Suprascapular Nerve Entrapment: Technique for Arthroscopic Release
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Suprascapular Nerve Lesions at the Spinoglenoid Notch: Report of Three Cases and Review of the Literature 243
Journal ofNeurology, Neurosurgery, and Psychiatry 1991;54:241-243 241 Suprascapular nerve lesions at the spinoglenoid J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.54.3.241 on 1 March 1991. Downloaded from notch: report of three cases and review of the literature Jay A Liveson, Michael J Bronson, Michael A Pollack Abstract of root involvement (cervical pain, and change Lesions of the suprascapular nerve can from Valsalva's manoeuvre). His past medical occur at the supraspinatus notch (SSN) history was negative. On physical examination or at the spinoglenoid notch (SGN). Elec- cranial nerves were normal. No weakness was tromyographic (EMG), evaluation of the detected on careful manual muscle examin- infraspinatus, and especially the supra- ation. Sensation was intact. Deep tendon spinatus muscles distinguishes SGN reflexes were active and symmetrical with no from SSN lesions. Three cases of SGN pathological reflexes. There was no Homer's lesions, which are more common than sign. SSN lesions, are presented. The patient gave up weight lifting and started a programme of physiotherapy. His shoulder ache resolved rapidly, but his muscle Entrapment of the suprascapular nerve at the bulk did not return to normal for another 12 suprascapular notch (SSN) was first described months. He reported completely normal func- in 1963 by Kopell and Thompson.' No alter- tion. native entrapment site was recognised until 1981 when the first case of spinoglenoid notch Case 2 (SGN) entrapmnt was described by Ganzhorn A 22 year old right handed male was skeet et al.2 Since then nine additional cases of SGN shooting, a month before his examination. -

Arthroscopic Decompression of the Suprascapular Nerve at the Spinoglenoid Notch and Suprascapular Notch Through the Subacromial Space
Technical Note Arthroscopic Decompression of the Suprascapular Nerve at the Spinoglenoid Notch and Suprascapular Notch Through the Subacromial Space Neil Ghodadra, M.D., Shane J. Nho, M.D., M.S., Nikhil N. Verma, M.D., Stefanie Reiff, B.A., Dana P. Piasecki, M.D., Matthew T. Provencher, M.D., and Anthony A. Romeo, M.D. Abstract: Suprascapular nerve entrapment can cause disabling shoulder pain. Suprascapular nerve release is often performed for compression neuropathy and to release pressure on the nerve associated with arthroscopic labral repair. This report describes a novel all-arthroscopic technique for decom- pression of the suprascapular nerve at the suprascapular notch or spinoglenoid notch through a subacromial approach. Through the subacromial space, spinoglenoid notch cysts can be visualized between the supraspinatus and infraspinatus at the base of the scapular spine. While viewing the subacromial space through the lateral portal, the surgeon can use a shaver through the posterior portal to decompress a spinoglenoid notch cyst at the base of the scapular spine. To decompress the suprascapular nerve at the suprascapular notch, a shaver through the posterior portal removes the soft tissue on the acromion and distal clavicle to expose the coracoclavicular ligaments. The medial border of the conoid ligament is identified and followed to its coracoid attachment. The supraspinatus muscle is retracted with a blunt trocar placed through an accessory Neviaser portal. The transverse scapular ligament, which courses inferior to the suprascapular artery, is sectioned with arthroscopic scissors, and the suprascapular nerve is decompressed. Key Words: Arthroscopy—Suprascapular nerve—Transverse scapular ligament—Suprascapular notch—Rotator cuff—Shoulder. -

Bone Limb Upper
Shoulder Pectoral girdle (shoulder girdle) Scapula Acromioclavicular joint proximal end of Humerus Clavicle Sternoclavicular joint Bone: Upper limb - 1 Scapula Coracoid proc. 3 angles Superior Inferior Lateral 3 borders Lateral angle Medial Lateral Superior 2 surfaces 3 processes Posterior view: Acromion Right Scapula Spine Coracoid Bone: Upper limb - 2 Scapula 2 surfaces: Costal (Anterior), Posterior Posterior view: Costal (Anterior) view: Right Scapula Right Scapula Bone: Upper limb - 3 Scapula Glenoid cavity: Glenohumeral joint Lateral view: Infraglenoid tubercle Right Scapula Supraglenoid tubercle posterior anterior Bone: Upper limb - 4 Scapula Supraglenoid tubercle: long head of biceps Anterior view: brachii Right Scapula Bone: Upper limb - 5 Scapula Infraglenoid tubercle: long head of triceps brachii Anterior view: Right Scapula (with biceps brachii removed) Bone: Upper limb - 6 Posterior surface of Scapula, Right Acromion; Spine; Spinoglenoid notch Suprspinatous fossa, Infraspinatous fossa Bone: Upper limb - 7 Costal (Anterior) surface of Scapula, Right Subscapular fossa: Shallow concave surface for subscapularis Bone: Upper limb - 8 Superior border Coracoid process Suprascapular notch Suprascapular nerve Posterior view: Right Scapula Bone: Upper limb - 9 Acromial Clavicle end Sternal end S-shaped Acromial end: smaller, oval facet Sternal end: larger,quadrangular facet, with manubrium, 1st rib Conoid tubercle Trapezoid line Right Clavicle Bone: Upper limb - 10 Clavicle Conoid tubercle: inferior -
Suprascapular Nerve Entrapment Isolated to the Spinoglenoid Notch: Surgical Technique and Results of Open Decompression
J Shoulder Elbow Surg (2013) 22, e1-e8 www.elsevier.com/locate/ymse Suprascapular nerve entrapment isolated to the spinoglenoid notch: surgical technique and results of open decompression Nathan A. Mall, MD*, James E. Hammond, DO, Brett A. Lenart, MD, Daniel J. Enriquez, MA, Stacy L. Twigg, PA-C, Gregory P. Nicholson, MD Department of Orthopaedic Surgery, Division of Sports Medicine and Shoulder and Elbow Surgery, Rush University Medical Center, St Louis, MO, USA Background: Entrapment of the suprascapular nerve (SSN) at the spinoglenoid notch (SGN) specifically affects the infraspinatus, and isolated external rotation (ER) weakness can result. We describe the tech- nique of open SSN decompression at the SGN for infraspinatus involvement and report the results of a consecutive series. Materials and methods: Twenty-nine shoulders underwent SSN decompression at the SGN. The mean age was 44 years (range, 15-69 years), and the mean follow-up was 4.3 years (range, 1-7 years). On manual muscle testing, ER strength was abnormal in all patients: 2/5 in 3, 3/5 in 21, and 4/5 in 5. The mean preop- erative American Shoulder and Elbow Surgeons (ASES) score was 48 (range, 23-83). Atrophy of the infra- spinatus was visible or palpable in 72% of shoulders. Magnetic resonance imaging showed ganglion cysts at the SGN in only 20.7% of shoulders. Results: Of the patients, 19 (66%) regained full ER strength, 9 (31%) improved to 4/5, and 1 (3%) had ER strength of 3/5. The mean ASES score improved to 75 (range, 60-100) (P < .05). -

Classification of the Superior Angle of the Scapula and Its Correlation with the Suprascapular Notch: a Study on 303 Scapulas
Surgical and Radiologic Anatomy (2019) 41:377–383 https://doi.org/10.1007/s00276-018-2156-4 ORIGINAL ARTICLE Classification of the superior angle of the scapula and its correlation with the suprascapular notch: a study on 303 scapulas Lei Zhang1,2 · Xiaoguang Guo1,2 · Yang Liu1,2 · Min Ou1,2 · Xiaoyan Lin1,2 · Ji Qi3 · Yanxiao Xu3 · Guoyou Wang1,2 · Shijie Fu1,2 Received: 10 October 2018 / Accepted: 7 December 2018 / Published online: 15 December 2018 © Springer-Verlag France SAS, part of Springer Nature 2018 Abstract Purpose The aims of this study had been to classify the superior angle of the scapula based on morphological features, and to investigate its correlation with the suprascapular notch. Methods 303 samples of Chinese dried scapular specimens were collected from the Department of anatomy, Southwest Medical University. According to the anatomical morphological characteristics of the superior angle of the scapula, the morphological classification was performed to explore its correlation with the suprascapular notch (SSN). Results The superior angle of the scapula was classified into three types (Hilly shape, Mountain Peak shape and Chimney shape). There were 143 cases of Hilly shape (47.20%), 144 cases of Mountain shape (47.52%), and 16 cases of Chimney shape (5.28%). The angle of Hilly shape (93.36° ± 7.76°) was significantly larger than the Mountain Peak shape (86.60° ± 6.61°) and the Chimney shape (86.22° ± 7.20°), and the difference was statistically significant (P < 0.05). The type I–III of Rengachary’s classification to SSN was low risk of suprascapular nerve entrapment, while the type IV–VI was high risk of suprascapular nerve entrapment. -

Morphology of Suprascapular Notch of Scapula and Its Clinical Implications
JK SCIENCE ORIGINALARTICLE Morphology of Suprascapular Notch of Scapula and its Clinical Implications Manmeet Kour, Sangeeta Gupta Abstract Morphology of suprascapular notch was studied in a tertiary care teaching hospital of North India on sixty dry adult human scapula of unknown sex. Firstly it was determined, whether the suprascapular notch was present or not. Then the shape of the suprascapular notch was noted i.e. whether it was 'U' shaped, 'V' shaped, 'J' shaped ,or round in the form of Foramen. The foramen is formed due to complete ossification of the superior transverse scapular ligament.The suprascapular nerve passes through it, and in some cases anterior coracoscapular ligament was also found.The study of morphology of suprascapular notch is important as suprascapular nerve entrapment is a common entity which leads to wastage of muscles supplied by it i.e. supraspinatus and infraspinatus.The knowledge of suprascapular notch variations is of importance for surgeons performing suprascapular nerve decompression, especially by means of endoscopic techniques. Key Words Morphometry, Scapula, Suprascapular Notch, Suprascapular Nerve Introduction The scapula of man is one of the interesting bones of shaped or "O" shaped (i.e. as a complete his skeleton. It presents numerous features and foramen).Different authors have classified the dimensions, which are easy to systematically examine suprascapular notch into different types. Authors like and measure, when in good condition, and it also presents Olivier (3) has divided it into 5 types and authors like many variations (1, 2). Scapula has three borders viz; Rengachary (4) has divided into 6 types. In all these types superior, medial and lateral border. -
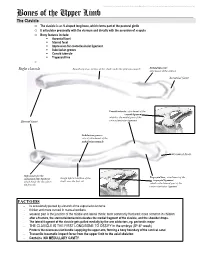
Bones of the Upper Limb
This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. Bones of the Upper Limb The Clavicle o The clavicle is an S-shaped long bone, which forms part of the pectoral girdle o It articulates proximally with the sternum and distally with the acromion of scapula o Bony features include: . Acromial facet . Sternal facet . Impression for costoclavicular ligament . Subclavian groove . Conoid tubercle . Trapezoid line o Right clavicle Smooth superior surface of the shaft, under the platysma muscle Deltoid tubercle: attachment of the deltoid Acromial facet Conoid tubercle, attachment of the conoid ligament which is the medial part of the Sternal facet coracoclavicular ligament Subclavian groove: site of attachment of the subclavius muscle Acromial facet Impression for the Trapezoid line, attachment of the costoclavicular ligament Rough inferior surface of the trapezoid ligament which binds the clavicle to shaft, over the first rib which is the lateral part of the the first rib coracoclavicular ligament FACTOIDS - Its occasionally pierced by a branch of the supraclavicular nerve - thicker and more curved in manual workers - weakest part is the junction of the middle and lateral thirds: most commonly fractured; more common in children - after a fracture, the sternocleidomastoid elevates the medial fragment of the clavicle, and the shoulder drops. - The lateral fragment of the clavicle gets pulled medially by the arm adductors, eg. pectoralis major - THE CLAVICLE IS THE FIRST LONG BONE TO OSSIFY in the embryo (5th-6th week) - Protects the neurovascular bundle supplying the upper arm, forming a bony boundary of the cervical canal - Transmits traumatic impact force from the upper limb to the axial skeleton - Contains NO MEDULLARY CAVITY - This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. -

Morphometric Study of Suprascapular Notch As A
International Journal of Anatomy and Research, Int J Anat Res 2017, Vol 5(2.3):4015-19. ISSN 2321-4287 Original Research Article DOI: https://dx.doi.org/10.16965/ijar.2017.243 MORPHOMETRIC STUDY OF SUPRASCAPULAR NOTCH AS A FACTOR OF SUPRASCAPULAR NERVE ENTRAPMENT AND DIMEN- SIONS OF SAFE ZONE TO PREVENT SUPRASCAPULAR NERVE INJURY Nutan Nalini Bage *1, Sriambika K 2, Magi Murugan 3, Virender Kumar Nim 4 *1 Professor, Department of Anatomy Pondicherry Institute of Medical Sciences, Ganapathychettikulam, Kalapet, Pondicherry, India. 2 Tutor, Department of Anatomy, Pondicherry Institute of Medical Sciences, Ganapathychettikulam, Kalapet, Pondicherry, India. 3 Associate Professor, Department of Anatomy, Pondicherry Institute of Medical Sciences, Ganapathychettikulam, Kalapet, Pondicherry, India. 4 Professor and Head, Department of Anatomy, Pondicherry Institute of Medical Sciences, Ganapathychettikulam, Kalapet, Pondicherry, India. ABSTRACT Background: The scapula is a large, flat, triangular bone which lies on the postero-lateral aspect of the chest wall Suprascapular nerve entrapment depends on the size and shape of suprascapular notch. Purpose of the study: Aim of the present study is to classify SSN based on morphometry according to Michal Polguj and to obtain a safe zone which would be useful to avoid iatrogenic nerve lesion and to verify the reliability of the existing data for the management of entrapment neuropathy. Materials and Methods: Study included 60 dried human scapulae obtained from the Department of Anatomy, Pondicherry institute of medical sciences. Three measurements were defined and collected for each SSN, Maximum depth (MD), Superior transverse diameter (STD) and Middle transverse diameters (MTD) based on which suprascapular notch was classified. -

Arthroscopic Release of Suprascapular Nerve Entrapment at the Suprascapular Notch: Technique and Preliminary Results
Arthroscopic Release of Suprascapular Nerve Entrapment at the Suprascapular Notch: Technique and Preliminary Results Laurent Lafosse, M.D., Andrea Tomasi, M.D., Steve Corbett, M.D., Gloria Baier, M.D., Karel Willems, M.D., and Reuben Gobezie, M.D. Purpose: We describe a novel all-arthroscopic technique for suprascapular nerve (SSN) decompres- sion and present our preliminary results for this procedure. Methods: A prospective series of 10 patients with preoperative electromyographic findings consistent with chronic SSN compression, posterior shoulder pain, and subjective weakness were treated with arthroscopic SSN decompression. There were 8 men and 2 women, with a mean age of 50 years. The mean follow-up was 15 months (range, 6 to 27 months). In 8 of 10 patients, we performed an electromyographic examination postoperatively to evaluate nerve recovery after decompression. The clinical outcomes measures used to assess preoperative and postoperative function were the visual analog scale for pain, the Constant score, strength testing of the supraspinatus and infraspinatus, and a subjective satisfaction question- naire. In all patients preoperative and postoperative computed tomography arthrograms were ob- tained to document the absence of a rotator cuff tear. Results: There were no complications resulting from SSN decompression. Of 10 patients, 8 had postoperative electromyography at a mean of 6 months after SSN release and 2 refused to undergo this study after surgery. Of the 8 postoperative electromyograms, 7 had complete normalization of the latency in the motor fibers of the SSN and normalization of the voluntary motor action potential for the supraspinatus and infraspinatus muscles. Two of the electromyograms showed evidence of partial recovery. -

Honeymoon Palsy and Other Upper Extremity Entrapment Neuropathies
Honeymoon Palsy and other upper extremity Entrapment Neuropathies Michael Wilensky M.D. Senior Neurologist Ochsner Metairie Clinic Less commonly recognized upper extremity neuropathies • Radial motor neuropathy -Saturday night palsy; honeymoon palsy • Suprascapular neuropathy-gymnast; volleyball servers • Dorsal scapular neuropathy –weight lifters • Pronator syndrome – oyster shuckers • Anterior interosseous syndrome- post op; premarital palsy; new mom • Deep palmer ulnar motor neuropathy- bikers; jewelers • Radial sensory neuropathy –hand cuff ; zip ties; CTS splint HONEYMOON PALSY DIFFERENTIATE FROM HONEYMOON SYNDROME – CYSTITIS FROM FIRST TIME OR FREQUENT SEX ON HONEYMOON SATURDAY NIGHT PALSY Radial motor Neuropathy • DRUNK AND FALLING ASLEEP IN UNUSUAL POSITION WITH PRESSURE ON UPPER ARM. • ONE ARM HANGING OVER THE BACK OF CHAIR AT THE BAR Radial motor neuropathy • Clinical weakness in extensor muscles of forearm • Weakness of finger extensors and wrist extensors • Presents as wrist drop • Important to examine finger flexors with wrist supported HONEYMOON PALSY • PRESSURE ON UPPER ARM FROM HEAD LYING ON ARM Suprascapular Neuropathy • ENTRAPMENT @SUPRASCAPULAR NOTCH • SHOULDER DEEP THROBBING PAIN-OCCASIONALLY DOWN ARM • SUPRASPINATUS-WEAKNESS SHOULDER ABDUCTION INITIAL 30 DEGREE • INFRASPINATUS –WEAKNESS SHOULDER EXTERNAL ROTATION • CAUSE –REPETITIVE FORCED ADDUCTION • GYMNASTS,WEIGHT LIFTERS,VOLLEYBALL SERVERS,SWIMMERS Suprascapular Neuropathy DIAGNOSIS & TREATMENT • EMG SHOWS DENERVATION IN SUPRASINATUS AND INFRASPINATUS TX • IDENTIFY PROBLEM • AVOID CAUSATIVE ACTIVITY • NSAID • POSSIBLE SURGICAL DECOMPRESSION DORSAL SCAPULAR ANATOMY shoulder and arm pain, DORSAL SCAPULAR NEUROPATHY • Pain over the medial border of the scapula. • Patients may also experience interscapular pain, weakness of arm abduction, and/or winged scapula. • Sharp, stabbing, burning, or knife-like medial scapular pain, lateral arm and forearm pain, neck and back dull ache, • Rhomboid or levator atrophy. -

Posterior Shoulder Pain and Arthroscopic Decompression of the Suprascapular Nerve
Sports Injuries DOI 10.1007/978-3-642-36801-1_26-1 # Springer-Verlag Berlin Heidelberg 2014 Posterior Shoulder Pain and Arthroscopic Decompression of the Suprascapular Nerve Kevin D. Planchera,b* and Stephanie C. Pettersonc aPlancher Orthopaedics and Sports Medicine, New York, NY, USA bDepartment of Orthopaedic Surgery, Albert Einstein College of Medicine, New York, NY, USA cOrthopaedic Foundation, Stamford, CT, USA Abstract Posterior shoulder pain is more often than not mistakenly identified as rotator cuff disease or cervical disk disease. While most current thoughts may be buried in the literature as suprascapular nerve entrapment, it is hoped that with a clearer understanding of this disease entity, patients will be treated in a timely manner and receive the expected outcome with great satisfaction. Introduction An article in the New England Journal of Medicine in 1959 opened the gates for discussion about suprascapular nerve entrapment in the clinical setting (Thompson and Kopell 1959). Various authors, including the authors of this chapter, have described the transverse scapular ligament and spinoglenoid notch as two potential sites of entrapment of the Suprascapular nerve (Post and Mayer 1987; Cummins et al. 2000; Plancher et al. 2005a, 2007) (Fig. 1). This injury, when recognized, leads to a multitude of symptoms including pain and weakness with an inability to hold even a 5-kg weight in the horizontal plane. The pain and disability associated with this condition can be unduly prolonged, but it is easily cured now with advanced arthroscopic techniques. While this entity represents a small percentage of the average shoulder surgeons’ practice, recent advancements as well as diagnostic testing have brought this diagnosis of exclusion to the forefront and minds of many surgeons. -

Anatomy of of Suprascapular Notch Among North Indian Dry Scapulae: a Morphological Evaluation
International Journal of Current Research and Review Original Article DOI: http://dx.doi.org/10.31782/IJCRR.2020.12227 Anatomy of of Suprascapular Notch among North Indian Dry Scapulae: A Morphological Evaluation IJCRR 1 2 1 3 Section: Healthcare Susmita Saha , Shilpi Garg , Kirandeep Kaur , Prachi Saffar Aneja Sci. Journal Impact Factor: 6.1 (2018) 1 ICV: 90.90 (2018) Associate Professor, Department of Anatomy, Faculty of Medicine & Health Sciences, SGT Medical College, Budhera, Gurgaon-122505, India; 2Assistant Professor, Department of Anatomy, Faculty of Medicine & Health Sciences, SGT Medical College, Budhera, Gur- gaon-122505, India; 3Professor & Head, Department of Anatomy, Faculty of Medicine & Health Sciences, SGT Medical College, Budhera, Copyright@IJCRR Gurgaon-122505, India. ABSTRACT . Background: The suprascapular notch (SSN) is a depression located in the lateral portion of the upper border of the scapula encroached by the superior transverse scapular ligament. It may be completely or partially ossified to transform the notch into a foramen which acts as a gateway for the passage of the suprascapular nerve. Methods: Two hundred & ninety adult dry scapulae (132 right & 158 left) from the osteology museum of the Department of Anatomy, belonging to North Indian population of unknown sex were obtained for the variable morphologic pattern of SSN by subjective evaluation according to Rengachary’s classification. We have also examined the morphological variant of the ossified superior transverse suprascapular ligament (STSL). Results: We have concluded six different morphological variations of SSN. Among them, the Type III SSN had the highest incidence of 41.7%. Morphological variability was noted for the ossified STSL: fan-shaped & band like; morphometric analysis was also performed for the completely ossified STSL.