Honeymoon Palsy and Other Upper Extremity Entrapment Neuropathies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Occupational Therapy Guide for Entry
University of North Dakota UND Scholarly Commons Occupational Therapy Capstones Department of Occupational Therapy 2008 An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries Ryan Edwards University of North Dakota Follow this and additional works at: https://commons.und.edu/ot-grad Part of the Occupational Therapy Commons Recommended Citation Edwards, Ryan, "An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries" (2008). Occupational Therapy Capstones. 57. https://commons.und.edu/ot-grad/57 This Scholarly Project is brought to you for free and open access by the Department of Occupational Therapy at UND Scholarly Commons. It has been accepted for inclusion in Occupational Therapy Capstones by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. AN OCCUPATIONAL THERAPY GUIDE FOR ENTRY-LEVEL THERAPISTS NOT SPECIALIZING IN THE TREATMENT OF UPPER EXTREMITY DYSFUNCTION: THREE COMMON CUMULATIVE TRAUMA INJURIES by Ryan Edwards Advisor: Anne Haskins PhD, OTR/L A Scholarly Project Submitted to the Occupational Therapy Department of the University of North Dakota In partial fulfillment of the requirements for the degree of Master’s of Occupational Therapy Grand Forks, North Dakota August 1, 2008 This Scholarly Project Paper, submitted by Ryan Edwards in partial fulfillment of the requirement for the Degree of Master’s of Occupational Therapy from the University of North Dakota, has been read by the Faculty Advisor under whom the work has been done and is hereby approved. -

Median Nerve Compression at Pronator Teres
1 Median Nerve Compression at Pronator Teres Surgical Indications and Considerations Anatomical Considerations: The median nerve and brachial artery travel together down the arm. Therefore, one must be very careful not to interfere with either the median nerve or the brachial artery, especially when conducting surgical procedures. In the area of the pronator teres, there are many tendons as well. It is important to identify, as much as possible, the correct site of compression. Pathogenesis: The median nerve can get entrapped or compressed by several structures in the arm. The pronator teres muscle is the most common. Others entrapment sites include the flexor digitorum superficialis arch, the lacertus fibrosis (bicipital aponeurosis), and ligament of Struthers (frequency occurs in that order). For compression of the median nerve at the pronator teres and flexor digitorum superficialis, the cause is almost always due to hypertrophy of the respected muscle. This hypertrophy is from quick, forceful and repeated movements to the involved muscle. Examples include a carpenter or a baseball batter. As the muscle hypertrophies, the signal from the median nerve is diminished resulting in paresthesias in the median nerve distribution (lateral arm and hand) distal to the site of compression. Pain in the volar part of the forearm, often aggravated by repetitive supination and pronation, is a common symptom of pronator involvement. Another indicator is forearm pain with the compression of muscle such as pain in the volar part of the forearm implicating pronator teres. Onset is typically insidious and diagnosis is usually delayed 9 months to 2 years. Epidemiology: Pronator teres syndrome is the second most common cause of median nerve compression behind carpal tunnel syndrome. -

Gross Anatomy
www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY www.BookOfLinks.com Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the infor- mation contained herein with other sources. For example and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY David A. Morton, PhD Associate Professor Anatomy Director Department of Neurobiology and Anatomy University of Utah School of Medicine Salt Lake City, Utah K. Bo Foreman, PhD, PT Assistant Professor Anatomy Director University of Utah College of Health Salt Lake City, Utah Kurt H. -
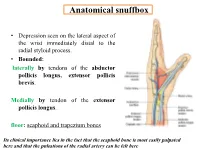
Anatomical Snuffbox
Anatomical snuffbox • Depression seen on the lateral aspect of the wrist immediately distal to the radial styloid process. • Bounded: laterally by tendons of the abductor pollicis longus, extensor pollicis brevis. Medially by tendon of the extensor pollicis longus. floor: scaphoid and trapezium bones Its clinical importance lies in the fact that the scaphoid bone is most easily palpated here and that the pulsations of the radial artery can be felt here Anatomical snuffbox Anatomical snuffbox • Contents: 2) Origin of the 1) The radial artery cephalic vein pass subcutaneously over the snuffbox. 3) Superficial branch of the radial nerve pass subcutaneously over the snuffbox. Blood supply of the hand Anastomoses occur between the radial and ulnar arteries via the superficial and deep palmar arches The Deep palmar arch is formed mainly by the radial artery while the superficial palmar arch is formed mainly by the ulnar artery 3-On entering the palm, it curves laterally behind (deep) the palmar 4-The arch is aponeurosis and in front completed on (superficial) of the long flexor the lateral side tendons forming by the the superficial palmar arch superficial branch of the radial artery. 2-Then it gives off its deep branch of which runs in front of the FR , and joins the radial artery to complete the deep palmar arch 1-Enters the hand anterior (superficial) to the Superficial flexor retinaculum palmar branch of radial artery through Guyon’s canal Radial artery 5-The superficial palmar arch gives off digital arteries from its convexity which pass to the fingers and supply them Superficial palmar arch Deep palmar branch of ulnar artery Superficial palmar branch of radial artery Ulnar artery Radial artery Radial Artery first dorsal interosseous muscle 1-From the floor of the anatomical snuff-box the radial artery leaves the dorsum of the hand by turning forward between the two heads of the first dorsal interosseous muscle. -

Suprascapular Nerve Lesions at the Spinoglenoid Notch: Report of Three Cases and Review of the Literature 243
Journal ofNeurology, Neurosurgery, and Psychiatry 1991;54:241-243 241 Suprascapular nerve lesions at the spinoglenoid J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.54.3.241 on 1 March 1991. Downloaded from notch: report of three cases and review of the literature Jay A Liveson, Michael J Bronson, Michael A Pollack Abstract of root involvement (cervical pain, and change Lesions of the suprascapular nerve can from Valsalva's manoeuvre). His past medical occur at the supraspinatus notch (SSN) history was negative. On physical examination or at the spinoglenoid notch (SGN). Elec- cranial nerves were normal. No weakness was tromyographic (EMG), evaluation of the detected on careful manual muscle examin- infraspinatus, and especially the supra- ation. Sensation was intact. Deep tendon spinatus muscles distinguishes SGN reflexes were active and symmetrical with no from SSN lesions. Three cases of SGN pathological reflexes. There was no Homer's lesions, which are more common than sign. SSN lesions, are presented. The patient gave up weight lifting and started a programme of physiotherapy. His shoulder ache resolved rapidly, but his muscle Entrapment of the suprascapular nerve at the bulk did not return to normal for another 12 suprascapular notch (SSN) was first described months. He reported completely normal func- in 1963 by Kopell and Thompson.' No alter- tion. native entrapment site was recognised until 1981 when the first case of spinoglenoid notch Case 2 (SGN) entrapmnt was described by Ganzhorn A 22 year old right handed male was skeet et al.2 Since then nine additional cases of SGN shooting, a month before his examination. -

Signs to Help the Deaf Included in This Packet
Signs to help the Deaf Included in this packet: Medical Signs Color Signs People Signs This is made by: Deanna Zander, I am a parent of a deaf son. Here is my email address: [email protected], if you have any questions, please email your question, Please put in the Subject box- RE: Medical Signs. For more information, or to obtain a hospital kit for Deaf or Hard of Hearing, please contact Pam Smith, Adult Outreach Coordinator @ 701-665-4401 Medical Signs (Medicine) Medical Medicine- Tip of bent middle finger rubs circle on left palm Sign- Palm-out indexes circle Signs alternately Made By: Deanna Zander Hi, Hello, Howdy Good-Bye, Yes, Yep Bye Right “S” hand & head nods (both head & hand nod) No, Nope Flat hand, Touch forehead, Just wave First two fingers close onto move forward slightly right thumb, & shake your head Appointment Schedule Fingertips of the right palm- out “5” draws down left palm; then turn palm-in & draws across palm The right “S” hand palm down, is postitioned above the left “S” hand, also palm- down. The right hand circels above the left in a clockwise manner & is brought on the back of left hand. Your Name, My Name Birthday My, Mine- Your- The right middle finger touches the chin, Palm of flat Vertical flat palm moves then moves down to touch the chest hand on chest toward person Fingerspell- The right hand, palm- out, is move left to right, fingers wiggling up & Name- Right “H” touches left “H” at right angles MM/DD/YYYY down Call, phone Left “Y” hand, thumb near ear, little finger near mouth The upturned thumbs -

Birth Cont R Ol Fact Sheet
VAGINAL RING FACT SHEET What is the Vaginal Ring (Nuvaring®)? The Vaginal Ring is a clear, flexible, thin, plastic ring that you place in the vagina where it stays for one cycle providing a continuous low dose of 2 hormones (estrogen and progestin). It prevents pregnancy by stopping the release of an egg (ovulation), thickening the cervical fluid, and changing the lining of the uterus. How effective is the Vaginal Ring? The ring is a very effective method of birth control. The ring is about 93% effective at preventing pregnancy in typical use, which means that around 7 out of 100 people who use it as their only form of birth control will get pregnant in one year. With consistent and correct use as described in this fact sheet, it can be over 99% effective. How can I get the Vaginal Ring? You can visit a clinic to get the ring or a prescription for it and talk with a healthcare provider about whether the ring is right for you. Advantages of the Vaginal Ring Disadvantages of the Vaginal Ring Periods may be more predictable/regular and lighter Must remember to remove and replace the ring once a Less period cramping month Decreased symptoms of Premenstrual Syndrome Some users may experience mild side effects such as: (PMS) and perimenopause spotting, nausea, breast tenderness, headaches, or Can be used to skip or shorten your periods dizziness (usually these improve in the first few months Less anemia/iron deficiency caused by heavy periods of use) Does not affect your ability to get pregnant in the Possibility of high blood pressure -

Arthroscopic Decompression of the Suprascapular Nerve at the Spinoglenoid Notch and Suprascapular Notch Through the Subacromial Space
Technical Note Arthroscopic Decompression of the Suprascapular Nerve at the Spinoglenoid Notch and Suprascapular Notch Through the Subacromial Space Neil Ghodadra, M.D., Shane J. Nho, M.D., M.S., Nikhil N. Verma, M.D., Stefanie Reiff, B.A., Dana P. Piasecki, M.D., Matthew T. Provencher, M.D., and Anthony A. Romeo, M.D. Abstract: Suprascapular nerve entrapment can cause disabling shoulder pain. Suprascapular nerve release is often performed for compression neuropathy and to release pressure on the nerve associated with arthroscopic labral repair. This report describes a novel all-arthroscopic technique for decom- pression of the suprascapular nerve at the suprascapular notch or spinoglenoid notch through a subacromial approach. Through the subacromial space, spinoglenoid notch cysts can be visualized between the supraspinatus and infraspinatus at the base of the scapular spine. While viewing the subacromial space through the lateral portal, the surgeon can use a shaver through the posterior portal to decompress a spinoglenoid notch cyst at the base of the scapular spine. To decompress the suprascapular nerve at the suprascapular notch, a shaver through the posterior portal removes the soft tissue on the acromion and distal clavicle to expose the coracoclavicular ligaments. The medial border of the conoid ligament is identified and followed to its coracoid attachment. The supraspinatus muscle is retracted with a blunt trocar placed through an accessory Neviaser portal. The transverse scapular ligament, which courses inferior to the suprascapular artery, is sectioned with arthroscopic scissors, and the suprascapular nerve is decompressed. Key Words: Arthroscopy—Suprascapular nerve—Transverse scapular ligament—Suprascapular notch—Rotator cuff—Shoulder. -

Hand Gestures
L2/16-308 More hand gestures To: UTC From: Peter Edberg, Emoji Subcommittee Date: 2016-10-31 Proposed characters Tier 1: Two often-requested signs (ILY, Shaka, ILY), and three to complete the finger-counting sets for 1-3 (North American and European system). None of these are known to have offensive connotations. HAND SIGN SHAKA ● Shaka sign ● ASL sign for letter ‘Y’ ● Can signify “Aloha spirit”, surfing, “hang loose” ● On Emojipedia top requests list, but requests have dropped off ● 90°-rotated version of CALL ME HAND, but EmojiXpress has received requests for SHAKA specifically, noting that CALL ME HAND does not fulfill need HAND SIGN ILY ● ASL sign for “I love you” (combines signs for I, L, Y), has moved into mainstream use ● On Emojipedia top requests list HAND WITH THUMB AND INDEX FINGER EXTENDED ● Finger-counting 2, European style ● ASL sign for letter ‘L’ ● Sign for “loser” ● In Montenegro, sign for the Liberal party ● In Philippines, sign used by supporters of Corazon Aquino ● See Wikipedia entry HAND WITH THUMB AND FIRST TWO FINGERS EXTENDED ● Finger-counting 3, European style ● UAE: Win, victory, love = work ethic, success, love of nation (see separate proposal L2/16-071, which is the source of the information below about this gesture, and also the source of the images at left) ● Representation for Ctrl-Alt-Del on Windows systems ● Serbian “три прста” (tri prsta), symbol of Serbian identity ● Germanic “Schwurhand”, sign for swearing an oath ● Indication in sports of successful 3-point shot (basketball), 3 successive goals (soccer), etc. HAND WITH FIRST THREE FINGERS EXTENDED ● Finger-counting 3, North American style ● ASL sign for letter ‘W’ ● Scout sign (Boy/Girl Scouts) is similar, has fingers together Tier 2: Complete the finger-counting sets for 4-5, plus some less-requested hand signs. -

Risk of Encountering Dorsal Scapular and Long Thoracic Nerves During Ultrasound-Guided Interscalene Brachial Plexus Block with Nerve Stimulator
Korean J Pain 2016 July; Vol. 29, No. 3: 179-184 pISSN 2005-9159 eISSN 2093-0569 http://dx.doi.org/10.3344/kjp.2016.29.3.179 | Original Article | Risk of Encountering Dorsal Scapular and Long Thoracic Nerves during Ultrasound-guided Interscalene Brachial Plexus Block with Nerve Stimulator Department of Anesthesiology and Pain Medicine, Wonkwang University College of Medicine, Wonkwang Institute of Science, Iksan, *Department of Anesthesiology and Pain Medicine, Presbyterian Medical Center, University of Seonam College of Medicine, Jeonju, Korea Yeon Dong Kim, Jae Yong Yu*, Junho Shim*, Hyun Joo Heo*, and Hyungtae Kim* Background: Recently, ultrasound has been commonly used. Ultrasound-guided interscalene brachial plexus block (IBPB) by posterior approach is more commonly used because anterior approach has been reported to have the risk of phrenic nerve injury. However, posterior approach also has the risk of causing nerve injury because there are risks of encountering dorsal scapular nerve (DSN) and long thoracic nerve (LTN). Therefore, the aim of this study was to evaluate the risk of encountering DSN and LTN during ultrasound-guided IBPB by posterior approach. Methods: A total of 70 patients who were scheduled for shoulder surgery were enrolled in this study. After deciding insertion site with ultrasound, awake ultrasound-guided IBPB with nerve stimulator by posterior approach was performed. Incidence of muscle twitches (rhomboids, levator scapulae, and serratus anterior muscles) and current intensity immediately before muscle twitches disappeared were recorded. Results: Of the total 70 cases, DSN was encountered in 44 cases (62.8%) and LTN was encountered in 15 cases (21.4%). Both nerves were encountered in 10 cases (14.3%). -

Distal Radial Approach Through the Anatomical Snuff Box for Coronary Angiography and Percutaneous Coronary Intervention
Korean Circ J. 2018 Dec;48(12):1131-1134 https://doi.org/10.4070/kcj.2018.0293 pISSN 1738-5520·eISSN 1738-5555 Editorial Distal Radial Approach through the Anatomical Snuff Box for Coronary Angiography and Percutaneous Coronary Intervention Jae-Hyung Roh, MD, PhD, and Jae-Hwan Lee , MD, PhD Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea ► See the article “Feasibility of Coronary Angiography and Percutaneous Coronary Intervention via Left Snuffbox Approach” in volume 48 on page 1120. Received: Aug 27, 2018 The anatomical snuffbox, also known as the radial fossa, is a triangular-shaped depression Accepted: Sep 17, 2018 on the radial, dorsal aspect of the hand at the level of the carpal bones. It is clearly observed Figure 1 1)2) Correspondence to when the thumb is extended ( ). The bottom of the snuffbox is supported by carpal Jae-Hwan Lee, MD, PhD bones composed of the scaphoid and trapezium. The medial and lateral borders are bounded Division of Cardiology, Department of Internal by tendons of the extensor pollicis longus and the extensor pollicis brevis, respectively. The Medicine, Chungnam National University proximal border is formed by the styloid process of the radius. Within this narrow triangular Hospital, Chungnam National University space, various structures are located, including the distal radial artery (RA), a branch of the School of Medicine, 282, Munhwa-ro, Jung-gu, radial nerve, and the cephalic vein. Daejeon 35015, Korea. E-mail: [email protected] The anatomy of the hand arteries is illustrated in Figure 2. -

Systemic Lupus Erythematosus Presenting with Finger Drop
DOI: 10.7860/JCDR/2018/36196.12107 Case Report Systemic Lupus Erythematosus Section Presenting with Finger Drop Internal Medicine MARJAN RAHIMI FARAHANI1, SAMIRA ALESAEIDI2 ABSTRACT Systemic Lupus Erythematosus (SLE) is an autoimmune disease with multiple organ involvement that can affect joints, skin, heart, lungs, kidneys and nervous system. SLE is a multisystem disorder resulting from abnormal immunological function. SLE affects women more than men. It affects both the central and the peripheral nervous system. Severe acute peripheral neuropathy in SLE is quite rare and it is always accompanied by evidence of active disease in other organs, including the central nervous system. The recognition of neurologic symptoms in SLE remains a clinical problem for physicians. Neurological manifestations are frequently present in SLE patients, although the peripheral nervous system involvement is rarer than the central one. Peripheral neuropathy is a known but uncommon presentation of SLE and the aim of this study is to report various forms of lupus-related neuropathies that may present as finger drop and discusses one of the rare neurological manifestations of lupus which remains a diagnostic challenge. Keywords: Autoimmune diseases, Nervous system, Pathology CASE REPORT A 33-year-old female was referred to the hospital with a chief compliant of symmetric finger drop of second, third and fourth fingers without any wrist drop for nine months before. She was able to use her fists but she had limitation on abduction of all fingers and also full extension of metacarpophalangeal and interphalangeal joints. The evaluation of sensation and reflexes were normal. The patient complained of shoulder, wrist, interphalangeal, knee, and elbow and ankle arthralgia.