2015 Community Health Needs Assessment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Health Facilities and Services Review Board
STATE OF ILLINOIS HEALTH FACILITIES AND SERVICES REVIEW BOARD 525 WEST JEFFERSON ST. • SPRINGFIELD, ILLINOIS 62761 •(217) 782-3516 FAX: (217) 785-4111 DOCKET NO: BOARD MEETING: PROJECT NO: September 14, 2021 21-016 PROJECT COST: H-04 FACILITY NAME: CITY: Original: $170,520,604 NorthShore Glenbrook Hospital Glenview TYPE OF PROJECT: Substantive HSA: VII PROJECT DESCRIPTION: The Applicant [NorthShore University HealthSystem] is asking the State Board approve establishment of an open-heart surgery category of service, the addition of 8 cardiac cath labs, and the addition of 6 surgery rooms at Glenbrook Hospital in Glenview, Illinois. The cost of the project is $170,520,604. The expected completion date is December 31, 2024. The purpose of the Illinois Health Facilities Planning Act is to establish a procedure (1) which requires a person establishing, constructing or modifying a health care facility, as herein defined, to have the qualifications, background, character and financial resources to adequately provide a proper service for the community; (2) that promotes the orderly and economic development of health care facilities in the State of Illinois that avoids unnecessary duplication of such facilities; and (3) that promotes planning for and development of health care facilities needed for comprehensive health care especially in areas where the health planning process has identified unmet needs. Cost containment and support for safety net services must continue to be central tenets of the Certificate of Need process. (20 ILCS 3960/2) The Certificate of Need process required under this Act is designed to restrain rising health care costs by preventing unnecessary construction or modification of health care facilities. -

View a List of the 2021 Performance Achievement Award Recipients
Congratulations to the Recipients of the Rewarding Excellence. Driving Success. The Chest Pain – MI Registry Performance Achievement Award recognizes a hospital’s success in implementing Chest Pain – MI Registry™ a higher standard of care for heart attack patients by meeting aggressive performance measures. 2021 Performance Achievement Award View hospitals participating in the registry at CardioSmart.org/ChestPainMI. St. Francis Medical Center Lee’s Summit Medical Center Summa Health Ascension Seton Medical Center Hays St. Luke’s Hospital Christian Hospital BJC Healthcare JFK Medical Center Baylor Scott & White Heart and Colorado Springs, CO Lee’s Summit, MO Akron, OH Cedar Rapids, IA St. Louis, MO Edison, NJ Vascular – Dallas Kyle, TX Dallas, TX 2021 The George Washington University Hospital SSM Health Saint Louis University Hospital Summa Health 2021 Trinity Medical Center – Bettendorf Citizens Memorial Hospital Ocean Medical Center Washington, DC St. Louis, MO Barberton, OH Dell Seton Medical Center at Bettendorf, IA Bolivar, MO Brick, NJ Baylor Scott & White Medical Center The University of Texas AdventHealth Celebration SSM Health St. Mary’s Hospital – The University of Toledo Medical Center Trinity Regional Medical Center Cox Medical Center Branson Riverview Medical Center – Round Rock Austin, TX Round Rock, TX Kissimmee, FL Jefferson City Toledo, OH Ft. Dodge, IA Branson, MO Red Bank, NJ Jefferson City, MO Houston Methodist The Woodlands Hospital CHRISTUS Mother Frances Hospital Chest Pain – MI Hamilton Medical Center Ascension -

Provider Partners Chicago
Provider Partners Chicago Enjoy direct access to quality healthcare where you live. No Guesswork. Choose to see a carefully selected Imagine Health provider and receive affordable, quality care. No referrals. You have the simplicity of direct access to quality hospitals and physicians in your area. It’s that easy. Walk-in Care. You have access to all CVS MinuteClinic® locations nationwide, which provide a broad range of services to help keep you and your family healthy. Lab Services. Rely on Quest Diagnostics for all your lab-related diagnostic services. Peace of mind. When you use an Imagine Health provider, you won’t be billed for more than your patient responsibility. It makes good sense. Count on getting the most out of your plan when you see one of our partners in Chicago. For a current and complete list of Imagine providers in your area, visit hospitals + providers 22 8,100 providers.imaginehealth.com or download the mobile app. + urgent + ambulatory 70 cares 10 surgical centers Now it’s easier than ever before to get quality healthcare in Chicago. Provider Partners Include: AMITA Presence Health | Northwestern Medicine | Edward-Elmhurst Health Northwest Community Healthcare | Ann & Robert H. Lurie Childrens Hospital Hospitals 1. AMITA Health Mercy Medical Center Aurora 1325 N Highland Ave Aurora, IL 60506 2. AMITA Health Resurrection Medical Center Chicago 7435 W Talcott Ave Chicago, IL 60631 3. AMITA Health Saint Francis Hospital Evanston - Chicago 355 Ridge Ave Evanston, IL 60202 4. AMITA Health Saint Joseph Hospital - Chicago 2900 N Lake Shore Dr Chicago, IL 60657 5. AMITA Health Saint Joseph Hospital Elgin 77 N Airlite St Elgin, IL 60123 NOTE: Members also have access to ambulatory surgical centers, AMITA Health Saint Joseph 6. -
For Immediate Release
MBGH MEDIA CONTACT: Cary Conway [email protected] 972.649.4707 Illinois Hospitals Receive New Spring 2019 Patient Safety Grades from The Leapfrog Group 40% of graded hospitals in state received an A, no hospitals received an F CHICAGO – May 15, 2019 – The Leapfrog Group, a national nonprofit representing the nation’s largest and most influential employers and purchasers of health care, announced today the spring 2019 Leapfrog Hospital Safety Grades. The independent grading system assigns A, B, C, D and F letter grades to general acute-care hospitals in the US based on their ability to protect patients from avoidable errors, injuries, accidents and infections. Of the 110 hospitals in Illinois graded, 40% earned an A, 27% B’s, and 29% earned C’s. Five hospitals earned a score of D, with no hospitals receiving an F. Illinois moved down a spot in the national rankings to the 14th spot. The Midwest Business Group on Health (MBGH), a non-profit organization representing employer purchasers of health care, and the Leapfrog Group’s Illinois Regional Leader, annually encourages Illinois hospitals to participate in Leapfrog’s online patient safety survey. Hospitals earning an A grade: • AMITA Health Adventist Medical Centers in • NorthShore University HealthSystem, Glenbrook Bolingbrook Hospital • AMITA Health Adventist Medical Center • NorthShore University HealthSystem, Skokie GlenOaks Hospital • AMITA Health Adventist Medical Center • NorthShore University HealthSystem, Highland Hinsdale Park Hospital • AMITA Health Adventist Medical Center La • Northwestern Medicine Central DuPage Hospital Grange • Northwestern Medicine Delnor Hospital • AMITA Health Resurrection Medical Center • OSF Heart of Mary Medical Center • AMITA Health Saint Joseph Hospital Chicago • OSF St. -

IHA Members by Illinois Senate District
IHA Members by IL Senate District Hospital City District: 1 Tony Munoz D none none 02-Aug-21 Members IL Senate District Page 1 of 60 IHA Members by IL Senate District Hospital City District: 2 Omar Aquino D AMITA Health Sts. Mary & Elizabeth Med Ctr, St. Chicago AMITA Health Sts. Mary & Elizabeth Med Ctr, St. Chicago Humboldt Park Health Chicago 02-Aug-21 Members IL Senate District Page 2 of 60 IHA Members by IL Senate District Hospital City District: 3 Mattie Hunter D Holy Cross Hospital Chicago Insight Hospital & Medical Center Chicago Jackson Park Hospital & Medical Center Chicago St. Bernard Hospital & Health Care Ctr Chicago 02-Aug-21 Members IL Senate District Page 3 of 60 IHA Members by IL Senate District Hospital City District: 4 Kimberly Lightford D Hartgrove Behavioral Health System Chicago Loretto Hospital Chicago Loyola University Medical Center Maywood Riveredge Hospital Forest Park 02-Aug-21 Members IL Senate District Page 4 of 60 IHA Members by IL Senate District Hospital City District: 5 Patricia Van Pelt D Garfield Park Behavioral Hospital Chicago Jesse Brown Veterans Administration Medical C Chicago John H. Stroger, Jr. Hospital of Cook Co. Chicago Mount Sinai Hospital Chicago RML Chicago Chicago Rush University Medical Center Chicago Schwab Rehabilitation Hospital Chicago University of Illinois Hospital & Health Sciences Chicago 02-Aug-21 Members IL Senate District Page 5 of 60 IHA Members by IL Senate District Hospital City District: 6 Sara Feigenholtz D Advocate Illinois Masonic Medical Center Chicago AMITA Health -
Admissions Requirements for the Edward Hospital Paramedic Program Spring 2022
Admissions Requirements for the Edward Hospital Paramedic Program Spring 2022 Please read this entire packet carefully and retain for your records _______________________________________ Paramedic I-II-III Fire 2278-2279-2280 THIS PACKET IS ONLY FOR STUDENTS INTERESTED IN EDWARD HOSPITAL Beginning Spring 2022 through Fall 2022 Application deadline: September 3, 2021 at 3 p.m. Classes and clinicals run January 2022 through December 2022 PLEASE MAINTAIN A PERSONAL COPY OF THIS PACKET FOR FUTURE REFERENCE Note: Students are not accepted into this program until they have received an official acceptance letter from Edward Hospital EMSS. Completion of Health Requirements, CPR completion, criminal background checks, and proof of insurance is an independent activity to prepare for entrance into health programs at College of DuPage and/or participation in clinical sites within health programs. Funds paid to Edward Corporate Health or to a personal health care provider/source, CastleBranch.com, insurance companies, and funds used towards CPR completion are not eligible for any sort of refund from College of DuPage if the required course is not successfully completed. Last Updated: 3/31/2021 Page 1 PROGRAM OVERVIEW College of DuPage (COD) offers Paramedic training through Central DuPage Hospital, Edward Hospital, Good Samaritan Hospital and Loyola University Medical Center Emergency Medical Services System (EMSS). These Paramedic training programs are currently utilizing the U.S. Department of Transportation’s National Education Standards and are approved to offer Paramedic training by the Illinois Department of Public Health (IDPH). The hospitals have been designated as Emergency Medical Services System resource hospitals by the State of Illinois. -
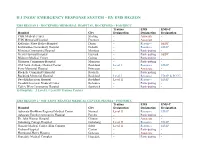
Illinois' Emergency Response System by EMS Region
ILLINOIS’ EMERGENCY RESPONSE SYSTEM – BY EMS REGION EMS REGION 1 - ROCKFORD MEMORIAL HOSPITAL, ROCKFORD – POD/RHCC Trauma EMS EMS-C Hospital City Designation Designation Designation CGH Medical Center Sterling - Associate - FHN Memorial Hospital Freeport - Associate - Katherine Shaw Bethea Hospital Dixon - Resource SEDP Kishwaukee Community Hospital DeKalb - Resource EDAP Mendota Community Hospital Mendota - Participating - Mercy Harvard Hospital Harvard - Participating SEDP Midwest Medical Center Galena - Participating - Morrison Community Hospital Morrison - Participating - OSF Saint Anthony Medical Center Rockford Level I Resource EDAP Perry Memorial Hospital Princeton - Associate - Rochelle Community Hospital Rochelle - Participating - Rockford Memorial Hospital Rockford Level I Resource EDAP & PCCC SwedishAmerican Hospital Rockford Level II Resource EDAP SwedishAmerican Medical Center Belvidere - Participating - Valley West Community Hospital Sandwich - Participating - 15 Hospitals – 2 Level I, 1 Level II Trauma Centers EMS REGION 2 - OSF SAINT FRANCIS MEDICAL CENTER, PEORIA – POD/RHCC Trauma EMS EMS-C Hospital City Designation Designation Designation Advocate BroMenn Regional Medical Center Normal Level II Resource EDAP Advocate Eureka Community Hospital Eureka - Participating - Dr. John Warner Hospital Clinton - Associate - Galesburg Cottage Hospital Galesburg Level II Resource EDAP Genesis Medical Center, Illini Campus Silvis Level II Resource EDAP Graham Hospital Canton - Participating - Hammond-Henry Hospital Geneseo - Associate - Hopedale Medical Complex Hopedale - Participating - Illinois Valley Community Hospital Peru - Resource SEDP Kewanee Hospital Kewanee - Resource SEDP McDonough District Hospital Macomb - Resource EDAP Mercer County Hospital Aledo - Participating - Methodist Medical Center of Illinois Peoria Level II Associate EDAP OSF Holy Family Medical Center Monmouth - Participating - OSF Saint Francis Medical Center Peoria Level I Resource EDAP & PCCC OSF Saint James – JW Albrecht Medical Center Pontiac - Resource EDAP OSF St. -

Healthchoice Illinois ADT Participants As of 06 01 2021
HealthChoice Illinois ADT Participants as of 6/01/2021 X = Complete | O = In Progress Sources of Data Type Contributing Data Consuming Data Hospitals Abraham Lincoln Memorial Hospital Critical Access Hospitals O Advocate Christ Medical Center Short-term (General and Specialty) Hospitals O Advocate Condell Medical Center Short-term (General and Specialty) Hospitals O Advocate Good Samaritan Hospital Short-term (General and Specialty) Hospitals O Advocate Good Shepherd Hospital Short-term (General and Specialty) Hospitals O Advocate Illinois Masonic Medical Center Short-term (General and Specialty) Hospitals O Advocate Lutheran General Hospital Short-term (General and Specialty) Hospitals O Advocate Sherman Hospital Short-term (General and Specialty) Hospitals O Advocate South Suburban Hospital Short-term (General and Specialty) Hospitals O Advocate Trinity Hospital Short-term (General and Specialty) Hospitals O AMITA Health Adventist Med Ctr Bolingbrook Short-term (General and Specialty) Hospitals O AMITA Health Adventist Med Ctr GlenOaks Short-term (General and Specialty) Hospitals O AMITA Health Adventist Med Ctr Hinsdale Short-term (General and Specialty) Hospitals O AMITA Health Adventist Med Ctr La Grange Short-term (General and Specialty) Hospitals O AMITA Health Alexian Brothers Behav Health Hosp Hoffman Estates Psychiatric Hospitals (Excluded from IPPS) O AMITA Health Alexian Brothers Med Ctr Elk Grove Village Short-term (General and Specialty) Hospitals O AMITA Health Holy Family Med Ctr Long-Term Care Hospitals (Excluded from -

Hospitals We Serve
Hospitals We Serve Illinois Cook County Kindred Hospital – Northlake Campus DeKalb County AMITA Health Alexian Brothers Medical Little Company of Mary Hospital and Kindred Hospital – Sycamore Center – Elk Grove Village Health Care Centers Northwestern Kishwaukee Hospital AMITA Health Alexian Brothers Loretto Hospital Northwestern Valley West Hospital Rehabilitation Hospital – Mount Sinai Hospital Elk Grove Village Northwest Community Hospital AMITA Health Adventist Medical DuPage County Center – Hinsdale Northwestern Memorial Hospital AMITA Health Adventist Medical Center AMITA Health Alexian Brothers Women & Northwestern Prentice Women’s Hospital Children’s Hospital – Hoffman Estates Edward Hospital & Health Services Norwegian American Hospital AMITA Health St. Alexius Medical Center – Elmhurst Memorial Hospital Palos Community Hospital Hoffman Estates Northwestern Central DuPage Hospital AMITA Health Adventist Medical Center Presence Holy Family Medical Center – LaGrange Presence Saint Francis Hospital Grundy County Community First Medical Center – Evanston Morris Hospital Edward Hines Jr. VA Hospital Presence Saint Joseph Hospital – Chicago Franciscan St. James Health – Presence Saints Mary and Elizabeth Chicago Heights Medical Center – Saint Elizabeth Campus Kane County Franciscan St. James Health – Presence Saints Mary and Elizabeth Northwestern Delnor Hospital Olympia Fields Medical Center – Saint Mary Campus Presence Mercy Center Holy Cross Hospital Presence Resurrection Medical Center Presence St. Joseph Hospital Ingalls Memorial -

COVID-19: Illinois Hospitals and Health Systems Response
COVID-19: Illinois hospitals and health systems response Illinois’ more than 200 hospitals and nearly 40 health systems took swift action in response to the coronavirus outbreak thanks to staunch preparation and training. Learn about their ongoing efforts. COVID-19 HOTLINE The Illinois Poison Center and IDPH launched a coronavirus hotline to assist healthcare providers and the general public. (KFVS 12, Feb. 8) ELECTIVE SURGERIES Edward-Elmhurst Health System is adopting new measures to deal with the coronavirus outbreak, including screening all visitors for flu-like symptoms before allowing entrance into the hospital, not allowing anyone under 18 to visit, cancelling all elective surgeries and closing all of their fitness centers (Kane County Chronicle, March 16) HSHS St. John’s Hospital, Memorial Health System and SIU Medicine implemented additional screening for patients entering their facilities and have canceled elective surgeries. (The State Journal-Register, March 17) Advocate BroMenn Medical Center in Normal and Advocate Eureka Hospital in Eureka have made several changes to prevent the spread of COVID-19, including canceling non-urgent visits and some elective surgeries and implementing visitor restrictions. (The Pantagraph, March 18) NorthShore University HealthSystem canceled elective surgeries and turned outpatient sites into screening centers to expand capacity for possible COVID-19 patients. (Health News Illinois, March 27) OSF HealthCare St. Joseph Medical Center in Bloomington enacted visitor restrictions and delayed non-urgent surgeries to keep beds open. (The Pantagraph, March 27) Galesburg Cottage Hospital delayed elective surgeries to increased capacity and conserve supplies. (The Register-Mail, March 28) OSF Healthcare St. Mary Medical Center in Galesburg postponed elective surgeries, implemented enhanced screening and isolation protocol, and enacted efforts to conserve supplies. -
Paramedic I-II-III Fire 2278-2279-2280
Admissions Requirements for the Central DuPage Hospital Paramedic Program Spring 2022 Please read this entire packet carefully and retain for your records _______________________________________ Paramedic I-II-III Fire 2278-2279-2280 THIS PACKET IS ONLY FOR STUDENTS INTERESTED IN CENTRAL DUPAGE HOSPITAL Beginning Spring 2022 through Fall 2022 Application deadline: September 1, 2021 at 3 p.m. Classes, Clinicals, and Internships run January 2022 through December 2022 PLEASE MAINTAIN A PERSONAL COPY OF THIS PACKET FOR FUTURE REFERENCE Note: Students are not accepted into this program until they have received an official acceptance letter from Central DuPage Hospital EMSS. Completion of Health Requirements, CPR completion, criminal background checks, and proof of insurance is an independent activity to prepare for entrance into health programs at College of DuPage and/or participation in clinical sites within health programs. Funds paid to Edward Corporate Health or to a personal health care provider/source, CastleBranch.com, insurance companies, and funds used towards CPR completion are not eligible for any sort of refund from College of DuPage if the required course is not successfully completed. Last Updated: 4/6/2021 Page 1 PROGRAM OVERVIEW College of DuPage (COD) offers Paramedic training through Central DuPage Hospital, Edward Hospital, Good Samaritan Hospital and Loyola University Medical Center Emergency Medical Services System (EMSS). These Paramedic training programs are currently utilizing the U.S. Department of Transportation’s National Curriculum as required by the Illinois Department of Public Health (IDPH) for those interested in attaining Paramedic certification. EMSS is a hospital based program for the delivery of pre-hospital stabilization of ill and injured patients. -
Chicago OAII 10-13.Indd
HealthLink OAII Hospital Locations – Chicago, IL and Surrounding Area Northbrook Cook County 14 Schaumburg 190 290 DuPage County 20 Oak Park 90 88 45 Chicago 55 294 Interstate Highway 94 12 34 U.S. Highway Naperville Downers Grove Waterway 355 55 12 Oak Lawn 41 Participating Hospitals Advocate Bethany Hospital (Cook County) Advocate Christ Medical Center (Cook County) Advocate Good Samaritan Hospital 6 (DuPage County) 57 Advocate Illinois Masonic Hospital (Cook County) Advocate Lutheran General Hospital (Cook County) 80 Advocate South Suburban Hospital (Cook County) Chicago Advocate Trinity Hospital (Cook County) Heights Alexian Brothers Medical Center (Cook County) Ann & Robert H Lurie Children’s Hospital of Chicago 30 (Cook County) Central DuPage Hospital (DuPage County) Children’s Memorial Hospital (Cook County) Northshore University Health System (Cook County) Edward Hospital (DuPage County) Northshore University Health System – Franciscan St. James Health (Cook County) Evanston Hospital (Cook County) Gottlieb Memorial Hospital (Cook County) Northshore University Health System – Holy Cross Hospital (Cook County) Glenbrook Hospital (Cook County) Ingalls Memorial Hospital (Cook County) Northshore University Health System – RML Specialty Hospital (DuPage County) Jackson Park Hospital (Cook County) Skokie Hospital (Cook County) South Shore Hospital (Cook County) La Rabida Children’s Hospital & Research Center Northwest Community Hospital (Cook County) St. Alexius Medical (Cook County) (Cook County) Northwestern Memorial Hospital (Cook County) St. Anthony Hospital (Cook County) LCM Op Care Center (Cook County) Norwegian American Hospital (Cook County) St. Bernard Hospital (Cook County) Little Company of Mary Care Station (Cook County) Palos Community Hospital (Cook County) St. James Hospital Olympia Fields Campus Little Company of Mary Hospital (Cook County) Presence Holy Family Medical Center (Cook County) (Cook County) Louis A Weiss Memorial Hospital (Cook County) Presence Our Lady of the Resurrection St.