Triple Whammy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Angiotensin-Converting Enzyme Inhibitors Or Angiotensin II Receptor Blockers and the Risk of Developing Rheumatoid Arthritis in Antihypertensive Drug Users
Jong, H.J.I. de, Vandebriel, R.J., Saldi, S.R.F., Dijk, L. van, Loveren, H. van, Cohen Tervaert, J.W., Klungel, O.H. Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers and the risk of developing rheumatoid arthritis in antihypertensive drug users. Pharmacoepidemiology and Drug Safety: 2012, 21(8), 835-843 Postprint Version 1.0 Journal website http://dx.doi.org/10.1002/pds.3291 Pubmed link http://www.ncbi.nlm.nih.gov/pubmed/22674737 DOI 10.1002/pds.3291 This is a NIVEL certified Post Print, more info at http://www.nivel.eu Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers and the risk of developing rheumatoid arthritis in antihypertensive drug users†‡ HILDA J. I. DE JONG1,2,3, ROB J. VANDEBRIEL1, SITI R. F. SALDI3, LISET VAN DIJK4, HENK VAN LOVEREN1,2, JAN WILLEM COHEN TERVAERT5, OLAF H. KLUNGEL3,* ABSTRACT Purpose: Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) are effective in the treatment of cardiovascular disease. Next to effects on hypertension and cardiac function, these drugs have anti-inflammatory and immunomodulating properties which may either facilitate or protect against the development of autoimmunity, potentially resulting in autoimmune diseases. Therefore, we determined in the current study the association between ACE inhibitor and ARB use and incident rheumatoid arthritis (RA). Methods: A matched case–control study was conducted among patients treated with antihypertensive drugs using the Netherlands Information Network of General Practice (LINH) database in 2001–2006. Cases were patients with a first-time diagnosis of RA. Each case was matched to five controls for age, sex, and index date, which was selected 1 year before the first diagnosis of RA. -

Ace Inhibitors (Angiotensin-Converting Enzyme)
Medication Instructions Ace Inhibitors (Angiotensin-Converting Enzyme) Generic Brand Benazepril Lotensin Captopril Capoten Enalapril Vasotec Fosinopril Monopril Lisinopril Prinivil, Zestril Do not Moexipril Univasc Quinapril Accupril stop taking Ramipril Altace this medicine Trandolapril Mavik About this Medicine unless told ACE inhibitors are used to treat both high blood pressure (hypertension) and heart failure (HF). They block an enzyme that causes blood vessels to constrict. This to do so allows the blood vessels to relax and dilate. Untreated, high blood pressure can damage to your heart, kidneys and may lead to stroke or heart failure. In HF, using by your an ACE inhibitor can: • Protect your heart from further injury doctor. • Improve your health • Reduce your symptoms • Can prevent heart failure. Generic forms of ACE Inhibitors (benazepril, captopril, enalapril, fosinopril, and lisinopril) may be purchased at a lower price. There are no “generics” for Accupril, Altace Mavik, and of Univasc. Thus their prices are higher. Ask your doctor if one of the generic ACE Inhibitors would work for you. How to Take Use this drug as directed by your doctor. It is best to take these drugs, especially captopril, on an empty stomach one hour before or two hours after meals (unless otherwise instructed by your doctor). Side Effects Along with needed effects, a drug may cause some unwanted effects. Many people will not have any side effects. Most of these side effects are mild and short-lived. Check with your doctor if any of the following side effects occur: • Fever and chills • Hoarseness • Swelling of face, mouth, hands or feet or any trouble in swallowing or breathing • Dizziness or lightheadedness (often a problem with the first dose) Report these side effects if they persist: • Cough – dry or continuing • Loss of taste, diarrhea, nausea, headache or unusual fatigue • Fast or irregular heartbeat, dizziness, lightheadedness • Skin rash Special Guidelines • Sodium in the diet may cause you to retain fluid and increase your blood pressure. -

Deprescribing for Older Patients
CMAJ Review CME Deprescribing for older patients Christopher Frank MD, Erica Weir MD MSc See related editorial at www.cmaj.ca/lookup/doi:10.1503/cmaj.122099 and articles at www.cmaj.ca/lookup/doi:10.1503/cmaj.122012 and www.cmaj.ca/lookup/doi:10.1503/cmaj.130523 he principles that guide optimal prescribing outcomes related to medications than other older Competing interests: None for older patients1,2 (Box 1) include depre- patients. They are also more likely to have limited declared. scribing medications that are no longer indi- life expectancy than well older people of similar This article has been peer T 17 cated, appropriate or aligned with evolving goals of age. Medication lists tend to lengthen as patients reviewed. care. Deprescribing is a relatively new term that age, and there are few guidelines to inform medi- Correspondence to: focuses attention on the sometimes overlooked step cation management in the context of polyphar- Christopher Frank, frankc in medication review of stopping medications to macy, multiple morbidities and age-related @providencecare.ca improve outcomes and decrease risks associated changes to pharmacokinetics and pharmacody- CMAJ 2014. DOI:10.1503 with polypharmacy in older people.3–5 These risks namics (Box 1). All prescribers contributing to the /cmaj.131873 include nonadherence,6 adverse drug reactions,7 medication list need to be alert to “prescribing functional and cognitive decline,8 and falls.9,10 In inertia”18 (the tendency to automatically renew a Canada, more than 50% of older people living in medication even when the original indication is long-term care facilities and 27% of those living in no longer present) and should view polypharmacy the community take more than five medications a as an impetus to deprescribe when appropriate. -

Icatibant Compared to Steroids and Antihistamines for ACE-Inhibitor-Induced Angioedema
KNOWLEDGE TO PRACTICE DES CONNAISSANCES ÀLA PRATIQUE CJEM Journal Club Icatibant Compared to Steroids and Antihistamines for ACE-Inhibitor-Induced Angioedema Reviewed by: Tudor Botnaru, MD, CM*; Antony Robert, MD, MASc*; Salvatore Mottillo, MD, MSc* syndromes, and acute heart failure NYHA class III or Article chosen IV,aswellasthosepregnantandlactating,were Bas M, Greve J, Stelter K, et al. A Randomized Trial of excluded. Icatibant in ACE-Inhibitor-Induced Angioedema. N Engl J Med 2015;372:418-25. doi:10.1056/NEJMoa1312524. STUDY DESIGN This was an industry and government funded, multi-centre, Keywords: angioedema, icatibant, corticosteroids, ACE-inhibitor, antihistamines double-blind, double-dummy randomized phase 2 study. Block randomization was performed online. Patients were randomly assigned in a 1:1 ratio. Primary investigators and BACKGROUND patients were blinded to the treatment. Investigators who were responsible for the randomization, study-drug administration, and assessment of injection site reactions Angiotensin-converting-enzyme-inhibitor (ACEI) induced were aware of study assignments. Patients in the treatment angioedema occurs in 0.68% of those taking the group received icatibant 30 mg subcutaneously and those in medication1 and accounts for one-third of angioedema the control group (standard therapy group) received pre- cases treated in the emergency department. Upper airway dnisolone 500 mg and clemastine 2 mg (an antihistamine) compromise, potentially leading to acute laryngeal intravenously. Patients assessed the intensity of symptoms obstruction and death, may occur in up to 10% of cases.1,2 at several intervals within 48 hours. Blinded investigators Standard therapy consists of glucocorticoids and anti- further assessed the signs and symptoms. If there was no histamines. -

Angiotensin Modulators/Calcium Channel Blocker Combinations Review 02/05/2009
Angiotensin Modulators/Calcium Channel Blocker Combinations Review 02/05/2009 Copyright © 2004 - 2009 by Provider Synergies, L.L.C. All rights reserved. Printed in the United States of America. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage and retrieval system without the express written consent of Provider Synergies, L.L.C. All requests for permission should be mailed to: Attention: Copyright Administrator Intellectual Property Department Provider Synergies, L.L.C. 5181 Natorp Blvd., Suite 205 Mason, Ohio 45040 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Comments and suggestions may be sent to [email protected]. -

Effect of Exogenous Glucocorticoid on Osmotically Stimulated Antidiuretic
European Journal of Endocrinology (2006) 155 845–848 ISSN 0804-4643 CLINICAL STUDY Effect of exogenous glucocorticoid on osmotically stimulated antidiuretic hormone secretion and on water reabsorption in man Volker Ba¨hr1, Norma Franzen1, Wolfgang Oelkers2, Andreas F H Pfeiffer1 and Sven Diederich1,2 1Department of Endocrinology, Diabetes and Nutrition, Charite-Universitatsmedizin Berlin, Campus Benjamin Franklin, Hindenburgdamm 30, 12200 Berlin, Germany and 2Endokrinologikum Berlin, Centre for Endocrine and Metabolic Diseases, Berlin, Germany (Correspondence should be addressed to V Ba¨hr; Email: [email protected]) Abstract Objective: Glucocorticoids exert tonic suppression of antidiuretic hormone (ADH) secretion. Hypocortisolism in secondary adrenocortical insufficiency can result in a clinical picture similar to the syndrome of inappropriate ADH secretion. On the other hand, in vitro and in vivo results provide evidence for ADH suppression in states of hypercortisolism. To test the hypothesis that ADH suppression is of relevance during glucocorticoid therapy, we investigated the influence of prednisolone on the osmotic stimulation of ADH. Design and methods: Seven healthy men were subjected to water deprivation tests with the measurement of plasma ADH (pADH) and osmolality (posmol) before and after glucocorticoid treatment (5 days 30 mg prednisolone per day). Results: Before glucocorticoid treatment, the volunteers showed a normal test with an adequate increase of pADH (basal 0.54G0.2 to 1.9G0.72 pg/ml (meanGS.D.)) in relation to posmol(basal 283.3G8.5 to 293.7G6 mosmol/kg). After prednisolone intake, pADH was attenuated (!0.4 pg/ml) in spite of an increase of posmol from 289.3G3.6 to 297.0G5.5 mosmol/kg. -

Angiotensin-Converting Enzyme (ACE) Inhibitors
Angiotensin-Converting Enzyme (ACE) Inhibitors Summary Blood pressure reduction is similar for the ACE inhibitors class, with no clinically meaningful differences between agents. Side effects are infrequent with ACE inhibitors, and are usually mild in severity; the most commonly occurring include cough and hypotension. Captopril and lisinopril do not require hepatic conversion to active metabolites and may be preferred in patients with severe hepatic impairment. Captopril differs from other oral ACE inhibitors in its rapid onset and shorter duration of action, which requires it to be given 2-3 times per day; enalaprilat, an injectable ACE inhibitor also has a rapid onset and shorter duration of action. Pharmacology Angiotensin Converting Enzyme Inhibitors (ACE inhibitors) block the conversion of angiotensin I to angiotensin II through competitive inhibition of the angiotensin converting enzyme. Angiotensin is formed via the renin-angiotensin-aldosterone system (RAAS), an enzymatic cascade that leads to the proteolytic cleavage of angiotensin I by ACEs to angiotensin II. RAAS impacts cardiovascular, renal and adrenal functions via the regulation of systemic blood pressure and electrolyte and fluid balance. Reduction in plasma levels of angiotensin II, a potent vasoconstrictor and negative feedback mediator for renin activity, by ACE inhibitors leads to increased plasma renin activity and decreased blood pressure, vasopressin secretion, sympathetic activation and cell growth. Decreases in plasma angiotensin II levels also results in a reduction in aldosterone secretion, with a subsequent decrease in sodium and water retention.[51035][51036][50907][51037][24005] ACE is found in both the plasma and tissue, but the concentration appears to be greater in tissue (primarily vascular endothelial cells, but also present in other organs including the heart). -

Beta-Blockers for Hypertension: Time to Call a Halt
Journal of Human Hypertension (1998) 12, 807–810 1998 Stockton Press. All rights reserved 0950-9240/98 $12.00 http://www.stockton-press.co.uk/jhh FOR DEBATE Beta-blockers for hypertension: time to call a halt DG Beevers University Department of Medicine, City Hospital, Birmingham B18 7QH, UK Beta-blockers are not very effective at lowering blood the endorsement of beta-blockers by the British Hyper- pressure in elderly hypertensive patients or in Afro- tension Society and other guidelines committees, Caribbeans and these two groups represent a large pro- except possibly for severe resistant hypertension, high portion of people with raised blood pressure. Further- risk post-infarct patients and those with angina pectoris. more they do not prevent more heart attacks than the The time has come to move across to newer, safer, more thiazide diuretics. Beta-blockers can also be dangerous tolerable and more effective antihypertensive agents in many hypertensive patients and even when these whilst continuing to use thiazide diuretics in low doses drugs are not contraindicated, they cause subtle and in the elderly as first choice, providing there are no depressing side effects which should preclude their contraindications. usefulness. The time has come therefore to reconsider Keywords: beta-blockers; hypertension Introduction Safety and tolerability Beta-adrenergic blockers were first introduced in the There is little doubt that the beta-blockers are the early 1960s for the treatment of angina pectoris. most unsafe of all antihypertensive drugs. They can Their antihypertensive properties were not fully precipitate or worsen heart failure in patients with recognised until the celebrated paper by Pritchard myocardial damage and they are contraindicated in and Gillam in 1964.1 They rapidly became popular patients with asthma. -

Effects of Statins on Renin–Angiotensin System
Journal of Cardiovascular Development and Disease Review Effects of Statins on Renin–Angiotensin System Nasim Kiaie 1,†, Armita Mahdavi Gorabi 1,†, Željko Reiner 2, Tannaz Jamialahmadi 3,4, Massimiliano Ruscica 5 and Amirhossein Sahebkar 6,7,8,9,* 1 Research Center for Advanced Technologies in Cardiovascular Medicine, Tehran Heart Center, Tehran University of Medical Sciences, Tehran 1411713138, Iran; [email protected] (N.K.); [email protected] (A.M.G.) 2 Department of Internal Diseases, School of Medicine, University Hospital Center Zagreb, Zagreb University, 10000 Zagreb, Croatia; [email protected] 3 Quchan Branch, Department of Food Science and Technology, Islamic Azad University, Quchan 9479176135, Iran; [email protected] 4 Department of Nutrition, Mashhad University of Medical Sciences, Mashhad 9177948564, Iran 5 Department of Pharmacological and Biomolecular Sciences, Università degli Studi di Milano, 20133 Milan, Italy; [email protected] 6 Biotechnology Research Center, Pharmaceutical Technology Institute, Mashhad University of Medical Sciences, Mashhad 9177948564, Iran 7 Applied Biomedical Research Center, Mashhad University of Medical Sciences, Mashhad 9177948564, Iran 8 School of Medicine, The University of Western Australia, Perth 6009, Australia 9 School of Pharmacy, Mashhad University of Medical Sciences, Mashhad 9177948564, Iran * Correspondence: [email protected] or [email protected] † Equally contributed. Abstract: Statins, a class of drugs for lowering serum LDL-cholesterol, have attracted attention because of their wide range of pleiotropic effects. An important but often neglected effect of statins is their role in the renin–angiotensin system (RAS) pathway. This pathway plays an integral role in the progression of several diseases including hypertension, heart failure, and renal disease. -
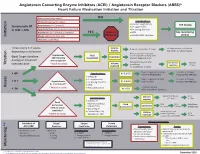
Initiation Titration Assess Monitoring **
Angiotensin Converting Enzyme Inhibitors (ACEI) / Angiotensin Receptor Blockers (ARBS)* Heart Failure Medication Initiation and Titration Bilateral renal artery stenosis NO Moderate/Severe aortic stenosis Considerations: • Baseline cough (ACEi) Hyperkalemia: K+ > 5.2 mmol/L See dosing Symptomatic HF • K+ supplements or LVEF < 40% Renal Dysfunction:Serum creatinine >220 µmol/L • K+ sparing diuretics Hypotension: SBP < 90 mmHg or symptoms YES Refer to • MRA See monitoring Initiation Allergy: angioedema, hives, rash Physician • NSAIDS/COX2 inhibitors section Intolerance: cough (ACEi) Titrate every 1-3 weeks, Volume Reduce/hold diuretic x 2-3 days No improvement, hold/reduce depending on tolerance deplete ACEI/ARB x 1-2 wks & reassess Reassess diuretic dose/other Hypotension Fluid non-essential BP lowering meds Goal: Target dose(see Euvolemic SBP<90mmHg Assessment Consider staggering doses dosing) or maximum with symptoms* Reduce/hold dose of other See Diuretic Reassess Titration * Watch for trends Volume tolerated dose vasodilators algorithm 1-2 wks overload +/- ACEI/ARB x 1-2 weeks Stop K+ supplements, reduce/ Serum K+ in 3-5 days, Considerations: • BP K+ 5.2-5.5 hold MRA (if applicable) Reassess ACEI/ARB dose • Dietary K+ • K+ supplements Stop K+ supplements, MRA. Serum K+ in 2-3 days, • K + Hyperkalemia • K+ sparing diuretics K+ 5.6-6.0 hold ACEI/ARB Reassess ACEI/ARB dose K+ > 5.2 mmol/L* • MRA Assess * Watch for trends • Renal dysfunction Treat hyperkalemia • Scr K+ > 6.0 Refer to MD/NP +/- send to ED Reduce/hold diuretic Scr in Considerations: -

Energy Drinks 800.232.4424 (Voice/TTY) 860.793.9813 (Fax)
Caffeine and Energy Boosting Drugs: Energy Drinks 800.232.4424 (Voice/TTY) 860.793.9813 (Fax) www.ctclearinghouse.org A Library and Resource Center on Alcohol, Tobacco, Other Drugs, Mental Health and Wellness What are energy drinks? you. You wouldn't use Mountain Dew as a sports Energy drinks are beverages like drink. And a drink like Red Bull and vodka is Red Bull, Venom, Adrenaline Rush, more like strong coffee and whisky than 180, ISO Sprint, and Whoopass, anything else. which contain large doses of caffeine and other legal stimulants What happens when energy drinks are like ephedrine, guarana, and ginseng. combined with alcohol? Energy drinks may contain as much as 80 mg. Energy drinks are also used as mixers with of caffeine, the equivalent of a cup of coffee. alcohol. This combination carries a number of Compared to the 37 mg. of caffeine in a dangers: Mountain Dew, or the 23 mg. in a Coca-Cola Classic, that's a big punch. These drinks are • Since energy drinks are stimulants and marketed to people under 30, especially to alcohol is a depressant, the combination of college students, and are widely available both effects may be dangerous. The stimulant on and off campus. effects can mask how intoxicated you are and prevent you from realizing how much Are there short-term dangers to drinking alcohol you have consumed. Fatigue is one energy drinks? of the ways the body normally tells Individual responses to caffeine vary, and someone that they've had enough to drink. these drinks should be treated carefully • The stimulant effect can give the person the because of how powerful they are. -

Online Appendix
The More We Die, The More We Sell? A Simple Test of the Home-Market Effect Online Appendix Arnaud Costinot Dave Donaldson MIT, CEPR, and NBER MIT, CEPR, and NBER Margaret Kyle Heidi Williams Mines ParisTech and CEPR MIT and NBER December 28, 2018 1 Contents A Theoretical Appendix3 A.1 Multinational Enterprises (Section III.1)..........................3 A.2 Log-Linearization (Section III.2)...............................3 A.3 Beyond Perfect Competition (Section III.3).........................6 A.3.1 Monopolistic Competition..............................6 A.3.2 Variable Markups...................................7 A.3.3 Endogenous Innovation...............................8 A.3.4 Price Regulations...................................9 A.4 Bilateral Sales (Section VI.1)................................. 12 B Empirical Appendix 12 B.1 Rich versus Poor Countries................................. 12 B.2 Additional Empirical Results................................ 13 B.3 Benchmarking IMS MIDAS data.............................. 13 B.3.1 Benchmarking to the OECD HealthStat Data................... 13 B.3.2 Benchmarking to the MEPS Data.......................... 14 B.4 ATC to GBD Mapping.................................... 15 2 A Theoretical Appendix A.1 Multinational Enterprises (Section III.1) In this appendix, we illustrate how to incorporate multinational production into our basic envi- ronment. Following Ramondo and Rodríguez-Clare(2013), suppose that each firm headquartered in country i that sells drugs targeting disease n in country j 6= i can choose the country l in which its production takes place. If l = i, then the firm exports, if l = j, it engages in horizontal FDI, and if l 6= i, j, it engages in platform FDI. Like in Ramondo and Rodríguez-Clare(2013), we assume that firm-level production functions exhibit constant returns to scale, but we further allow for external economies of scale at the level of the headquarter country for each disease.