Programmed Necrosis and Disease:We Interrupt Your Regular Programming to Bring You Necroinflammation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Wound Classification
Wound Classification Presented by Dr. Karen Zulkowski, D.N.S., RN Montana State University Welcome! Thank you for joining this webinar about how to assess and measure a wound. 2 A Little About Myself… • Associate professor at Montana State University • Executive editor of the Journal of the World Council of Enterstomal Therapists (JWCET) and WCET International Ostomy Guidelines (2014) • Editorial board member of Ostomy Wound Management and Advances in Skin and Wound Care • Legal consultant • Former NPUAP board member 3 Today We Will Talk About • How to assess a wound • How to measure a wound Please make a note of your questions. Your Quality Improvement (QI) Specialists will follow up with you after this webinar to address them. 4 Assessing and Measuring Wounds • You completed a skin assessment and found a wound. • Now you need to determine what type of wound you found. • If it is a pressure ulcer, you need to determine the stage. 5 Assessing and Measuring Wounds This is important because— • Each type of wound has a different etiology. • Treatment may be very different. However— • Not all wounds are clear cut. • The cause may be multifactoral. 6 Types of Wounds • Vascular (arterial, venous, and mixed) • Neuropathic (diabetic) • Moisture-associated dermatitis • Skin tear • Pressure ulcer 7 Mixed Etiologies Many wounds have mixed etiologies. • There may be both venous and arterial insufficiency. • There may be diabetes and pressure characteristics. 8 Moisture-Associated Skin Damage • Also called perineal dermatitis, diaper rash, incontinence-associated dermatitis (often confused with pressure ulcers) • An inflammation of the skin in the perineal area, on and between the buttocks, into the skin folds, and down the inner thighs • Scaling of the skin with papule and vesicle formation: – These may open, with “weeping” of the skin, which exacerbates skin damage. -

Myeloid and Tubular Epithelial Cells Shape Renal Innate Immunity
Am J Physiol Renal Physiol 304: F1243–F1251, 2013. First published March 20, 2013; doi:10.1152/ajprenal.00101.2013. Review Sisters in arms: myeloid and tubular epithelial cells shape renal innate immunity Takashi Hato, Tarek M. El-Achkar, and Pierre C. Dagher Department of Medicine, Indiana University, Indianapolis, Indiana Submitted 19 February 2013; accepted in final form 13 March 2013 Hato T, El-Achkar TM, Dagher PC. Sisters in arms: myeloid and tubular epithelial cells shape renal innate immunity. Am J Physiol Renal Physiol 304: F1243– F1251, 2013. First published March 20, 2013; doi:10.1152/ajprenal.00101.2013.—The importance of innate immunity for survival is underscored by its presence at almost every level of the evolutionary tree of life. The task of “danger” recognition by the Downloaded from innate immune system is carried out by a broad class of pattern recognition receptors. These receptors are expressed in both hematopoietic and nonhematopoi- etic cells such as renal epithelial cells. Upon activation, pattern recognition receptors induce essentially two types of defensive responses: inflammation and phagocytosis. In this review, we highlight evidence that renal epithelial cells are endowed with such defensive capabilities and as such fully participate in renal innate immune responses. http://ajprenal.physiology.org/ epithelial cells; innate immunity; pattern recognition receptors; Toll-like receptor; endotoxin THE FUNDAMENTAL ROLE OF THE innate immune system is to primarily focus on the less explored “innate immune cells”, initiate a quick response immediately after detecting “danger i.e., renal epithelial cells. signals” in the setting of infection (nonself) or tissue injury (self). -

797 Circulating Tumor DNA and Circulating Tumor Cells for Cancer
Medical Policy Circulating Tumor DNA and Circulating Tumor Cells for Cancer Management (Liquid Biopsy) Table of Contents • Policy: Commercial • Coding Information • Information Pertaining to All Policies • Policy: Medicare • Description • References • Authorization Information • Policy History • Endnotes Policy Number: 797 BCBSA Reference Number: 2.04.141 Related Policies Biomarkers for the Diagnosis and Cancer Risk Assessment of Prostate Cancer, #336 Policy1 Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity Plasma-based comprehensive somatic genomic profiling testing (CGP) using Guardant360® for patients with Stage IIIB/IV non-small cell lung cancer (NSCLC) is considered MEDICALLY NECESSARY when the following criteria have been met: Diagnosis: • When tissue-based CGP is infeasible (i.e., quantity not sufficient for tissue-based CGP or invasive biopsy is medically contraindicated), AND • When prior results for ALL of the following tests are not available: o EGFR single nucleotide variants (SNVs) and insertions and deletions (indels) o ALK and ROS1 rearrangements o PDL1 expression. Progression: • Patients progressing on or after chemotherapy or immunotherapy who have never been tested for EGFR SNVs and indels, and ALK and ROS1 rearrangements, and for whom tissue-based CGP is infeasible (i.e., quantity not sufficient for tissue-based CGP), OR • For patients progressing on EGFR tyrosine kinase inhibitors (TKIs). If no genetic alteration is detected by Guardant360®, or if circulating tumor DNA (ctDNA) is insufficient/not detected, tissue-based genotyping should be considered. Other plasma-based CGP tests are considered INVESTIGATIONAL. CGP and the use of circulating tumor DNA is considered INVESTIGATIONAL for all other indications. 1 The use of circulating tumor cells is considered INVESTIGATIONAL for all indications. -

Theory Revolution? Doubts About The
Cutting Edge Commentary: A Copernican Revolution? Doubts About the Danger Theory This information is current as Russell E. Vance of September 29, 2021. J Immunol 2000; 165:1725-1728; ; doi: 10.4049/jimmunol.165.4.1725 http://www.jimmunol.org/content/165/4/1725 Downloaded from References This article cites 42 articles, 11 of which you can access for free at: http://www.jimmunol.org/content/165/4/1725.full#ref-list-1 Why The JI? Submit online. http://www.jimmunol.org/ • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average by guest on September 29, 2021 Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2000 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. ● Cutting Edge Commentary: A Copernican Revolution? Doubts About the Danger Theory1 Russell E. Vance2 What Is the Danger Theory? The immune system is often said to function by “self-nonself” Although the notion that the immune system has evolved to rec- discrimination. Recently, some have argued that it actually de- ognize (dangerous) pathogens is not new (15), recent discussions tects “danger” or “strangers.” There are problems with all of of “danger” have revolved around one particular characterization these points of view. -

A 10 Year Cross Sectional Multicentre Study of Infected Pancreatic Necrosis
JOP. J Pancreas (Online) 2021 Jan 30; 22(1): 11-20. ORIGINAL PAPER A 10 Year Cross Sectional Multicentre Study of Infected Pancreatic Necrosis. Trends in Management and an Analysis of Factors Predicting Mortality for Interventions in Infected Pancreatic Necrosis Johann Faizal Khan1, Suryati Mokhtar1, Krishnan Raman1, Harjit Singh1, Leow Voon Meng 2,3, Manisekar K Subramaniam1,2 1 2 Department of Hepatopancreatobiliary Surgery and Liver Transplantation, Selayang Hospital, Selangor, Malaysia 3Department of General Surgery, Division of Hepatopancreatobiliary Surgery, Sultanah Bahiyah Hospital, Kedah, Malaysia Malaysia Advanced Medical and Dental Institute (AMDI), Science University of Malaysia (USM), Penang, ABSTRACT Objective To identify trends in management and analyse outcomes of patients undergoing interventions for infected pancreatic necrosis Method A cross sectional study of patients undergoing intervention for IPN with specific reference to factors predictive of mortality. between 2009-2018 were performed at two of the largest hepatopancreatobiliary centres in Malaysia. FinalResults outcome A measuretotal number of complete of 65 resolution was compared against mortality (D). Head to head comparison of percutaneous catheter drainage alone versus Videoscopic Assisted Retroperitoneal Debridement was performed based on final predictive factor on mortality. patients with IPN were identified. Data from 59/65 patients were analysed for final outcome of death (D) versus complete resolution. 6 patients were omitted due to incomplete data -

Cognitive and Memory Functions in Plant Immunity
Review Cognitive and Memory Functions in Plant Immunity Hidetaka Yakura Institute for Science and Human Existence, Tokyo 163-8001, Japan; [email protected] Received: 5 August 2020; Accepted: 16 September 2020; Published: 17 September 2020 Abstract: From the time of Thucydides in the 5th century BC, it has been known that specific recognition of pathogens and memory formation are critical components of immune functions. In contrast to the immune system of jawed vertebrates, such as humans and mice, plants lack a circulatory system with mobile immune cells and a repertoire of clonally distributed antigen receptors with almost unlimited specificities. However, without these systems and mechanisms, plants can live and survive in the same hostile environment faced by other organisms. In fact, they achieve specific pathogen recognition and elimination, with limited self-reactivity, and generate immunological memory, sometimes with transgenerational characteristics. Thus, the plant immune system satisfies minimal conditions for constituting an immune system, namely, the recognition of signals in the milieu, integration of that information, subsequent efficient reaction based on the integrated information, and memorization of the experience. In the previous report, this set of elements was proposed as an example of minimal cognitive functions. In this essay, I will first review current understanding of plant immunity and then discuss the unique features of cognitive activities, including recognition of signals from external as well as internal environments, autoimmunity, and memory formation. In doing so, I hope to reach a deeper understanding of the significance of immunity omnipresent in the realm of living organisms. Keywords: autoimmunity; cognition; metaphysicalization; plant immunity; transgenerational memory 1. -

Systemic Features of Immune Recognition
PhD degree in Foundations of the Life Sciences and their Ethical Consequences European School of Molecular Medicine (SEMM) and University of Milan Faculty of Medicine Settore disciplinare: FIL/2 SYSTEMIC FEATURES OF IMMUNE RECOGNITION Bartlomiej Swiatczak IFOM-IEO Campus, Milan Matricola n. R07404 Supervisor: Prof. Mark Bedau Visiting Professor IFOM-IEO Campus, Milan Anno accademico 2010-2011 1 Acknowledgements I would like to express my sincere gratitude to my supervisor Professor Mark Bedau for his invaluable encouragement and guidance. I could not have imagined having a better advisor and a mentor for my PhD. Without his constant support and patience I would never have finished this work. I owe many thanks to my second supervisor, Professor Irun Cohen for being a constant source of inspiration and for many useful discussions. I am also grateful to my laboratory supervisor, Doctor Maria Rescigno for support and useful criticisms during my PhD. I would also like to thank Professor John Dupré and Doctor Stefano Casola for their very constructive input in developing this thesis. I also extend my gratitude to the coordinators of the FOLSATEC program, Professor Giovanni Boniolo and Doctor Giuseppe Testa for their continuous encouragement throughout these years. 2 Table of contents List of Abbreviations……………………………………………………………………. 6 Figure index……………………………………………………………………………... 9 Author’s declaration…………………………………………………………………….. 10 Abstract………………………………………………………………………………….. 11 Introduction……………………………………………………………………………… 12 Part 1. Immune recognition as an integrated activity of cells and molecules….…. 16 Single types of cells and molecules cannot distinguish between pathogenic 17 and non-pathogenic microbes………………………………………………… Single types of cells and molecules, in principle, cannot recognize pathogens………………………………..…………………………...……….. 24 Return to basics: What makes a pathogen a pathogen?.................................... -

WA Coding Rule 1215/07 Skin Ulcer Necrosis Versus Gangrene
WA Coding Rules are a requirement of the Clinical Coding Policy MP0056/17 Western Australian Coding Rule 1215/07 Skin ulcer necrosis versus gangrene WA Coding Rule 0110/06 Skin ulcer necrosis versus gangrene is superseded by ACCD Coding Rule Skin necrosis (Ref No: Q2659) effective 1 January 2014; (log in to view on the ACCD CLIP portal). DECISION WA Coding Rule 0110/06 Skin ulcer necrosis versus gangrene is retired. [Effective 01 Jan 2014, ICD-10-AM/ACHI/ACS 8th Ed.] Page 1 of 3 © Department of Health WA 2018 WA Coding Rules are a requirement of the Clinical Coding Policy MP0056/17 Western Australian Coding Rule 0110/06 Skin ulcer necrosis versus gangrene Q. Often with traumatic wounds or infection there will be documentation of devitalized tissue or necrotic wound edges or just some mention of necrotic tissue, the extent of the necrosis usually not known. No mention of gangrene. The ICD 10 indexing for necrosis defaults to coding R02. For cases with documentation of necrosis irrespective of the extent of necrosis and definitely no mention of gangrene is the coder to assign the code R02 or if documentation suggests the amount of necrosis is small and confined to edges should this be considered part of the traumatic wound and the code not assigned? Necrosis is commonly documented in the patient records with traumatic wounds, burns, pressure sores etc. Necrosis due to lack of oxygen such as with a MI would be considered part of the MI code as would any necrosis with infection in pneumonia. Gangrene would seem to be a complication of necrotic tissue. -

Molecular Pathological Epidemiology in Diabetes Mellitus and Risk of Hepatocellular Carcinoma
Submit a Manuscript: http://www.wjgnet.com/esps/ World J Hepatol 2016 September 28; 8(27): 1119-1127 Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx ISSN 1948-5182 (online) DOI: 10.4254/wjh.v8.i27.1119 © 2016 Baishideng Publishing Group Inc. All rights reserved. REVIEW Molecular pathological epidemiology in diabetes mellitus and risk of hepatocellular carcinoma Chun Gao Chun Gao, Department of Gastroenterology, China-Japan logy and epidemiology, and investigates the relationship Friendship Hospital, Ministry of Health, Beijing 100029, China between exogenous and endogenous exposure factors, tumor molecular signatures, and tumor initiation, progres- Author contributions: Gao C conceived the topic, performed sion, and response to treatment. Molecular epidemiology research, retrieved concerned literatures and wrote the paper. broadly encompasses MPE and conventional-type mole- cular epidemiology. Hepatocellular carcinoma (HCC) Supported by Beijing NOVA Programme of Beijing Municipal is the third most common cause of cancer-associated Science and Technology Commission, No. Z13110.7000413067. death worldwide and remains as a major public health Conflict-of-interest statement: No conflict of interest. challenge. Over the past few decades, a number of epidemiological studies have demonstrated that diabetes Open-Access: This article is an open-access article which was mellitus (DM) is an established independent risk factor selected by an in-house editor and fully peer-reviewed by external for HCC. However, how DM affects the occurrence and -

Salivary Gland – Necrosis
Salivary Gland – Necrosis Figure Legend: Figure 1 Salivary gland - Necrosis in a male F344/N rat from a subchronic study. There is necrosis of the acinar cells (arrow) with inflammation. Figure 2 Salivary gland - Necrosis in a male F344/N rat from a subchronic study. There is necrosis of the acinar cells (arrow) with chronic active inflammation. Figure 3 Salivary gland - Necrosis in a female F344/N rat from a subchronic study. There is necrosis of an entire lobe of the salivary gland (arrow), consistent with an infarct. Figure 4 Salivary gland - Necrosis in a female F344/N rat from a subchronic study. There is necrosis of all the components of the salivary gland (consistent with an infarct), with inflammatory cells, mostly neutrophils. Comment: Necrosis may be characterized either by scattered single-cell necrosis or by locally extensive areas of necrosis involving contiguous cells or structures. Single-cell necrosis can present as cell shrinkage, condensation of nuclear chromatin and cytoplasm, convolution of the cell, and the presence of apoptotic bodies. Acinar necrosis can present as focal to multifocal areas characterized by 1 Salivary Gland – Necrosis tissue that is paler than the surrounding viable tissue, consisting of swollen cells with variable degrees of eosinophilia, hyalinized cytoplasm, vacuolated cytoplasm, nuclear pyknosis, karyolysis, and/or karyorrhexis with associated cellular debris (Figure 1 and Figure 2). Secondary inflammation is common. Infarction (Figure 3 and Figure 4) is characterized by a focal to focally extensive area of salivary gland necrosis. One cause of necrosis, inflammation, and atrophy of the salivary gland in the rat is an active sialodacryoadenitis virus infection, but this virus does not affect the mouse salivary gland. -
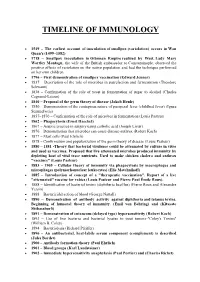
Timeline of Immunology
TIMELINE OF IMMUNOLOGY 1549 – The earliest account of inoculation of smallpox (variolation) occurs in Wan Quan's (1499–1582) 1718 – Smallpox inoculation in Ottoman Empire realized by West. Lady Mary Wortley Montagu, the wife of the British ambassador to Constantinople, observed the positive effects of variolation on the native population and had the technique performed on her own children. 1796 – First demonstration of smallpox vaccination (Edward Jenner) 1837 – Description of the role of microbes in putrefaction and fermentation (Theodore Schwann) 1838 – Confirmation of the role of yeast in fermentation of sugar to alcohol (Charles Cagniard-Latour) 1840 – Proposal of the germ theory of disease (Jakob Henle) 1850 – Demonstration of the contagious nature of puerperal fever (childbed fever) (Ignaz Semmelweis) 1857–1870 – Confirmation of the role of microbes in fermentation (Louis Pasteur) 1862 – Phagocytosis (Ernst Haeckel) 1867 – Aseptic practice in surgery using carbolic acid (Joseph Lister) 1876 – Demonstration that microbes can cause disease-anthrax (Robert Koch) 1877 – Mast cells (Paul Ehrlich) 1878 – Confirmation and popularization of the germ theory of disease (Louis Pasteur) 1880 – 1881 -Theory that bacterial virulence could be attenuated by culture in vitro and used as vaccines. Proposed that live attenuated microbes produced immunity by depleting host of vital trace nutrients. Used to make chicken cholera and anthrax "vaccines" (Louis Pasteur) 1883 – 1905 – Cellular theory of immunity via phagocytosis by macrophages and microphages (polymorhonuclear leukocytes) (Elie Metchnikoff) 1885 – Introduction of concept of a "therapeutic vaccination". Report of a live "attenuated" vaccine for rabies (Louis Pasteur and Pierre Paul Émile Roux). 1888 – Identification of bacterial toxins (diphtheria bacillus) (Pierre Roux and Alexandre Yersin) 1888 – Bactericidal action of blood (George Nuttall) 1890 – Demonstration of antibody activity against diphtheria and tetanus toxins. -

Chapter 15 Self and Nonself Moira Howes
Chapter 15 Self and Nonself moira howes 1. Introduction Immunology is the science that investigates how organisms defend themselves against infection, harmful substances, and foreign tissue. In order for an organism to defend itself against such threats, however, its immune system presumably must be able to discriminate self from nonself. If the immune system could not make such a discrimina- tion, it might harm the organism it is to defend, rather than the microbes infecting it. Self–nonself discrimination thus appears to be a crucial function of the immune system. Indeed, immunology has been referred to as the “science of self–nonself discrimination” (Klein, 1982). How self–nonself discrimination is achieved depends, among other things, on whether an organism is an invertebrate or a jawed vertebrate. Self–nonself discrimina- tion is more rudimentary in invertebrates (and jawless fi shes) because their immune systems are “innate.” Innate immune mechanisms are those that do not change after repeated exposure to a given infectious agent; they do not learn. This contrasts with a type of immunity in jawed vertebrates – adaptive immunity – which does change after repeated exposure to pathogens. After the adaptive immune system adapts to a given pathogen, it can target the pathogen with greater precision and eliminate it more rapidly. Because of adaptive immunity, self–nonself discrimination in jawed vertebrates is specialized and precise: vertebrate immune systems are fi ne-tuned to differences between self and nonself. So signifi cant do immunologists fi nd the evolution of adaptive immunity – both with respect to enhanced pathogen defense and self–nonself discrimination – that some refer to it as the “immunological Big Bang” (Janeway & Travers, 2005).