Despite Vaccination, China Needs Non-Pharmaceutical Interventions To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Current and Future Natural Gas Demand in China and India
Global Gas/LNG Research Current and Future Natural Gas Demand in China and India By Miranda Wainberg Senior Energy Advisor Michelle Michot Foss, Ph.D. Chief Energy Economist and Program Manager Gürcan Gülen, Ph.D. Senior Energy Economist and Research Scientist Daniel Quijano Economist and Research Associate April 2017 April 2017, BEG/CEE China/India Gas Demand, Page 1 TABLE OF CONTENTS ESSENTIAL ACRONYMNS, UNITS AND CONVERSIONS ................................................................................................... 5 ACKNOWLEDGMENTS .................................................................................................................................................... 6 PREFACE ......................................................................................................................................................................... 7 INTRODUCTION ............................................................................................................................................................. 8 MACROECONOMIC CONTEXT FOR NATURAL GAS IN CHINA AND INDIA ...................................................................... 9 Composition of GDP and Employment Structure ...................................................................................................... 9 GDP Growth and Industrial Structures in China and India ...................................................................................... 11 Industrial overcapacity and debt in China ......................................................................................................... -

Occupational Characteristics and Management Measures of Sporadic
Occupational characteristics and management measures of sporadic COVID-19 outbreaks from June 2020 to January 2021 in China: the importance of tracking down “patient zero” Maohui Feng 1,a, Qiong Ling 2,a, Jun Xiong 3, Anne Manyande 4, Weiguo Xu 5, Boqi Xiang 6,* 1 Department of Gastrointestinal Surgery, Wuhan Peritoneal Cancer Clinical Medical Research Center, Zhongnan Hospital of Wuhan University, Hubei Key Laboratory of Tumor Biological Behaviors and Hubei Cancer Clinical Study Center, Wuhan 430071, Hubei, PR China; 2 Department of Anesthesiology, The Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510120, Guangdong, PR China; 3 Hepatobiliary Surgery Center, Union Hospital of Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430022, PR China; 4 School of Human and Social Sciences, University of West London, London, United Kingdom; 5 Department of Orthopedics, Tongji Hospital of Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430030, PR China; 6 School of Public Health, University of Rutgers, New Brunswick, NJ 08854, USA. a These authors have contributed equally to this work. *Correspondence: Boqi Xiang, E-mail: [email protected] Abstract There are occupational disparities in the risk of contracting COVID-19. Occupational characteristics and work addresses play key roles in tracking down “patient zero”. The present descriptive analysis for occupational characteristics and management measures of sporadic COVID-19 outbreaks from June to December 2020 in China offers important new information to the international community at this stage of the pandemic. These data suggest that Chinese measures including tracking down “patient zero”, launching mass COVID-19 testing in the SARS-CoV-2-positive areas, designating a new high or medium-risk area, locking down the corresponding community or neighborhood in response to new COVID-19 cases and basing individual methods of protection on science, are effective in reducing transmission of the highly contagious SARS-CoV-2 across China. -

Innovent Biologics (1801
22 Jul 2021 CMB International Securities | Equity Research | Company Initiation Innovent Biologics (1801 HK) BUY (Initiation) Growing into a global biopharma company Target Price HK$120.91 Up/Downside +43.00% Current Price HK$84.55 Rich innovative drug pipelines. Innovent is a leading integrated biopharma company with comprehensive innovative pipelines including monoclonal antibodies (mAbs), bispecific antibodies (bsAbs), small molecules and CAR- China Healthcare Sector T therapies, covering oncology, autoimmune and metabolic diseases. Besides five marketed products (sintilimab, three biosimilars and pemigatinib), Jill Wu, CFA Innovent has six innovative drugs in pivotal clinical stage, including IBI306 (852) 3900 0842 (PCSK9 antibody), IBI310 (CTLA-4 antibody), IBI376 (PI3Kδ inhibitor), IBI326 [email protected] (BCMA-CART), taletrectinib (ROS1/NTRK inhibitor) and HQP1351 (olverembatinib, third-generation BCR-ABL TKI). In addition, Innovent has Sam Hu, PhD established a comprehensive innovative portfolio covering next-generation (852) 3900 0882 immuno-oncology (I/O) targets, including CD47/SIRPα, TIGT, LAG3, 4-1BB, [email protected] etc. It’s worth noting that Innovent is an early mover in CD47-SIRPα pathway with three assets under development, including clinical-stage IBI188 (a CD47 Jonathan Zhao antibody) and IBI322 (a PD-L1/CD47 bispecific antibody), and preclinical (852) 6359 1614 stage IBI397 (AL008, a SIRPα antibody). [email protected] Tyvyt being an early mover in large indications. After the approval for r/r- cHL in Dec 2018, Tyvyt has been approved by the NMPA for 1L ns-NSCLC, Mkt. Cap. (HK$ mn) 123,312 1L s-NSCLC and 1L HCC in 2021. These three large indications may be Avg. -
Emergence of Highly Infectious SARS-Cov-2 Variants in Bangladesh
Hasan et al. Trop Med Health (2021) 49:69 https://doi.org/10.1186/s41182-021-00360-w Tropical Medicine and Health LETTER TO THE EDITOR Open Access Emergence of highly infectious SARS-CoV-2 variants in Bangladesh: the need for systematic genetic surveillance as a public health strategy Mohammad Mehedi Hasan1,2, Ian Christopher N. Rocha3, Kimberly G. Ramos3, Trisha Denise D. Cedeño3, Ana Carla dos Santos Costa4, Christos Tsagkaris5, Md. Masum Billah6, Shoaib Ahmad7 and Mohammad Yasir Essar8* Abstract Bangladesh, a low-middle-income country in South Asia is facing one of its worst public health emergencies due to the COVID-19 pandemic. The increase in the number of cases from the disease, since the second half of March 2021, can potentially cause the health system overload, and has, as one of the main reasons, the non-compliance with measures of social distance and the emergence of the variants of concern in the country. This increase in the contagion curve can also provide a favorable environment for the occurrence of more mutations in the structure and genome of the virus. Therefore, there is an urge to carry out genomic surveillance programs in order to identify, moni- tor and characterize these variants, and understand whether the vaccines currently used are efective against them. Keywords: Bangladesh, SARS-CoV-2 variants, Public health, Genetic surveillance Dear editor, in the country began to increase during the middle of Te ongoing Coronavirus Disease 2019 (COVID-19) March 2021. Initially, there was a drop in the number of pandemic is a major burden to health systems world- cases during February 2021, in which the lowest monthly wide, constituting the worst health crisis in history. -

Medical JOUR
RHODE ISLAND M EDiCAL J ournal ZOOM – It’s a Match! Virtual National Match Day is largest on record See page 75 R SPECIAL SECTION, PART II BIOMEDICAL/TRANSLATIONAL RESEARCH in RI GUEST EDITORS: JAMES PADBURY, MD; BONGSUP CHO, PhD ApRiL 2021 VOLUME 104 • NUMBER 3 iSSN 2327-2228 REINVENTING WHAT YOU EXPECT FROM A MEDICAL PROFESSIONAL LIABILITY PROVIDER. With Coverys, you can reduce the distractions that come between diagnosis and outcomes. By leveraging claims data and analytics plus innovative educational resources, we’re helping doctors and administrators reduce distractions and focus on improving clinical, operational, and financial outcomes.Visit coverys.com Insurance products issued by ProSelect® Insurance Company (NE, NAIC 10638) and Preferred Professional Insurance Company® (NE, NAIC 36234). RHODE ISLAND M EDICAL J OURNAL 15 Translational Research: The Time is Now JAMES F. PADBURY, MD BONGSUP P. CHO, PhD GUEST EDITORS James F. Padbury, MD Bongsup Cho, PhD 17 The Time is NOW: Filling the Gaps in Treatment of Opioid-Exposed Infants: A Prospective, Pragmatic, Randomized Control Drug Trial ADAM J. CZYNSKI, DO; ABBOT R. LAPTOOK, MD 22 COBRE on Opioid and Overdose: A Collaborative Research-Based Center Addressing the Crises in Rhode Island and Beyond TRACI C. GREEN, PhD, MSc; ELIANA KAPLOWITZ, BA; KIRSTEN LANGDON, PhD; JACLYN M.W. HUGHTO, PhD, MPH; WILLIAM C. GOEDEL, PhD; ADAM J. CZYNSKI, DO; GAYLE FRASER, BS; JOSIAH RICH, MD, MPH 27 Brown University COBRE Center for Addiction and Disease Risk Exacerbation PETER M. MONTI, PhD; JENNIFER W. TIDEY, PhD; JASJIT S. AHLUWALIA, MD 32 The Center of Biomedical Research Excellence (COBRE) for Perinatal Biology – Accomplishments, Impact, and Long-term Results SUNIL K. -
Assessing SARS-Cov-2 Circulation, Variants of Concern, Non-Pharmaceutical Interventions and Vaccine Rollout in the EU/EEA, 15Th Update 10 June 2021
RISK ASSESSMENT Assessing SARS-CoV-2 circulation, variants of concern, non-pharmaceutical interventions and vaccine rollout in the EU/EEA, 15th update 10 June 2021 Summary Although SARS-CoV-2 transmission remains widespread in large parts of the EU/EEA, most countries report declining trends in 14-day COVID-19 notification rates, hospital and intensive care unit (ICU) occupancy, and mortality. Many countries have initiated partial lifting of different non-pharmaceutical interventions (NPIs) that aim to reduce the degree of citizens physical contact and mobility. Since January 2021, EU/EEA countries have reported an increase in the number and proportion of SARS-CoV-2 cases of variants of concern (VOC) associated with increasing transmissibility and/or severity, with Alpha (B.1.1.7) the current dominant variant across the EU/EEA. Estimates across the region show that a large proportion of the population across Europe still remains susceptible to SARS-CoV-2 and that population immunity is far from being reached. As of 3 June, the median cumulative vaccine uptake in the EU/EEA adult population (aged 18 years and older) had reached 46.2% for at least one vaccine dose and 22.3% for the full vaccination course. The highest level of vaccine uptake was observed among the elderly aged over 80, in which the uptake reached 80.5% for at least one dose and 66.3% for full vaccination coverage. For healthcare workers, the median level of at least one dose uptake was 87% and the median uptake for the full vaccination course was 65.2%. Increased vaccine supply has allowed countries to expand eligibility for vaccination to younger age groups. -

Doctors' Mental Health in the Midst of COVID-19 Pandemic
International Journal of Environmental Research and Public Health Article Doctors’ Mental Health in the Midst of COVID-19 Pandemic: The Roles of Work Demands and Recovery Experiences 1,2, 1, , 3 Mohd Fadhli Mohd Fauzi y , Hanizah Mohd Yusoff * y, Rosnawati Muhamad Robat , Nur Adibah Mat Saruan 1,2 , Khairil Idham Ismail 1,2 and Ahmad Firdaus Mohd Haris 4 1 Department of Community Health, Faculty of Medicine, Universiti Kebangsaan Malaysia, Jalan Yaacob Latiff, Bandar Tun Razak, Cheras, Kuala Lumpur 56000, Malaysia; [email protected] (M.F.M.F.); [email protected] (N.A.M.S.); [email protected] (K.I.I.) 2 Ministry of Health Malaysia, Federal Government Administrative Centre, Putrajaya 62590, Malaysia 3 Occupational and Environmental Health Unit, Selangor State Health Department, No 1, Wisma Sunway, Jalan Tengku Ampuan Zabedah C 9/C, Seksyen 9, Shah Alam, Selangor 40100, Malaysia; [email protected] 4 Non-Communicable Diseases Unit, Perak State Health Department, Jalan Koo Chong Kong, Ipoh 30000, Perak, Malaysia; ahmad.fi[email protected] * Correspondence: [email protected]; Tel.: +60-3-9145-5904 These authors contributed equally to this work. y Received: 18 September 2020; Accepted: 5 October 2020; Published: 8 October 2020 Abstract: The COVID-19 pandemic potentially increases doctors’ work demands and limits their recovery opportunity; this consequently puts them at a high risk of adverse mental health impacts. This study aims to estimate the level of doctors’ fatigue, recovery, depression, anxiety, and stress, and exploring their association with work demands and recovery experiences. This was a cross-sectional study among all medical doctors working at all government health facilities in Selangor, Malaysia. -

Social Distancing and Supply Disruptions in a Pandemic∗
Social Distancing and Supply Disruptions in a Pandemic∗ Martin Bodenstein Giancarlo Corsetti Luca Guerrieri Federal Reserve Board University of Cambridge Federal Reserve Board June 18, 2020 Abstract Drastic public health measures such as social distancing or lockdowns can reduce the loss of human life by keeping the number of infected individuals from exceeding the capacity of the health care system but are often criticized because of the social and economic costs they entail. We question this view by combining an epidemiological model, calibrated to capture the spread of the COVID-19 virus, with a multisector model, designed to capture key characteristics of the U.S. Input Output Tables. Our two-sector model features a core sector that produces intermediate inputs not easily replaced by inputs from the other sector, subject to minimum-scale requirements. We show that, by affecting workers in this core sector, the high peak of an infection not mitigated by social distancing may cause very large upfront economic costs in terms of output, consumption and investment. Social distancing measures can reduce these costs, especially if skewed towards non-core industries and occupations with tasks that can be performed from home, helping to smooth the surge in infections among workers in the core sector. JEL classifications: E1, E3, I1. Keywords: infectious disease, epidemic, recession, COVID-19. ∗ The views expressed in this paper are solely the responsibility of the authors and should not be interpreted as reflecting the views of the Board of Governors of the Federal Reserve System or of any other person associated with the Federal Reserve System. -

World Energy Investment 2021 INTERNATIONAL ENERGY AGENCY
World Energy Investment 2021 INTERNATIONAL ENERGY AGENCY The IEA examines the IEA member IEA association full spectrum countries: countries: of energy issues including oil, gas and Australia Brazil coal supply and Austria China demand, renewable Belgium India energy technologies, electricity markets, Canada Indonesia energy efficiency, Czech Republic Morocco access to energy, Denmark Singapore demand side Estonia South Africa management and Finland Thailand much more. Through France its work, the IEA Germany advocates policies that Greece will enhance the Hungary reliability, affordability Ireland and sustainability of Italy energy in its 30 member countries, Japan 8 association countries Korea and beyond. Luxembourg Mexico Netherlands New Zealand Norway Poland Portugal Please note that this Slovak Republic publication is subject to Spain specific restrictions that limit its use and distribution. The Sweden terms and conditions are Switzerland available online at Turkey www.iea.org/t&c/ United Kingdom United States This publication and any map included herein are The European without prejudice to the Commission also status of or sovereignty over participates in the any territory, to the delimitation of international work of the IEA frontiers and boundaries and to the name of any territory, city or area. Source: IEA. All rights reserved. International Energy Agency Website: www.iea.org World Energy Investment 2021 Abstract Abstract This year’s edition of the World Energy Investment report presents the latest data and analysis of how energy investment flows are recovering from the shock of the Covid-19 pandemic, including full-year estimates of the outlook for 2021. It examines how investors are assessing risks and opportunities across all areas of fuel and electricity supply, efficiency and research and development, against a backdrop of a recovery in global energy demand as well as strengthened pledges from governments and the private sector to address climate change. -

Global Offering
蘇州貝康醫療股份有限公司 SUZHOU BASECARE MEDICAL CORPORATION LIMITED (A joint stock company incorporated in the People's Republic of China with limited liability) Stock Code: 2170 GLOBAL OFFERING Sole Sponsor, Joint Global Coordinator, Joint Bookrunner and Joint Lead Manager Joint Global Coordinators, Joint Bookrunners and Joint Lead Managers Joint Bookrunners and Joint Lead Managers Joint Lead Manager IMPORTANT IMPORTANT: If you are in any doubt about any of the contents of this prospectus, you should seek independent professional advice. Suzhou Basecare Medical Corporation Limited 蘇州貝康醫療股份有限公司 (A joint stock company incorporated in the People’s Republic of China with limited liability) GLOBAL OFFERING Number of Offer Shares under : 66,667,000 H Shares (subject to the the Global Offering Over-allotment Option) Number of Hong Kong Offer Shares : 6,667,000 H Shares (subject to adjustment) Number of International Offer Shares : 60,000,000 H Shares (subject to adjustment and the Over-allotment Option) Maximum Offer Price : HK$27.36 per H Share, plus brokerage of 1.0%, SFC transaction levy of 0.0027% and Stock Exchange trading fee of 0.005% (payable in full on application in Hong Kong Dollars and subject to refund) Nominal Value : RMB1.00 per H Share Stock Code : 2170 Sole Sponsor, Joint Global Coordinator, Joint Bookrunner and Joint Lead Manager Joint Global Coordinators, Joint Bookrunners and Joint Lead Managers Joint Bookrunners and Joint Lead Managers Joint Lead Manager Hong Kong Exchanges and Clearing Limited, The Stock Exchange of Hong Kong Limited and Hong Kong Securities Clearing Company Limited take no responsibility for the contents of this prospectus, make no representation as to its accuracy or completeness, and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this prospectus. -

IHP News 610 : Perseverance
IHP news 610 : Perseverance ( 26 Feb 2021) The weekly International Health Policies (IHP) newsletter is an initiative of the Health Policy unit at the Institute of Tropical Medicine in Antwerp, Belgium. Dear Colleagues, When the first vaccine doses distributed by COVAX landed in Ghana earlier this week, it felt a bit like the Perseverance’s landing on Mars. Ouf! At last. Neil Armstrong probably also nodded approvingly from heaven, when hearing some of the rhetoric: “Wonderful words from @UNICEF Covax Coordinator Gian Gandhi as the first ACTA flight hits the ground in Ghana: « A short flight, and small step to reduce inequities in vaccine access... but a huge achievement that’s been almost 10 months in the making». Anyway, encouraging and great news, not a day too soon. Still, the picture on global vaccine equity remains bleak in the short term, for the reasons you know. Yes, there is a growing movement behind vaccine equity, as dr. Tedros claimed last week, and multilateralism made a cautious comeback at the G7 summit (with Covax getting a (much needed) shot in the arm). WHO officials can now be (a bit) more optimistic about successfully getting around 2 billion vaccine doses to at least 20% of the populations of 92 lower-income economies by the end of 2021. But they shouldn’t get carried away too soon, as this (excellent) COVAX “state of affairs” piece in Stat argued: “more is needed to ensure global vaccine access”. A quote from Kenneth Shadlen put things in perspective: “It would be great if COVAX can help us avoid a worst-case scenario of poor countries having no vaccines until 2022 or later. -
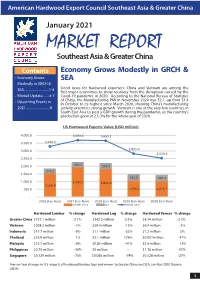
AHEC Market Report
American Hardwood Export Council Southeast Asia & Greater China January 2021 MARKET REPORT Southeast Asia & Greater China Contents Economy Grows Modestly in GRCH & • Economy Grows SEA Modestly in GRCH & SEA..............................1-4 Good news for hardwood exporters: China and Vietnam are among the first major economies to show recovery from the disruption caused by the • Market Update........4-7 Covid-19 pandemic in 2020. According to the National Bureau of Statistics • Upcoming Events in of China, the Manufacturing PMI in November 2020 was 52.1, up from 51.4 in October to its highest since March 2020, showing China’s manufacturing 2021.............................8 activity extend its strong growth. Vietnam is one of the very few countries in South East Asia to post a GDP growth during the pandemic, as the country’s production grew at 2.5-3% for the whole year of 2020. US Hardwood Exports Value (USD million) 4,000.0 3,693.6 3,665.1 3,500.0 3,290.3 2,825.0 3,000.0 2,528.6 2,500.0 2,000.0 304.5 341.4 272.2 1,500.0 361.6 342.3 1,000.0 1,949.2 1,841.6 1,556.8 500.0 1,096.4 1,076.7 - 2016 (Jan-Nov) 2017 (Jan-Nov) 2018 (Jan-Nov) 2019 (Jan-Nov) 2020 (Jan-Nov) Greater China SEA World Total Hardwood Lumber % change Hardwood Log % change Hardwood Veneer % change Greater China $727.1 million -2.7% $342.2 million 0.3% $4.74 million -2.7% Vietnam $208.3 million -1% $59.4 million -15% $6.4 million -3% Indonesia $17.7 million -9% $1.1 million -53% $7.2 million 5% Thailand $15.9 million 1% $2.1 million 179% $0.057million 47% Malaysia $13.7 million -6% $0.83 million -41% $5.6 million 12% Philippines $0.75 million -36% $0 million -- $1.16 million -33% Singapore $0.129 million -75% $0.065 million -74% $0.328 million -27% Year-on-Year changes in U.S.