The IL4I1 Enzyme: a New Player in the Immunosuppressive Tumor Microenvironment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Myeloid and Tubular Epithelial Cells Shape Renal Innate Immunity
Am J Physiol Renal Physiol 304: F1243–F1251, 2013. First published March 20, 2013; doi:10.1152/ajprenal.00101.2013. Review Sisters in arms: myeloid and tubular epithelial cells shape renal innate immunity Takashi Hato, Tarek M. El-Achkar, and Pierre C. Dagher Department of Medicine, Indiana University, Indianapolis, Indiana Submitted 19 February 2013; accepted in final form 13 March 2013 Hato T, El-Achkar TM, Dagher PC. Sisters in arms: myeloid and tubular epithelial cells shape renal innate immunity. Am J Physiol Renal Physiol 304: F1243– F1251, 2013. First published March 20, 2013; doi:10.1152/ajprenal.00101.2013.—The importance of innate immunity for survival is underscored by its presence at almost every level of the evolutionary tree of life. The task of “danger” recognition by the Downloaded from innate immune system is carried out by a broad class of pattern recognition receptors. These receptors are expressed in both hematopoietic and nonhematopoi- etic cells such as renal epithelial cells. Upon activation, pattern recognition receptors induce essentially two types of defensive responses: inflammation and phagocytosis. In this review, we highlight evidence that renal epithelial cells are endowed with such defensive capabilities and as such fully participate in renal innate immune responses. http://ajprenal.physiology.org/ epithelial cells; innate immunity; pattern recognition receptors; Toll-like receptor; endotoxin THE FUNDAMENTAL ROLE OF THE innate immune system is to primarily focus on the less explored “innate immune cells”, initiate a quick response immediately after detecting “danger i.e., renal epithelial cells. signals” in the setting of infection (nonself) or tissue injury (self). -

Theory Revolution? Doubts About The
Cutting Edge Commentary: A Copernican Revolution? Doubts About the Danger Theory This information is current as Russell E. Vance of September 29, 2021. J Immunol 2000; 165:1725-1728; ; doi: 10.4049/jimmunol.165.4.1725 http://www.jimmunol.org/content/165/4/1725 Downloaded from References This article cites 42 articles, 11 of which you can access for free at: http://www.jimmunol.org/content/165/4/1725.full#ref-list-1 Why The JI? Submit online. http://www.jimmunol.org/ • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average by guest on September 29, 2021 Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2000 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. ● Cutting Edge Commentary: A Copernican Revolution? Doubts About the Danger Theory1 Russell E. Vance2 What Is the Danger Theory? The immune system is often said to function by “self-nonself” Although the notion that the immune system has evolved to rec- discrimination. Recently, some have argued that it actually de- ognize (dangerous) pathogens is not new (15), recent discussions tects “danger” or “strangers.” There are problems with all of of “danger” have revolved around one particular characterization these points of view. -

Cognitive and Memory Functions in Plant Immunity
Review Cognitive and Memory Functions in Plant Immunity Hidetaka Yakura Institute for Science and Human Existence, Tokyo 163-8001, Japan; [email protected] Received: 5 August 2020; Accepted: 16 September 2020; Published: 17 September 2020 Abstract: From the time of Thucydides in the 5th century BC, it has been known that specific recognition of pathogens and memory formation are critical components of immune functions. In contrast to the immune system of jawed vertebrates, such as humans and mice, plants lack a circulatory system with mobile immune cells and a repertoire of clonally distributed antigen receptors with almost unlimited specificities. However, without these systems and mechanisms, plants can live and survive in the same hostile environment faced by other organisms. In fact, they achieve specific pathogen recognition and elimination, with limited self-reactivity, and generate immunological memory, sometimes with transgenerational characteristics. Thus, the plant immune system satisfies minimal conditions for constituting an immune system, namely, the recognition of signals in the milieu, integration of that information, subsequent efficient reaction based on the integrated information, and memorization of the experience. In the previous report, this set of elements was proposed as an example of minimal cognitive functions. In this essay, I will first review current understanding of plant immunity and then discuss the unique features of cognitive activities, including recognition of signals from external as well as internal environments, autoimmunity, and memory formation. In doing so, I hope to reach a deeper understanding of the significance of immunity omnipresent in the realm of living organisms. Keywords: autoimmunity; cognition; metaphysicalization; plant immunity; transgenerational memory 1. -

Systemic Features of Immune Recognition
PhD degree in Foundations of the Life Sciences and their Ethical Consequences European School of Molecular Medicine (SEMM) and University of Milan Faculty of Medicine Settore disciplinare: FIL/2 SYSTEMIC FEATURES OF IMMUNE RECOGNITION Bartlomiej Swiatczak IFOM-IEO Campus, Milan Matricola n. R07404 Supervisor: Prof. Mark Bedau Visiting Professor IFOM-IEO Campus, Milan Anno accademico 2010-2011 1 Acknowledgements I would like to express my sincere gratitude to my supervisor Professor Mark Bedau for his invaluable encouragement and guidance. I could not have imagined having a better advisor and a mentor for my PhD. Without his constant support and patience I would never have finished this work. I owe many thanks to my second supervisor, Professor Irun Cohen for being a constant source of inspiration and for many useful discussions. I am also grateful to my laboratory supervisor, Doctor Maria Rescigno for support and useful criticisms during my PhD. I would also like to thank Professor John Dupré and Doctor Stefano Casola for their very constructive input in developing this thesis. I also extend my gratitude to the coordinators of the FOLSATEC program, Professor Giovanni Boniolo and Doctor Giuseppe Testa for their continuous encouragement throughout these years. 2 Table of contents List of Abbreviations……………………………………………………………………. 6 Figure index……………………………………………………………………………... 9 Author’s declaration…………………………………………………………………….. 10 Abstract………………………………………………………………………………….. 11 Introduction……………………………………………………………………………… 12 Part 1. Immune recognition as an integrated activity of cells and molecules….…. 16 Single types of cells and molecules cannot distinguish between pathogenic 17 and non-pathogenic microbes………………………………………………… Single types of cells and molecules, in principle, cannot recognize pathogens………………………………..…………………………...……….. 24 Return to basics: What makes a pathogen a pathogen?.................................... -
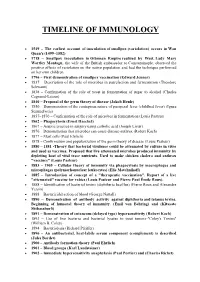
Timeline of Immunology
TIMELINE OF IMMUNOLOGY 1549 – The earliest account of inoculation of smallpox (variolation) occurs in Wan Quan's (1499–1582) 1718 – Smallpox inoculation in Ottoman Empire realized by West. Lady Mary Wortley Montagu, the wife of the British ambassador to Constantinople, observed the positive effects of variolation on the native population and had the technique performed on her own children. 1796 – First demonstration of smallpox vaccination (Edward Jenner) 1837 – Description of the role of microbes in putrefaction and fermentation (Theodore Schwann) 1838 – Confirmation of the role of yeast in fermentation of sugar to alcohol (Charles Cagniard-Latour) 1840 – Proposal of the germ theory of disease (Jakob Henle) 1850 – Demonstration of the contagious nature of puerperal fever (childbed fever) (Ignaz Semmelweis) 1857–1870 – Confirmation of the role of microbes in fermentation (Louis Pasteur) 1862 – Phagocytosis (Ernst Haeckel) 1867 – Aseptic practice in surgery using carbolic acid (Joseph Lister) 1876 – Demonstration that microbes can cause disease-anthrax (Robert Koch) 1877 – Mast cells (Paul Ehrlich) 1878 – Confirmation and popularization of the germ theory of disease (Louis Pasteur) 1880 – 1881 -Theory that bacterial virulence could be attenuated by culture in vitro and used as vaccines. Proposed that live attenuated microbes produced immunity by depleting host of vital trace nutrients. Used to make chicken cholera and anthrax "vaccines" (Louis Pasteur) 1883 – 1905 – Cellular theory of immunity via phagocytosis by macrophages and microphages (polymorhonuclear leukocytes) (Elie Metchnikoff) 1885 – Introduction of concept of a "therapeutic vaccination". Report of a live "attenuated" vaccine for rabies (Louis Pasteur and Pierre Paul Émile Roux). 1888 – Identification of bacterial toxins (diphtheria bacillus) (Pierre Roux and Alexandre Yersin) 1888 – Bactericidal action of blood (George Nuttall) 1890 – Demonstration of antibody activity against diphtheria and tetanus toxins. -

Chapter 15 Self and Nonself Moira Howes
Chapter 15 Self and Nonself moira howes 1. Introduction Immunology is the science that investigates how organisms defend themselves against infection, harmful substances, and foreign tissue. In order for an organism to defend itself against such threats, however, its immune system presumably must be able to discriminate self from nonself. If the immune system could not make such a discrimina- tion, it might harm the organism it is to defend, rather than the microbes infecting it. Self–nonself discrimination thus appears to be a crucial function of the immune system. Indeed, immunology has been referred to as the “science of self–nonself discrimination” (Klein, 1982). How self–nonself discrimination is achieved depends, among other things, on whether an organism is an invertebrate or a jawed vertebrate. Self–nonself discrimina- tion is more rudimentary in invertebrates (and jawless fi shes) because their immune systems are “innate.” Innate immune mechanisms are those that do not change after repeated exposure to a given infectious agent; they do not learn. This contrasts with a type of immunity in jawed vertebrates – adaptive immunity – which does change after repeated exposure to pathogens. After the adaptive immune system adapts to a given pathogen, it can target the pathogen with greater precision and eliminate it more rapidly. Because of adaptive immunity, self–nonself discrimination in jawed vertebrates is specialized and precise: vertebrate immune systems are fi ne-tuned to differences between self and nonself. So signifi cant do immunologists fi nd the evolution of adaptive immunity – both with respect to enhanced pathogen defense and self–nonself discrimination – that some refer to it as the “immunological Big Bang” (Janeway & Travers, 2005). -

Thymus Epithelium Induces Tissue-Specific Tolerance by Adriana Bonomo and Polly Matzinger
Thymus Epithelium Induces Tissue-specific Tolerance By Adriana Bonomo and Polly Matzinger From the Laboratoryfor Cellular and Molecular Immunology, National Institute of Allergy and Infectious Disease, National Institutes of Health, Bethesda, Maryland 20892 Summary Most current models of T cell development include a positive selection step in the thymus that occurs when T cells interact with thymic epithelium and a negative selection step after encounters with bone marrow-derived cells. We show here that developing T cells are tolerized when they recognize antigens expressed by thymic epithelium, that the tolerance is tissue specific, and that it can occur by deletion of the reactive T cells. 't is generally believed that the primary role of the thymic profile). We reasoned that if the TE induces tolerance, it would I . epithelium (TE) 1 is to serve as an environment in which naturally tolerize only for the MHC-peptide complexes in- T cell precursors differentiate into mature T cells, as well as cluded in its own surface MAP, sparing T cells capable of to selectively promote maturation of those T cells deemed responding to the MAPs of other tissues. Since the strength to be "useful" by virtue of their affinity for self-MHC mole- of the response against any particular tissue would depend cules. Although the question of whether cells of the thymic on how its MAP overlapped with the MAP of the TE, many stroma also play a role in the induction of tolerance has been of the reported cases of split tolerance induced by TE might asked several times, the results have been diffcult to fit into actually be unrecognized cases of tissue-specific tolerance. -

Immunological Tolerance: Danger — Pathogen on the Premises! Charles A
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Dispatch 519 Immunological tolerance: Danger — pathogen on the premises! Charles A. Janeway Jr*, Christopher C. Goodnow† and Ruslan Medzhitov* Recent results show that immune responses can be lymphocytes, as infusing lymphocytes from a strain B induced in neonatal mice. Do they really refute the mouse immune to a strain A mouse led to skin graft rejec- traditional view that the ability to discriminate between tion. Surprisingly, normal strain B lymphocytes would not ‘self’ and ‘non-self’ is a fundamental property of the cause graft rejection, even though normal strain B mice immune system? can reject strain A skin [4]. These experiments can now be interpreted to mean that tolerance requires chimerism, the Addresses: *Section of Immunobiology, Yale University School of Medicine, New Haven, Connecticut 06510, USA. †Department of persistence of cells from the donor in the circulation of the Microbiology and Immunology, Stanford University Medical School, recipient; when donor cells are removed, the graft is Stanford, California 94305-5428, USA. rejected. This also indicates that tolerance is an ongoing process in adult mice. Current Biology 1996, Vol 6 No 5:519–522 © Current Biology Ltd ISSN 0960-9822 Many experiments in the 1950s, 1960s, and 1970s argued against Burnet and Medawar’s simple notion that toler- The March 22 issue of Science carried three articles [1–3] ance was acquired because of a special state of immune that claim to challenge a key principle of immunology, cells in utero and in neonates. -

The Pluripotent History of Immunology a Review
AVANT Volume III, Number 1/2012 www.avant.edu.pl/en 37 The pluripotent history of immunology A review Neeraja Sankaran History of Science, Technology & Medicine Underwood International College, Yonsei University, Seoul, S. Korea Abstract The historiography of immunology since 1999 is reviewed, in part as a response to claims by historians such as Thomas Söderqvist the field was still immature at the time (Söderqvist & Stillwell 1999). First addressed are the difficulties, past and present, surrounding the disciplinary definition of immunology, which is followed by a commentary on the recent scholarship devoted to the concept of the immune self. The new literature on broad immunological topics is examined and assessed, and specific charges leveled against the paucity of certain types of histories, e.g. biographical and institutional histories, are evaluated. In conclusion, there are compelling indications that the history of immunology has moved past the initial tentative stages identified in the earlier reviews to become a bustling, pluripotent discipline, much like the subject of its scrutiny, and that it continues to develop in many new and exciting directions. Keywords: Biographical history; Continuity model; Danger Model; Historiography of Immunology; History of Immunology; Institutional history; Self vs. Non-self model. Introduction Two decades ago, in the summer of 1992, the Naples Zoological Station’s summer school in the history of the life sciences, a roughly biennial event since the mid- 1970s, chose to focus on the history of immunology. Whether the meeting achieved its stated purpose of facilitating dialogue and exchange between immunologists and historians appears to have been a matter of some contention among the atten- dees (Judson & Mackay 1992; Söderqvist 1993). -

Narrative Immunities: the Logic of Infection and Defense in American Speculative Fiction
Western University Scholarship@Western Electronic Thesis and Dissertation Repository 1-9-2018 11:30 AM Narrative Immunities: The Logic of Infection and Defense in American Speculative Fiction Riley R. McDonald The University of Western Ontario Supervisor Schuster, Joshua The University of Western Ontario Joint Supervisor Carmichael, Thomas The University of Western Ontario Graduate Program in English A thesis submitted in partial fulfillment of the equirr ements for the degree in Doctor of Philosophy © Riley R. McDonald 2018 Follow this and additional works at: https://ir.lib.uwo.ca/etd Part of the American Literature Commons Recommended Citation McDonald, Riley R., "Narrative Immunities: The Logic of Infection and Defense in American Speculative Fiction" (2018). Electronic Thesis and Dissertation Repository. 5174. https://ir.lib.uwo.ca/etd/5174 This Dissertation/Thesis is brought to you for free and open access by Scholarship@Western. It has been accepted for inclusion in Electronic Thesis and Dissertation Repository by an authorized administrator of Scholarship@Western. For more information, please contact [email protected]. Abstract In this project I analyze the roles that notions of viruses and immunities and their figurations play within the narrative discourse of speculative fiction. Focusing on a series of texts from twentieth- and twenty-first century American fiction, I seek to examine the ways in which the dialectical confrontation between infection and immunity is explored, reified, or challenged on a narrative level. The terms “virus” and “immunity,” so intrinsic to life sciences, have come into use to describe specific micro-organisms and biological processes only within the last 150 years. Yet these terms possess a significantly longer history in political, legalistic, and philosophical discourses. -

Applying a Novel Immunological Concept to Intrusion Detection Systems
Poster Proceedings of ACDM 2004 Engineers’ House, Bristol, UK DETECTING DANGER: APPLYING A NOVEL IMMUNOLOGICAL CONCEPT TO INTRUSION DETECTION SYSTEMS Julie Greensmith, Uwe Aickelin & Jamie Twycross ASAP Group, School Of Computer Science, University Of Nottingham, UK. {jqg, uxa, jpt}@cs.nott.ac.uk INTRODUCTION is exposed to many different bacteria and food, neither of which are classically defined as `self', but In recent years computer systems have become neither of which produce an immune response. In increasingly complex and consequently the addition, the model of self-nonself discrimination challenge of protecting these systems has become cannot explain the phenomena of auto-immune increasingly difficult. Various techniques have diseases. In the example of multiple sclerosis, the been implemented to counteract the misuse of HIS attacks certain cells that it classifies as `self’. computer systems in the form of firewalls, anti- In 1994, Polly Matzinger [4] postulated that in this virus software and intrusion detection systems. instance, the HIS was not reacting to self or nonself The complexity of networks and dynamic nature but was due to a protection mechanism of sensing of computer systems leaves current methods with danger. The manner in which danger is detected significant room for improvement. forms the basis of the Danger Theory. Computer scientists have recently drawn The Danger Theory does not deny the existence of inspiration from mechanisms found in biological self-nonself discrimination but rather states there systems and, in the context of computer security, are other contributory factors involved in the have focused on the human immune system (HIS). initiation of an immune response. -

A Case of Mistaken Identity: Hsps Are No Damps but Dampers
Cell Stress and Chaperones (2012) 17:281–292 DOI 10.1007/s12192-011-0311-5 PERSPECTIVE AND REFLECTION ARTICLE A case of mistaken identity: HSPs are no DAMPs but DAMPERs Willem van Eden & Rachel Spiering & Femke Broere & Ruurd van der Zee Received: 9 November 2011 /Accepted: 15 November 2011 /Published online: 3 December 2011 # The Author(s) 2011. This article is published with open access at Springerlink.com Abstract Until recently, the immune system was seen What are DAMPs? solely as a defense system with its primary task being the elimination of unwanted microbial invaders. Currently, In the 1990s, Polly Matzinger introduced the concept of however, the functional significance of the immune system immunological “danger” as a further refinement of has obtained a much wider perspective, to include among Burnet’s original clonal selection theory which is the others the maintenance and restoration of homeostasis basis of self–nonself discrimination by the immune following tissue damage. In this latter aspect, there is a system (Fuchs and Matzinger 1996). In her “danger” growing interest in the identification of molecules involved, concept of immune function, she proposed immune such as the so-called danger or damage-associated molec- responses result from detecting and addressing danger ular patterns (DAMPs), also called alarmins. Since heat and not just nonself. In this context, the molecules shock proteins are archetypical molecules produced under associated with distress and damage (including self stressful conditions, such as tissue damage or inflammation, molecules) are regarded as the prime stimuli for immuno- they are frequently mentioned as prime examples of logical reactivity.