Helmets
Assessing Next-Generation May 2018 Construction Helmets The KASK - Zenith and Superplasma Helmets Skanska’s Advancement In Head Protection Pilot Program Current Status Currently, Skanska uses the MSA V-Gard as its primary choice of hard hat head protection. This hard hat was introduced to the US 56 years ago. The V Guard (and all other regular styles of hard hats) primarily protects against objects striking the crown of a person’s head. This type of head protection offers minimal, if any protection to the front, rear and sides of the head. Comparatively, head protection such as the KASK helmet (not a hard hat) offers much more protection. Although it is listed as Type I head protection, it has passed ANSI Type II impact tests to the front, rear and sides. The Need for Change Skanska USA is investigating the advancements of head protection for employees working on its projects. Helmets being piloted on our projects include products from KASK, MSA Nexius, and 3M X5000. There are many reasons why we are looking to improve the current head protection. The primary reason is the fact that head injuries of all classifications still occur on our projects. These injuries vary on the spectrum of severity, from minimal in nature to catastrophic. Plain and simple: changes in head protection are needed in our industry. Skanska is looking to champion these efforts through an in-depth evaluation of different types of head protection, including the KASK helmets described in this white paper. A thorough list of the reasons for change include: • During any fall incident (slips, trips and falls from the same level, falls from ladders, falls from wall forms, etc.) the current hard hat is prone to fall off a worker’s head prior to impact because of the tendency for the head to “snap backwards,” leaving the head exposed when protection is most needed. -

The Effect of Eye Protection on SARS-Cov-2 Transmission: a Systematic Review
medRxiv preprint doi: https://doi.org/10.1101/2021.08.08.21261770; this version posted August 9, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . The effect of eye protection on SARS-CoV-2 transmission: a systematic review Oyungerel Byambasuren1, PhD, Postdoctoral Research Fellow; Elaine Beller1, MAppStat, Associate Professor; Justin Clark1, BA, Information Specialist; Peter Collignon2, PhD, Professor; Paul Glasziou1, PhD, Professor, Director Affiliations: 1 Institute for Evidence-Based Healthcare, Bond university, Australia 2 Medical School, Australian National University, Australia Corresponding author: Oyungerel Byambasuren Postdoctoral Research Fellow Institute for Evidence-Based Healthcare Bond University 14 University Dr, Robina QLD 4226 Australia Tel: 61 7 5595 5518 Email: [email protected] NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. medRxiv preprint doi: https://doi.org/10.1101/2021.08.08.21261770; this version posted August 9, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Abstract Background: The effect of eye protection to prevent SARS-CoV-2 infection in the real- world remains uncertain. We aimed to synthesize all available research on the potential impact of eye protection on transmission of SARS-CoV-2. -

Tactical Eyewear Protection Equipment Assessment Report
Tactical Eyewear Protection Equipment Assessment Report May 2020 Approved for Public Release SAVER-T-R-21 The Tactical Eyewear Protection Equipment Assessment Report was funded under Financial Transaction FTLF- 19-00009 from the U.S. Department of Homeland Security, Science and Technology Directorate. The views and opinions of authors expressed herein do not necessarily reflect those of the U.S. Government. Reference herein to any specific commercial products, processes, or services by trade name, trademark, manufacturer, or otherwise does not necessarily constitute or imply its endorsement, recommendation, or favoring by the U.S. Government. The information and statements contained herein shall not be used for the purposes of advertising, nor to imply the endorsement or recommendation of the U.S. Government. With respect to documentation contained herein, neither the U.S. Government nor any of its employees make any warranty, express or implied, including but not limited to the warranties of merchantability and fitness for a particular purpose. Further, neither the U.S. Government nor any of its employees assume any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed; nor do they represent that its use would not infringe privately owned rights. The cover photo and images included herein were provided by the National Urban Security Technology Laboratory, unless otherwise noted. Approved for Public Release ii FOREWORD The U.S. Department of Homeland Security (DHS) established the System Assessment and Validation for Emergency Responders (SAVER) Program to assist emergency responders making procurement decisions. Located within the Science and Technology Directorate (S&T) of DHS, the SAVER Program conducts objective assessments and validations on commercially available equipment and systems and develops knowledge products that provide relevant equipment information to the emergency responder community. -

Using Smart Glasses and Augmented Reality Head-Mounted Displays To
Using smart glasses and augmented reality head-mounted displays to drive supply chain innovation A series exploring Industry 4.0 technologies and their potential impact for enabling digital supply networks in manufacturing Using smart glasses and augmented reality head-mounted displays to drive supply chain innovation Contents What are smart glasses and augmented reality HMDs? 4 Benefits of smart glasses and AR in the supply chain 6 Criteria for evaluation and adoption 8 Key applications for smart glasses in your supply chain 10 Getting started with smart glasses and augmented reality devices 11 Key Deloitte contacts in smart glasses and augmented reality 12 02 Using smart glasses and augmented reality head-mounted displays to drive supply chain innovation Do you need smart glasses in your supply chain? Smart glasses are already being used to improve quality, standardize workflows, accelerate decision making, and enhance communication in logistics, manufacturing, and maintenance operations throughout the supply chain. Of interest because: A trend in more universal, data-driven decision making is evolving just as leaps in hardware and software capability have led to smaller, more ergonomic devices. Could improve your supply chain by: Boosting labor effectiveness and productivity; reducing quality defects and rework; improving workflow standardization; enhancing workforce collaboration; improving safety. Why not? The technology is still rapidly evolving and has not yet reached operational maturity. Companies will have to understand how they will leverage data for critical use cases and should expect difficult integration challenges. Deloitte recommends: Evaluate the business case for smart glasses and augmented reality in your supply chain and pilot on a small number of critical use cases. -

A Review of Extended Reality (XR) Technologies for Manufacturing Training
technologies Article A Review of Extended Reality (XR) Technologies for Manufacturing Training Sanika Doolani * , Callen Wessels, Varun Kanal, Christos Sevastopoulos, Ashish Jaiswal and Harish Nambiappan and Fillia Makedon * Department of Computer Science and Engineering, The University of Texas at Arlington, Arlington, TX 76019, USA; [email protected] (C.W.); [email protected] (V.K.); [email protected] (C.S.); [email protected] (A.J.); [email protected] (H.N.) * Correspondence: [email protected] (S.D.); [email protected] (F.M.) Received: 30 October 2020; Accepted: 5 December 2020; Published: 10 December 2020 Abstract: Recently, the use of extended reality (XR) systems has been on the rise, to tackle various domains such as training, education, safety, etc. With the recent advances in augmented reality (AR), virtual reality (VR) and mixed reality (MR) technologies and ease of availability of high-end, commercially available hardware, the manufacturing industry has seen a rise in the use of advanced XR technologies to train its workforce. While several research publications exist on applications of XR in manufacturing training, a comprehensive review of recent works and applications is lacking to present a clear progress in using such advance technologies. To this end, we present a review of the current state-of-the-art of use of XR technologies in training personnel in the field of manufacturing. First, we put forth the need of XR in manufacturing. We then present several key application domains where XR is being currently applied, notably in maintenance training and in performing assembly task. -

X-Reality Museums: Unifying the Virtual and Real World Towards Realistic Virtual Museums
applied sciences Article X-Reality Museums: Unifying the Virtual and Real World Towards Realistic Virtual Museums George Margetis 1 , Konstantinos C. Apostolakis 1, Stavroula Ntoa 1, George Papagiannakis 1,2 and Constantine Stephanidis 1,2,* 1 Foundation for Research and Technology Hellas, Institute of Computer Science, N. Plastira 100, Vassilika Vouton, GR-700 13 Heraklion, Greece; [email protected] (G.M.); [email protected] (K.C.A.); [email protected] (S.N.); [email protected] (G.P.) 2 Department of Computer Science, University of Crete, GR-700 13 Heraklion, Greece * Correspondence: [email protected]; Tel.: +30-2810-391-741 Abstract: Culture is a field that is currently entering a revolutionary phase, no longer being a privilege for the few, but expanding to new audiences who are urged to not only passively consume cultural heritage content, but actually participate and assimilate it on their own. In this context, museums have already embraced new technologies as part of their exhibitions, many of them featuring augmented or virtual reality artifacts. The presented work proposes the synthesis of augmented, virtual and mixed reality technologies to provide unified X-Reality experiences in realistic virtual museums, engaging visitors in an interactive and seamless fusion of physical and virtual worlds that will feature virtual agents exhibiting naturalistic behavior. Visitors will be able to interact with the virtual agents, as they would with real world counterparts. The envisioned approach is expected to not only provide refined experiences for museum visitors, but also achieve high quality entertainment combined with more effective knowledge acquisition. Keywords: extended reality; diminished reality; true mediated reality; augmented reality; virtual reality; natural multimodal interaction; unified user experiences; interactive museum exhibits Citation: Margetis, G.; Apostolakis, K.C.; Ntoa, S.; Papagiannakis, G.; Stephanidis, C. -

Business Finland Neogames Fivr Mixed Reality Report 2017
MIXED REALITY REPORT 2017 BUSINESS FINLAND NEOGAMES FIVR 2 3 BUSINESS FINLAND | NEOGAMES BUSINESS FINLAND | NEOGAMES MIXED REALITY 2017 MIXED REALITY 2017 Content 1. Introduction 1. Introduction 3 lready from the 1990’s there has been a strong will and hope towards a virtual- and augmented reality based gaming experience. For a couple of 2. Terminology of VR, AR, MR and XR 3 decades, the development of technology was quite slow, but after HTC 3. Current Status of the VR/AR field 5 AVive, and the first Oculus consumer version release in March 2016 it seemed that 3.1 Available VR & AR devices and platforms for consumers 6 the technology is finally advanced enough, and the market for B2C VR applications, 3.1.1 High-end tethered VR headsets 6 including games, is ready to open. 3.1.2 Smartphone-based mobile VR headsets 7 The Oculus and Vive releases together with available VC funding and the 3.2 Technological demands in general 7 saturation of the mobile market (resulting in some mobile developers fleeing to 3.3 User expectations 8 VR/AR development) created high hopes towards VR. Basically everything required 4. Future - Towards casual VR 8 was coming together, funding, technology, skills and companies. However, after a 4.1 Four tiers of future VR devices 9 good start and excessive hype the VR games’ B2C market didn’t develop as expected. 4.2 High-end consumer VR devices 10 One clear indicator of that was that some existing VR studios have closed and even 5. AR Devices 10 Icelandic CCP, a big advocate of VR games since 2013, announced in the end of 6. -

Tobii Pro Glasses 2 Helmet Edition Product Description
Tobii Pro Glasses 2 Helmet Edition Product Description Head Unit (Firmware version 1.25.3) Recording Unit Prescription Lenses Controller Software Product Description Tobii Pro Glasses 2 Helmet Edition Version 1.0.1 08/2018 All rights reserved. Copyright © Tobii AB (publ) The information contained in this document is proprietary to Tobii AB. Any reproduction in part or whole without prior writ- ten authorization by Tobii AB is prohibited. Products that are referred to in this document may be either trademarks and/or registered trademarks of the respective owners. The publisher and the author make no claim to these trademarks. While every precaution has been taken in the preparation of this document, the publisher and the author assume no re- sponsibility for errors or omissions, or for damages resulting from the use of information contained in this document or from the use of programs and source code that may accom- pany it. In no event shall the publisher and the author be liable for any loss of profit or any other commercial damage caused or alleged to have been caused directly or indirectly by this document. Content subject to change without notice. Please check Tobii web site www.tobiipro.com for updated versions of this document. Table of Contents 1 Introduction.................................................................................................................................... 1 2 System Overview ..........................................................................................................................