Radiation Hazard, Safety, Control and Protection Review Article
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of Fernald
Draft ADVISORY BOARD ON RADIATION AND WORKER HEALTH National Institute for Occupational Safety and Health Review of the General Steel Industries Special Exposure Cohort (SEC) Petition-00105 and the NIOSH SEC Petition Evaluation Report Contract No. 200-2009-28555 SCA-SEC-TASK5-0005 Prepared by S. Cohen & Associates 1608 Spring Hill Road, Suite 400 Vienna, Virginia 22182 July 2009 [Redacted version – October 2, 2009] Disclaimer This document is made available in accordance with the unanimous desire of the Advisory Board on Radiation and Worker Health (ABRWH) to maintain all possible openness in its deliberations. However, the ABRWH and its contractor, SC&A, caution the reader that at the time of its release, this report is pre-decisional and has not been reviewed by the Board for factual accuracy or applicability within the requirements of 42 CFR 82. This implies that once reviewed by the ABRWH, the Board’s position may differ from the report’s conclusions. Thus, the reader should be cautioned that this report is for information only and that premature interpretations regarding its conclusions are unwarranted. Effective Date: Revision No.: Document No.: Page No.: July 24, 2009 0 SCA-SEC-TASK5-0005 Page 2 of 50 S. COHEN & ASSOCIATES: Document No. SCA-SEC-TASK5-0005 Technical Support for the Advisory Board on Effective Date: Radiation & Worker Health Review of July 24, 2009 – Draft NIOSH Dose Reconstruction Program Redacted version – October 2, 2009 Revision No. 0 Review of the General Steel Industries Special Exposure Cohort (SEC) Petition-00105 -
A Standard Complex-Wide Methodology for Overestimating External Doses Effective Date: 06/05/2006 Measured with Film Badge Dosimeters Type of Document: OTIB
ORAU TEAM Dose Reconstruction Project for NIOSH Oak Ridge Associated Universities I Dade Moeller & Associates I MJW Corporation Page 1 of 19 Document Title: Document Number: ORAUT-OTIB-0010 Revision: 01 A Standard Complex-Wide Methodology for Overestimating External Doses Effective Date: 06/05/2006 Measured with Film Badge Dosimeters Type of Document: OTIB Supersedes: Revision 00 Subject Experts: Donald N. Stewart and Jack J. Fix Document Owner Approval: Signature on File Approval Date: 05/17/2006 James P. Griffin, Deputy Project Director Concurrence: Signature on File Concurrence Date: 05/22/2006 Kate Kimpan, Project Director Approval: Signature on File Approval Date: 06/05/2006 James W. Neton, Associate Director for Science New Total Rewrite Revision Page Change FOR DOCUMENTS MARKED AS A TOTAL REWRITE, REVISION, OR PAGE CHANGE, REPLACE THE PRIOR REVISION AND DISCARD / DESTROY ALL COPIES OF THE PRIOR REVISION. Document No. ORAUT-OTIB-0010 Revision No. 01 Effective Date: 06/05/2006 Page 2 of 19 PUBLICATION RECORD EFFECTIVE REVISION DATE NUMBER DESCRIPTION 01/12/2004 00 New Technical Information Bulletin for a Standard Complex-Wide Correction Factor for Overestimating External Doses Measured with Film Badge Dosimeters. First approved issue. Initiated by Donald N. Stewart. 06/05/2006 01 Constitutes rewrite of document as a result of biennial review. Incorporates resolution of S. Cohen & Associates final draft comments contained in “The Review of NIOSH/ORAUT Procedures and Methods used for Dose Reconstruction” (ref: letter from John Mauro to David Staudt, dated January 17, 2005). Approved issue of Revision 01. This revision results in no change to the assigned dose and no PER is required. -

ORAU Team Document Number: ORAUT-TKBS-0008-6
ORAU Team Document Number: ORAUT-TKBS-0008-6 Dose Reconstruction Project for NIOSH Effective Date: 09/21/2004 Revision No.: 00 Technical Basis Document for the Nevada Test Site – Controlled Copy No.: ________ Occupational External Dose Page 1 of 55 Subject Expert: Eugene M. Rollins Supersedes: Document Owner Approval: Signature on File Date: 09/16/2004 Eugene M. Rollins, TBD Team Leader None Approval: Signature on File Date: 09/16/2004 Judson L. Kenoyer, Task 3 Manager Concurrence: Signature on File Date: 09/13/2004 Richard E. Toohey, Project Director Approval: Signature on File Date: 09/21/2004 James W. Neton, Associate Director for Science TABLE OF CONTENTS Section Page Record of Issue/Revisions ................................................................................................................... 4 Acronyms and Abbreviations ............................................................................................................... 5 6.1 Introduction ................................................................................................................................. 7 6.2 Dosimetric Basis of Comparison ................................................................................................. 7 6.2.1 Photon Measurement Quantities ........................................................................................ 8 6.2.2 Beta Measurement Quantities ............................................................................................ 9 6.2.3 Neutron Measurement Quantities ...................................................................................... -

The Use of Film Badges for Personnel Monitoring
This publication is not longer valid Please see http://www-ns.iaea.org/standards/ SAFETY SERIES No. 8 The Use of Film Badges for Personnel Monitoring INTERNATIONAL ATOMIC ENERGY AGENCY, VIENNA, 1962 This publication is not longer valid Please see http://www-ns.iaea.org/standards/ This publication is not longer valid Please see http://www-ns.iaea.org/standards/ THE USE OF FILM BADGES FOR PERSONNEL MONITORING This publication is not longer valid Please see http://www-ns.iaea.org/standards/ The following States are Members of the International Atomic Energy Agency: AFGHANISTAN ISRAEL ALBANIA ITALY ARGENTINA JAPAN AUSTRALIA REPUBLIC OF KOREA AUSTRIA LEBANON BELGIUM LUXEMBOURG BRAZIL MALI BULGARIA MEXICO BURMA MONACO BYELORUSSIAN SOVIET MOROCCO SOCIALIST REPUBLIC NETHERLANDS CAMBODIA NEW ZEALAND CANADA NICARAGUA CEYLON NORWAY CHILE PAKISTAN CHINA PARAGUAY COLOMBIA PERU CONGO (LEOPOLDVILLE) PHILIPPINES CUBA POLAND CZECHOSLOVAK SOCIALIST PORTUGAL REPUBLIC ROMANIA DENMARK SENEGAL DOMINICAN REPUBLIC SOUTH AFRICA ECUADOR SPAIN EL SALVADOR SUDAN ETHIOPIA SWEDEN FINLAND SWITZERLAND FRANCE THAILAND FEDERAL REPUBLIC TUNISIA OF GERMANY TURKEY GHANA UKRAINIAN SOVIET GREECE SOCIALIST REPUBLIC GUATEMALA UNION OF SOVIET HAITI SOCIALIST REPUBLICS HOLY SEE UNITED ARAB REPUBLIC HONDURAS UNITED KINGDOM OF GREAT HUNGARY BRITAIN AND NORTHERN ICELAND IRELAND INDIA UNITED STATES OF AMERICA INDONESIA VENEZUELA IRAN VIET-NAM IRAQ YUGOSLAVIA The Agency’s Statute was approved on 26 October 1956 at an international conference held at United Nations headquarters, New York, and the Agency came into being when the Statute entered into force on 29 July 1957. The first session of the General Conference was held in Vienna, Austria, the permanent seat of the Agency, in October, 1957. -
Individual Monitoring Individual Monitoring Practical Radiation Technical Manual
PRACTICAL RADIATION TECHNICAL MANUAL INDIVIDUAL MONITORING INDIVIDUAL MONITORING PRACTICAL RADIATION TECHNICAL MANUAL INDIVIDIAL MONITORING INTERNATIONAL ATOMIC ENERGY AGENCY VIENNA, 2004 INDIVIDUAL MONITORING IAEA, VIENNA, 2004 IAEA-PRTM-2 (Rev. 1) © IAEA, 2004 Permission to reproduce or translate the information in this publication may be obtained by writing to the International Atomic Energy Agency, Wagramer Strasse 5, P.O. Box 100, A-1400 Vienna, Austria. Printed by the IAEA in Vienna April 2004 FOREWORD Occupational exposure to ionizing radiation can occur in a range of industries, such as mining and milling; medical institutions; educational and research establishments; and nuclear fuel facilities. Adequate radiation protection of workers is essential for the safe and acceptable use of radiation, radioactive materials and nuclear energy. Guidance on meeting the requirements for occupational protection in accordance with the Basic Safety Standards for Protection against Ionizing Radiation and for the Safety of Radiation Sources (IAEA Safety Series No. 115) is provided in three interrelated Safety Guides (IAEA Safety Standards Series Nos. RS-G-1.1, 1.2 and 1.3) covering the general aspects of occupational radiation protection as well as the assessment of occupational exposure. These Safety Guides are in turn supplemented by Safety Reports providing practical information and technical details for a wide range of purposes, from methods for assessing intakes of radionuclides to optimization of radiation protection in the control of occupational exposure. Occupationally exposed workers need to have a basic awareness and understanding of the risks posed by exposure to radiation and the measures for managing these risks. To address this need, two series of publications, the Practical Radiation Safety Manuals (PRSMs) and the Practical Radiation Technical Manuals (PRTMs) were initiated in the 1990s. -

Photographic Dosimetry of X- and Gamma Rays 15 U
* Keterence dook PHOTOGRAPHIC DOSIMETRY OF X- AND GAMMA RAYS Handbook 57 U. S. Department of Commerce National Bureau of Standards HANDBOOKS OF THE NATIONAL BUREAU OF STANDARDS The following Handbooks issued by the Bureau are avail¬ able by purchase from the Superintendent of Documents, Government Printing Office, Washington 25, D. C., at the prices indicated: No. Price 23 Radium Protection_ $0. 20 27 Safe Handling of Radioactive Luminous Compounds_ . 10 28 (1944) Screw Thread Standards for Federal Services_ 1. 25 1950 Supplement_ . 60 30 National Electrical Safety Code_ 1. 75 31 Safety Rules for the Installation and Maintenance of Elec¬ trical Supply Stations_ . 10 34 Safety Rules for the Operation of Electric Equipment and Lines__ . 25 35 Safety Rules for Radio Installations_ . 15 36 Safety Rules for Electric Fences_ . 15 37 Testing of Weighing Equipment_ 1. 25 39 Discussion of the National Electrical Safety Code_ 1. 25 41 Medical X-ray Protection Up to Two Million Volts_ . 25 42 Safe Handling of Radioactive Isotopes_ . 20 43 Installation and Maintenance of Electric Supply and Com¬ munication Lines. Safety Rules and Discussion_ 2. 00 44 Specifications, Tolerances, and Regulations for Commercial Weighing and Measuring Devices_ 1. 25 45 Testing of Measuring Equipment_ 1. 50 46 Code for Protection Against Lightning_ . 40 47 Recommendations of the International Commission on Radiological Protection and of the International Com¬ mission on Radiological Units 1950_ 20 48 Control and Removal of Radioactive Contamination in Laboratories_ 15 49 Recommendations for Waste Disposal of Phosphorus-32 and Iodine-131 for Medical Users_ 15 50 X-ray Protection Design_ 20 51 Radiological Monitoring Methods and Instruments_ 15 52 Maximum Permissible Amounts of Radioisotopes in the Human Body and Maximum Permissible Concentrations in Air and Water_ 20 53 Recommendations for the Disposal of Carbon-14 Wastes. -

Historical Evaluation of the Film Badge Dosimetry Program at the Y-12 Plant in Oak Ridge, Tennessee, Part 3 – Beta Radiation, ORAUT-OTIB-0046, Rev
ORAU TEAM Dose Reconstruction Project for NIOSH Oak Ridge Associated Universities I Dade Moeller I MJW Technical Services Page 1 of 56 DOE Review Release 12/14/2009 Document Title: Document Number: ORAUT-OTIB-0045 Revision: 01 Historical Evaluation of the Film Badge Effective Date: 11/30/2009 Dosimetry Program at the Y-12 Plant in Oak Ridge, Tennessee: Part 2 – Neutron Radiation Type of Document: OTIB Supersedes: Revision 00 (ORAUT-RPRT-0033) Subject Expert(s): George D. Kerr, Edward L. Frome, Janice P. Watkins, William G. Tankersley Site Expert(s): N/A Approval: Signature on File Approval Date: 11/12/2009 George D. Kerr, Document Owner Concurrence: Signature on File Concurrence Date: 11/12/2009 John M. Byrne, Objective 1 Manager Concurrence: Keith A. McCartney Signature on File for Concurrence Date: 11/23/2009 Edward F. Maher, Objective 3 Manager Concurrence: Signature on File Concurrence Date: 11/12/2009 Kate Kimpan, Project Director Approval: Signature on File Approval Date: 11/30/2009 James W. Neton, Associate Director for Science New Total Rewrite Revision Page Change FOR DOCUMENTS MARKED AS A TOTAL REWRITE, REVISION, OR PAGE CHANGE, REPLACE THE PRIOR REVISION AND DISCARD / DESTROY ALL COPIES OF THE P RIOR REVIS ION. Document No. ORAUT-OTIB-0045 Revision No. 01 Effective Date: 11/30/2009 Page 2 of 56 PUBLICATION RECORD EFFECTIVE REVISION DATE NUMBER DESCRIPTION 04/13/2005 00 This report was previously published as an Oak Ridge Associated Universities document and is now being incorporated as an ORAU Team controlled document. Future revisions will be reviewed and approved by NIOSH. -
Neutron Scattering at ORNL to the Point Focus on Biofuels US ITER Gets New Director, ORNL 24
Contents Editorial Infographic . 1 Neutron scattering for a better world 22 Neutron scattering at ORNL To the Point Focus on Biofuels US ITER gets new director, ORNL 24 . Getting to the root of better plants . fuel tech can make ethanol 2 competitive, ORNL home to nine Focus on Transportation highly cited researchers . ORNL engine research supports 26 new fuel development Neutrons 8 . Neutrons open a world of research Focus on Physical Sciences . What makes neutron scattering . Bio-inspired material soaks up 10 unique 28 oceans’ uranium . SNS upgrades will benefit . Right electrolyte doubles 2D 12 researchers 30 material’s ability to store energy Focus on Computing Early Career Award Winners Farewell, Titan: A long-running The future is bright: Nine ORNL 18 . supercomputer with tremendous 32 . researchers take home prestigious impact early career awards . Igniting a new class of combustion Why Science? 20 research . Young researchers explain 42 Time Warp . The church that’s not supposed to 44 be there On the Cover Neutron scattering scientist Hugh O'Neill leads ORNL's Center for Structural Molecular Biology. Image credit: Genevieve Martin, ORNL Neutron scattering for a better world eutron science began at Oak Ridge in 1944 when researcher Ernest Wollan took advantage of the world's first N continuously operating nuclear reactor—the X-10 Graphite Reactor—to study the diffraction of neutrons in a single crystal. In the intervening years, neutron scattering has proved to be an indispensable tool for scientific research, with neutron research at ORNL leading the way to such advances as better batteries, more effective drugs, and stronger armor for the military. -

Evaluation of Annual External Radiation Doses at Values Near Minimum Detection Levels of Dosimeters at the Hanford Nuclear Facility
Journal of Exposure Analysis and Environmental Epidemiology (2000) 10, 27±35 # 2000 Nature America, Inc. All rights reserved 1053-4245/00/$15.00 www.nature.com/jea Evaluation of annual external radiation doses at values near minimum detection levels of dosimeters at the Hanford nuclear facility DAVID RICHARDSON,a STEVE WING,a JAMES WATSONb AND SUSANNE WOLFa aDepartment of Epidemiology, School of Public Health, University of North Carolina, Chapel Hill, North Carolina 27599 bDepartment of Environmental Science and Engineering, School of Public Health, University of North Carolina, Chapel Hill, North Carolina 27599 In epidemiological studies of workers exposed to ionizing radiation, recognition of the limitations of available radiation dosimetry data is important to interpretation of a study's findings. This paper provides an investigation of external radiation dosimetry data for workers at the Hanford nuclear facility, focusing on changes over time in practices for recording dosimetry measurements that were between zero and the minimum detectable level of a radiation dosimeter. Reported annual external radiation doses for the years 1944±1989 were examined for 33,459 workers; these records are the sum of periodic dosimetry measurements within a calendar year. For each year, the proportion of annual external doses with values in the range of minimum detectable level was examined. Contrary to previous researchers, we conclude that there is evidence that dosimetry measurements with values between zero and the minimum detectable level may have been recorded as zero in some historical periods. This conclusion is supported by evidence drawn from historical documentation about radiation dosimetry practices at the Hanford facility. Although workers at the Hanford facility have relatively complete and detailed external radiation dosimetry data compared to some other nuclear facilities that began operation in the 1940s, these data may suffer limitations related to dosimetry recording practices at the facility. -
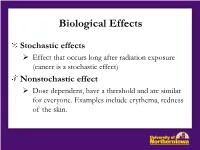
Biological Effects and Methods For
Biological Effects Stochastic effects Effect that occurs long after radiation exposure (cancer is a stochastic effect) Nonstochastic effect Dose dependent, have a threshold and are similar for everyone. Examples include erythema, redness of the skin. Biological Effects Somatic Effects Physical effects May be immediate or delayed Genetic Effects Birth defects due to irradiation to reproductive cells before conception Teratogenic Effects Cancer or congenital malformation due to radiation exposure to fetus in utero Biological Effects Dose terms Absorbed dose Energy imparted by ionizing radiation per unit mass of irradiated material. Rad or Gray Dose equivalent Product of absorbed dose and quality factor (QF, radiation weighting factor) which compensates for ‘effectiveness” of different types of radiation in producing biological damage. SI unit is Sievert (SV). More common units are Rem or Roentgen effective man. Smaller dose = mrem. Committed dose Dose equivalent to given organs or tissues of reference received from intake of radioactive material over 50 year period following intake. Biological Effects Weighting Factors (Q, RBE) _________________________________________________________ LET in water Weighting factor Type and energy of radiation (eV/nm) wr __________________________________________________________________________ 0.2 – 35 1 photons (X-rays and γ’s) – 1. 0.2 – 1.1 1 all electrons > 5 keV 20 5 slow neutrons < 10 keV 50 20 intermediate n’s 0.1 – 2 MeV 10 fast n’s 2 -20 MeV 5 protons > 2 MeV 20 α particles – 5 MeV, high energy ions Effects of Acute, Whole-Body Gamma Radiation Absorbed Dose Probability of Survival 100 rad Virtually certain 100 – 200 rad Probable 200 – 450 rad Probable 500 – 600 rad Almost impossible 900 – 1200 rad Possible in some cases with bone marrow transplant Note: As a comparison, the estimated average annual whole body dose from all sources to the population is about 0.2 rad per year. -

Multiple Choice Questions
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) Heart Multiple choice questions 1. When the distance from the source of radiation is doubled, the amount of radiation received by the operator will be? a. Tripled b. Doubled c. The same d. Reduced by ½ e. Reduced by 3/4 Increasing the distance between the operator and the radiation source, will reduce exposure by the square of the distance from the source. Doubling the distance between the operator and the radiation source will reduc radiation exposure by a factor of 4. 2. During X-ray diagnostics, a staff member wears personal protective clothing – which of the following offers the best protection? a. an apron with a thickness of 0.25 lead-equivalent without a thyroid collar b. an apron with a thickness of 0.25 lead-equivalent and a thyroid collar c. an apron with a thickness of 0.35 lead-equivalent without a thyroid collar d. an apron with a thickness of 0.35 lead-equivalent and a thyroid collar e. an apron with a thickness of 0.15 lead-equivalent and a thyroid collar Lead aprons are the primary radiation protective garments used by staff during exposure to X rays. The radiation protection provided by a lead apron is approximately the same as 0.25- to 1-mm thick lead. Thicker aprons are usually more protective but heavier. An apron with 0.5-mm thickness can attenuate approximately 90% or more of the scatter radiation. -

Radiation Safety Manual
Radiation Safety Manual BU Baylor University [Pick the date] BAYLOR UNIVERSITY Radiation Safety Manual PURPOSE: Radioactive materials and radiation machines are used by Baylor University faculty, staff, and students. These materials are highly regulated by local, state, and federal entities. This manual ensures the compliant and safe use of all such materials and machines as required by law. SCOPE: This manual defines the acceptable use and possession of all radioactive materials or radiation machines emitting ionizing radiation by all Baylor University faculty, staff, and students. RESPONSIBILITY: It is the responsibility of each individual department at Baylor University to ensure that its students, faculty and staff use materials and machines which emit ionizing radiation in a legal, safe and compliant manner. The University Radiation Safety Officer (RSO) shall act as an advisory point of contact and the Department of Environmental Health & Safety (EHS) shall also offer advice and support where applicable. The Department of EHS and University RSO will manage the application of this manual. Formulated: 11/2005 Revised: 8/29/06; 2/20/07; 11/15/07; 4/12/11; 6/14/13; 3/8/2016; 4/26/2018; 8/8/2019; 2/25/2020; 3/16/2020 Last Reviewed: August 2021 Page 2 BAYLOR UNIVERSITY Radiation Safety Manual TABLE OF CONTENTS Introduction 8 Part I. Responsibility and Authority of the Baylor University Radiation Safety Officer 9 A. Establishment of Radiation Safety Policy 9 B. Licensing 9 C. Oversight of the Radiation Safety Program 10 D. Investigation of Incidents 10 Part II. The Radiation Safety Officer 10 A. Qualifications of the Radiation Safety Officer 10 B.