Molecular Detection of Urogenital Mollicutes in Patients with Invasive Malignant Prostate Tumor Osama Mohammed Saed Abdul-Wahab1, Mishari H
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Comparative Genome Analysis of 19 Ureaplasma Urealyticum and Ureaplasma Parvum Strains
Paralanov et al. BMC Microbiology 2012, 12:88 http://www.biomedcentral.com/1471-2180/12/88 RESEARCH ARTICLE Open Access Comparative genome analysis of 19 Ureaplasma urealyticum and Ureaplasma parvum strains Vanya Paralanov1, Jin Lu2, Lynn B Duffy2, Donna M Crabb2, Susmita Shrivastava1, Barbara A Methé1, Jason Inman1, Shibu Yooseph1, Li Xiao2, Gail H Cassell2, Ken B Waites2 and John I Glass1* Abstract Background: Ureaplasma urealyticum (UUR) and Ureaplasma parvum (UPA) are sexually transmitted bacteria among humans implicated in a variety of disease states including but not limited to: nongonococcal urethritis, infertility, adverse pregnancy outcomes, chorioamnionitis, and bronchopulmonary dysplasia in neonates. There are 10 distinct serotypes of UUR and 4 of UPA. Efforts to determine whether difference in pathogenic potential exists at the ureaplasma serovar level have been hampered by limitations of antibody-based typing methods, multiple cross-reactions and poor discriminating capacity in clinical samples containing two or more serovars. Results: We determined the genome sequences of the American Type Culture Collection (ATCC) type strains of all UUR and UPA serovars as well as four clinical isolates of UUR for which we were not able to determine serovar designation. UPA serovars had 0.75−0.78 Mbp genomes and UUR serovars were 0.84−0.95 Mbp. The original classification of ureaplasma isolates into distinct serovars was largely based on differences in the major ureaplasma surface antigen called the multiple banded antigen (MBA) and reactions of human and animal sera to the organisms. Whole genome analysis of the 14 serovars and the 4 clinical isolates showed the mba gene was part of a large superfamily, which is a phase variable gene system, and that some serovars have identical sets of mba genes. -

Role of Protein Phosphorylation in Mycoplasma Pneumoniae
Pathogenicity of a minimal organism: Role of protein phosphorylation in Mycoplasma pneumoniae Dissertation zur Erlangung des mathematisch-naturwissenschaftlichen Doktorgrades „Doctor rerum naturalium“ der Georg-August-Universität Göttingen vorgelegt von Sebastian Schmidl aus Bad Hersfeld Göttingen 2010 Mitglieder des Betreuungsausschusses: Referent: Prof. Dr. Jörg Stülke Koreferent: PD Dr. Michael Hoppert Tag der mündlichen Prüfung: 02.11.2010 “Everything should be made as simple as possible, but not simpler.” (Albert Einstein) Danksagung Zunächst möchte ich mich bei Prof. Dr. Jörg Stülke für die Ermöglichung dieser Doktorarbeit bedanken. Nicht zuletzt durch seine freundliche und engagierte Betreuung hat mir die Zeit viel Freude bereitet. Des Weiteren hat er mir alle Freiheiten zur Verwirklichung meiner eigenen Ideen gelassen, was ich sehr zu schätzen weiß. Für die Übernahme des Korreferates danke ich PD Dr. Michael Hoppert sowie Prof. Dr. Heinz Neumann, PD Dr. Boris Görke, PD Dr. Rolf Daniel und Prof. Dr. Botho Bowien für das Mitwirken im Thesis-Komitee. Der Studienstiftung des deutschen Volkes gilt ein besonderer Dank für die finanzielle Unterstützung dieser Arbeit, durch die es mir unter anderem auch möglich war, an Tagungen in fernen Ländern teilzunehmen. Prof. Dr. Michael Hecker und der Gruppe von Dr. Dörte Becher (Universität Greifswald) danke ich für die freundliche Zusammenarbeit bei der Durchführung von zahlreichen Proteomics-Experimenten. Ein ganz besonderer Dank geht dabei an Katrin Gronau, die mich in die Feinheiten der 2D-Gelelektrophorese eingeführt hat. Außerdem möchte ich mich bei Andreas Otto für die zahlreichen Proteinidentifikationen in den letzten Monaten bedanken. Nicht zu vergessen ist auch meine zweite Außenstelle an der Universität in Barcelona. Dr. Maria Lluch-Senar und Dr. -

The Phylogenetic Composition and Structure of Soil Microbial Communities Shifts in Response to Elevated Carbon Dioxide
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Minnesota Digital Conservancy The ISME Journal (2012) 6, 259–272 & 2012 International Society for Microbial Ecology All rights reserved 1751-7362/12 www.nature.com/ismej ORIGINAL ARTICLE The phylogenetic composition and structure of soil microbial communities shifts in response to elevated carbon dioxide Zhili He1, Yvette Piceno2, Ye Deng1, Meiying Xu1,3, Zhenmei Lu1,4, Todd DeSantis2, Gary Andersen2, Sarah E Hobbie5, Peter B Reich6 and Jizhong Zhou1,2 1Institute for Environmental Genomics, Department of Botany and Microbiology, University of Oklahoma, Norman, OK, USA; 2Ecology Department, Earth Sciences Division, Lawrence Berkeley National Laboratory, Berkeley, CA, USA; 3Guangdong Provincial Key Laboratory of Microbial Culture Collection and Application, Guangdong Institute of Microbiology, Guangzhou, China; 4College of Life Sciences, Zhejiang University, Hangzhou, China; 5Department of Ecology, Evolution, and Behavior, St Paul, MN, USA and 6Department of Forest Resources, University of Minnesota, St Paul, MN, USA One of the major factors associated with global change is the ever-increasing concentration of atmospheric CO2. Although the stimulating effects of elevated CO2 (eCO2) on plant growth and primary productivity have been established, its impacts on the diversity and function of soil microbial communities are poorly understood. In this study, phylogenetic microarrays (PhyloChip) were used to comprehensively survey the richness, composition and structure of soil microbial communities in a grassland experiment subjected to two CO2 conditions (ambient, 368 p.p.m., versus elevated, 560 p.p.m.) for 10 years. The richness based on the detected number of operational taxonomic units (OTUs) significantly decreased under eCO2. -

Metabolic Network Percolation Quantifies Biosynthetic Capabilities
RESEARCH ARTICLE Metabolic network percolation quantifies biosynthetic capabilities across the human oral microbiome David B Bernstein1,2, Floyd E Dewhirst3,4, Daniel Segre` 1,2,5,6,7* 1Department of Biomedical Engineering, Boston University, Boston, United States; 2Biological Design Center, Boston University, Boston, United States; 3The Forsyth Institute, Cambridge, United States; 4Harvard School of Dental Medicine, Boston, United States; 5Bioinformatics Program, Boston University, Boston, United States; 6Department of Biology, Boston University, Boston, United States; 7Department of Physics, Boston University, Boston, United States Abstract The biosynthetic capabilities of microbes underlie their growth and interactions, playing a prominent role in microbial community structure. For large, diverse microbial communities, prediction of these capabilities is limited by uncertainty about metabolic functions and environmental conditions. To address this challenge, we propose a probabilistic method, inspired by percolation theory, to computationally quantify how robustly a genome-derived metabolic network produces a given set of metabolites under an ensemble of variable environments. We used this method to compile an atlas of predicted biosynthetic capabilities for 97 metabolites across 456 human oral microbes. This atlas captures taxonomically-related trends in biomass composition, and makes it possible to estimate inter-microbial metabolic distances that correlate with microbial co-occurrences. We also found a distinct cluster of fastidious/uncultivated taxa, including several Saccharibacteria (TM7) species, characterized by their abundant metabolic deficiencies. By embracing uncertainty, our approach can be broadly applied to understanding metabolic interactions in complex microbial ecosystems. *For correspondence: DOI: https://doi.org/10.7554/eLife.39733.001 [email protected] Competing interests: The authors declare that no Introduction competing interests exist. -

A Review of Ureaplasma Diversum: a Representative of the Mollicute Class Associated with Reproductive and Respiratory Disorders in Cattle
REVIEW published: 18 February 2021 doi: 10.3389/fvets.2021.572171 A Review of Ureaplasma diversum: A Representative of the Mollicute Class Associated With Reproductive and Respiratory Disorders in Cattle Manoel Neres Santos Junior 1,2, Nayara Silva de Macêdo Neres 1, Guilherme Barreto Campos 1, Bruno Lopes Bastos 1, Jorge Timenetsky 3 and Lucas Miranda Marques 1,2,3* 1 Department of Biointeraction, Multidisciplinary Institute of Health, Universidade Federal da Bahia, Vitória da Conquista, Brazil, 2 Department of Microbiology, State University of Santa Cruz (UESC), Ilhéus, Brazil, 3 Department of Microbiology, Institute of Biomedical Science, University of São Paulo, São Paulo, Brazil The Mollicutes class encompasses wall-less microbes with a reduced genome. They may infect plants, insects, humans, and animals including those on farms and in livestock. Edited by: Ureaplasma diversum is a mollicute associated with decreased reproduction mainly in the Michael Kogut, conception rate in cattle, as well as weight loss and decreased quality in milk production. United States Department of Agriculture, United States Therefore, U. diversum infection contributes to important economic losses, mainly in Reviewed by: large cattle-producing countries such as the United States, China, Brazil, and India. Marie Rene Culhane, The characteristics of Mollicutes, virulence, and pathogenic variations make it difficult to University of Minnesota, United States control their infections. Genomic analysis, prevalence studies, and immunomodulation Christine Letitia -

Comprehensive Analysis of Risk Factors for Periodontitis Focusing on the Saliva Microbiome and Polymorphism
International Journal of Environmental Research and Public Health Article Comprehensive Analysis of Risk Factors for Periodontitis Focusing on the Saliva Microbiome and Polymorphism Naoki Toyama 1,* , Daisuke Ekuni 1 , Daisuke Matsui 2, Teruhide Koyama 2 , Masahiro Nakatochi 3, Yukihide Momozawa 4, Michiaki Kubo 4 and Manabu Morita 1 1 Department of Preventive Dentistry, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, 2-5-1 Shikata-cho, Kita-ku, Okayama 700-8558, Japan; [email protected] (D.E.); [email protected] (M.M.) 2 Department of Epidemiology for Community Health and Medicine, Kyoto Prefectural University of Medicine, 465 Kajii-cho, Kamigyo-ku, Kyoto 602-8566, Japan; [email protected] (D.M.); [email protected] (T.K.) 3 Public Health Informatics Unit, Department of Integrated Health Sciences, Nagoya University Graduate School of Medicine, Nagoya 461-8673, Japan; [email protected] 4 Laboratory for Genotyping Development, RIKEN Center for Integrative Medical Sciences, 1-7-22 Suehiro-cho, Tsurumi-ku, Yokohama City 230-0045, Japan; [email protected] (Y.M.); [email protected] (M.K.) * Correspondence: [email protected]; Tel.: +81-86-235-6712 Abstract: Few studies have exhaustively assessed relationships among polymorphisms, the micro- biome, and periodontitis. The objective of the present study was to assess associations simultaneously among polymorphisms, the microbiome, and periodontitis. We used propensity score matching with a 1:1 ratio to select subjects, and then 22 individuals (mean age ± standard deviation, 60.7 ± 9.9 years) Citation: Toyama, N.; Ekuni, D.; were analyzed. -

Genome Diversity of Spore-Forming Firmicutes MICHAEL Y
Genome Diversity of Spore-Forming Firmicutes MICHAEL Y. GALPERIN National Center for Biotechnology Information, National Library of Medicine, National Institutes of Health, Bethesda, MD 20894 ABSTRACT Formation of heat-resistant endospores is a specific Vibrio subtilis (and also Vibrio bacillus), Ferdinand Cohn property of the members of the phylum Firmicutes (low-G+C assigned it to the genus Bacillus and family Bacillaceae, Gram-positive bacteria). It is found in representatives of four specifically noting the existence of heat-sensitive vegeta- different classes of Firmicutes, Bacilli, Clostridia, Erysipelotrichia, tive cells and heat-resistant endospores (see reference 1). and Negativicutes, which all encode similar sets of core sporulation fi proteins. Each of these classes also includes non-spore-forming Soon after that, Robert Koch identi ed Bacillus anthracis organisms that sometimes belong to the same genus or even as the causative agent of anthrax in cattle and the species as their spore-forming relatives. This chapter reviews the endospores as a means of the propagation of this orga- diversity of the members of phylum Firmicutes, its current taxon- nism among its hosts. In subsequent studies, the ability to omy, and the status of genome-sequencing projects for various form endospores, the specific purple staining by crystal subgroups within the phylum. It also discusses the evolution of the violet-iodine (Gram-positive staining, reflecting the pres- Firmicutes from their apparently spore-forming common ancestor ence of a thick peptidoglycan layer and the absence of and the independent loss of sporulation genes in several different lineages (staphylococci, streptococci, listeria, lactobacilli, an outer membrane), and the relatively low (typically ruminococci) in the course of their adaptation to the saprophytic less than 50%) molar fraction of guanine and cytosine lifestyle in a nutrient-rich environment. -

Ureaplasma Urealyticum and U. Parvum in Sexually Active Women Attending Public Health Clinics in Brazil
Epidemiol. Infect. (2017), 145, 2341–2351. © Cambridge University Press 2017 doi:10.1017/S0950268817001145 Ureaplasma urealyticum and U. parvum in sexually active women attending public health clinics in Brazil T. N. LOBÃO1,G.B.CAMPOS1,2,N.N.SELIS2,A.T.AMORIM1,S.G.SOUZA2, S. S. MAFRA2,L.S.PEREIRA2,D.B.DOSSANTOS3,T.B.FIGUEIREDO2, 1,2 1 L. M. MARQUES * AND J. TIMENETSKY 1 Instituto de Ciências Biomédicas, Departamento de Microbiologia, Universidade de São Paulo, Brazil 2 Instituto Multidisciplinar em Saúde, Núcleo de Tecnologia em Saúde, Universidade Federal da Bahia, Brazil 3 Centro de Ciências da Saúde, Universidade Federal do Recôncavo Baiano, Instituto de Ciências Biomédicas, Av. Professor Lineu Prestes, 1374. CEP 05508900, São Paulo, SP, Brazil Received 15 June 2016; Final revision 5 May 2017; Accepted 16 May 2017; first published online 22 June 2017 SUMMARY Ureaplasma urealyticum and U. parvum have been associated with genital infections. The purpose of this study was to detect the presence of ureaplasmas and other sexually transmitted infections in sexually active women from Brazil and relate these data to demographic and sexual health, and cytokines IL-6 and IL-1β. Samples of cervical swab of 302 women were examined at the Family Health Units in Vitória da Conquista. The frequency of detection by conventional PCR was 76·2% for Mollicutes. In qPCR, the frequency found was 16·6% for U. urealyticum and 60·6% U. parvum and the bacterial load of these microorganisms was not significantly associated with signs and symptoms of genital infection. The frequency found for Trichomonas vaginalis, Neisseria gonorrhoeae, Gardnerella vaginalis and Chlamydia trachomatis was 3·0%, 21·5%, 42·4% and 1·7%, respectively. -

Roles of the Vagina and the Vaginal Microbiota in Urinary Tract Infection: Evidence from Clinical Correlations and Experimental Models
Washington University School of Medicine Digital Commons@Becker Open Access Publications 1-1-2020 Roles of the vagina and the vaginal microbiota in urinary tract infection: Evidence from clinical correlations and experimental models Amanda L Lewis Nicole M Gilbert Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Urogenital infections and inflammations OPEN ACCESS Review Article Roles of the vagina and the vaginal microbiota in urinary tract infection: evidence from clinical correlations and experimental models Abstract Mounting evidence indicates that the vagina can harbor uropathogenic Amanda L. Lewis1,2,3 bacteria. Here, we consider three roles played by the vagina and its Nicole M. Gilbert2,3,4 bacterial inhabitants in urinary tract infection (UTI) and urinary health. First, the vagina can serve as a reservoir for Escherichia coli, the most common cause of UTI, and other recognized uropathogens. Second, 1 Molecular Microbiology, several vaginal bacterial species are frequently detected upon urine Washington University School culture but are underappreciated as uropathogens, and other vaginal of Medicine in Saint Louis, species are likely under-reported because of their fastidious nature. United States Third, some vaginal bacteria that are not widely viewed as uropathogens 2 Obstetrics and Gynecology, can transit briefly in the urinary tract, cause injury or immunomodulation, Washington University School and shift the balance of host-pathogen interactions to influence the of Medicine in Saint Louis, outcomes of uropathogenesis. This chapter describes the current liter- United States ature in these three areas and summarizes the impact of the vaginal 3 Center for Women's microbiota on susceptibility to UTI and other urologic conditions. -

Moving Beyond Serovars
ABSTRACT Title of Document: MOLECULAR AND BIOINFORMATICS APPROACHES TO REDEFINE OUR UNDERSTANDING OF UREAPLASMAS: MOVING BEYOND SEROVARS Vanya Paralanov, Doctor of Philosophy, 2014 Directed By: Prof. Jonathan Dinman, Cell Biology and Molecular Genetics, University of Maryland College Park Prof. John I. Glass, Synthetic Biology, J. Craig Venter Institute Ureaplasma parvum and Ureaplasma urealyticum are sexually transmitted, opportunistic pathogens of the human urogenital tract. There are 14 known serovars of the two species. For decades, it has been postulated that virulence is related to serotype specificity. Understanding of the role of ureaplasmas in human diseases has been thwarted due to two major barriers: (1) lack of suitable diagnostic tests and (2) lack of genetic manipulation tools for the creation of mutants to study the role of potential pathogenicity factors. To address the first barrier we developed real-time quantitative PCRs (RT-qPCR) for the reliable differentiation of the two species and 14 serovars. We typed 1,061 ureaplasma clinical isolates and observed about 40% of isolates to be genetic mosaics, arising from the recombination of multiple serovars. Furthermore, comparative genome analysis of the 14 serovars and 5 clinical isolates showed that the mba gene, used for serotyping ureaplasmas was part of a large, phase variable gene system, and some serovars shown to express different MBA proteins also encode mba genes associated with other serovars. Together these data suggests that differential pathogenicity and clinical outcome of an ureaplasmal infection is most likely due to the presence or absence of potential pathogenicity factors in individual ureaplasma clinical isolates and/or patient to patient differences in terms of autoimmunity and microbiome. -

Cryptic Inoviruses Revealed As Pervasive in Bacteria and Archaea
Cryptic inoviruses revealed as pervasive in bacteria and archaea across Earth’s biomes Simon Roux, M Krupovic, Rebecca Daly, Adair Borges, Stephen Nayfach, Frederik Schulz, Allison Sharrar, Paula Matheus Carnevali, Jan-Fang Cheng, Natalia Ivanova, et al. To cite this version: Simon Roux, M Krupovic, Rebecca Daly, Adair Borges, Stephen Nayfach, et al.. Cryptic inoviruses revealed as pervasive in bacteria and archaea across Earth’s biomes. Nature Microbiology, Nature Publishing Group, 2019, 4 (11), pp.1895-1906. 10.1038/s41564-019-0510-x. pasteur-02557242 HAL Id: pasteur-02557242 https://hal-pasteur.archives-ouvertes.fr/pasteur-02557242 Submitted on 28 Apr 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Distributed under a Creative Commons Attribution| 4.0 International License ARTICLES https://doi.org/10.1038/s41564-019-0510-x Cryptic inoviruses revealed as pervasive in bacteria and archaea across Earth’s biomes Simon Roux 1*, Mart Krupovic 2, Rebecca A. Daly3, Adair L. Borges4, Stephen Nayfach1, Frederik Schulz 1, Allison Sharrar5, Paula B. Matheus Carnevali 5, Jan-Fang Cheng1, Natalia N. Ivanova 1, Joseph Bondy-Denomy4,6, Kelly C. Wrighton3, Tanja Woyke 1, Axel Visel 1, Nikos C. -
Advances in PCR Based Detection of Mycoplasmas Contaminating Cell Cultures
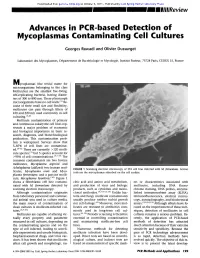
Downloaded from genome.cshlp.org on October 6, 2021 - Published by Cold Spring Harbor Laboratory Press Advances in PCR based Detection of Mycoplasmas Contaminating Cell Cultures Georges Rawadi and Olivier Dussurget Laboratoire des Mycoplasmes, D~partement de Bact&iologie et Mycologie, Institut Pasteur, 75724 Paris, CEDEX 15, France M ycoplasmas (the trivial name for microorganisms belonging to the class Mollicutes) are the smallest free-living, self-replicating bacteria, having diame- ters of 300 to 800 nm. These pleomorph microorganisms have no cell walls. (1~ Be- cause of their small size and flexibility, mollicutes can pass through filters of 450 and 220 nm used commonly in cell culturing. ~,2) Mollicute contamination of primary and continuous eukaryotic cell lines rep- resents a major problem of economic and biological importance in basic re- search, diagnosis, and biotechnological production. This contamination prob- lem is widespread. Surveys show that 5-87% of cell lines are contaminat- ed. (3-6~ There are currently ~120 molli- cute species, (~ but 5 species account for ~>95% of cell contaminations. (3'7-9~ The common contaminants are two bovine mollicutes, Mycoplasma arginini and Acholeplasma laidlawii; two human mol- FIGURE 1 Scanning electron microscopy of 3T6 cell line infected with M. fermentans. Arrows licutes, Mycoplasma orale and Myco- indicate the mycoplasmas adsorbed on the cell surface. plasma fermentans; and a porcine molli- cute, Mycoplasma hyorhinis. (1~ Figure 1 shows a fibroblastic cell line contami- cleic acid and amino acid metabolism, ers or characteristics associated with nated with M. fermentans detected by and production of virus and biologic mollicutes, including DNA fluoro- scanning electron microscopy.