Uganda Country Strategy Paper Evaluation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Gomba District Hazard, Risk and Vulnerability Profi Le
Gomba District Hazard, Risk and Vulnerability Profi le 2016 GOMBA DISTRICT HAZARD, RISK AND VULNERABILITY PROFILE a Acknowledgment On behalf of Office of the Prime Minister, I wish to express my sincere appreciation to all of the key stakeholders who provided their valuable inputs and support to this Multi-Hazard, Risk and Vulnerability mapping exercise that led to the production of comprehensive district Hazard, Risk and Vulnerability (HRV) profiles. I extend my sincere thanks to the Department of Relief, Disaster Preparedness and Management, under the leadership of the Commissioner, Mr. Martin Owor, for the oversight and management of the entire exercise. The HRV assessment team was led by Ms. Ahimbisibwe Catherine, Senior Disaster Preparedness Officer supported by Mr. Ogwang Jimmy, Disaster Preparedness Officer and the team of consultants (GIS/DRR specialists); Dr. Bernard Barasa, and Mr. Nsiimire Peter, who provided technical support. Our gratitude goes to UNDP for providing funds to support the Hazard, Risk and Vulnerability Mapping. The team comprised of Mr. Steven Goldfinch – Disaster Risk Management Advisor, Mr. Gilbert Anguyo - Disaster Risk Reduction Analyst, and Mr. Ongom Alfred-Early Warning system Programmer. My appreciation also goes to Gomba District Team. The entire body of stakeholders who in one way or another yielded valuable ideas and time to support the completion of this exercise. Hon. Hilary O. Onek Minister for Relief, Disaster Preparedness and Refugees GOMBA DISTRICT HAZARD, RISK AND VULNERABILITY PROFILE i EXECUTIVE SUMMARY The multi-hazard vulnerability profile outputs from this assessment for Gomba District was a combination of spatial modeling using adaptive, sensitivity and exposure spatial layers and information captured from District Key Informant interviews and sub-county FGDs using a participatory approach. -

WHO UGANDA BULLETIN February 2016 Ehealth MONTHLY BULLETIN
WHO UGANDA BULLETIN February 2016 eHEALTH MONTHLY BULLETIN Welcome to this 1st issue of the eHealth Bulletin, a production 2015 of the WHO Country Office. Disease October November December This monthly bulletin is intended to bridge the gap between the Cholera existing weekly and quarterly bulletins; focus on a one or two disease/event that featured prominently in a given month; pro- Typhoid fever mote data utilization and information sharing. Malaria This issue focuses on cholera, typhoid and malaria during the Source: Health Facility Outpatient Monthly Reports, Month of December 2015. Completeness of monthly reporting DHIS2, MoH for December 2015 was above 90% across all the four regions. Typhoid fever Distribution of Typhoid Fever During the month of December 2015, typhoid cases were reported by nearly all districts. Central region reported the highest number, with Kampala, Wakiso, Mubende and Luweero contributing to the bulk of these numbers. In the north, high numbers were reported by Gulu, Arua and Koti- do. Cholera Outbreaks of cholera were also reported by several districts, across the country. 1 Visit our website www.whouganda.org and follow us on World Health Organization, Uganda @WHOUganda WHO UGANDA eHEALTH BULLETIN February 2016 Typhoid District Cholera Kisoro District 12 Fever Kitgum District 4 169 Abim District 43 Koboko District 26 Adjumani District 5 Kole District Agago District 26 85 Kotido District 347 Alebtong District 1 Kumi District 6 502 Amolatar District 58 Kween District 45 Amudat District 11 Kyankwanzi District -
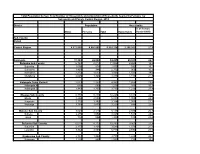
Population by Parish
Total Population by Sex, Total Number of Households and proportion of Households headed by Females by Subcounty and Parish, Central Region, 2014 District Population Households % of Female Males Females Total Households Headed HHS Sub-County Parish Central Region 4,672,658 4,856,580 9,529,238 2,298,942 27.5 Kalangala 31,349 22,944 54,293 20,041 22.7 Bujumba Sub County 6,743 4,813 11,556 4,453 19.3 Bujumba 1,096 874 1,970 592 19.1 Bunyama 1,428 944 2,372 962 16.2 Bwendero 2,214 1,627 3,841 1,586 19.0 Mulabana 2,005 1,368 3,373 1,313 21.9 Kalangala Town Council 2,623 2,357 4,980 1,604 29.4 Kalangala A 680 590 1,270 385 35.8 Kalangala B 1,943 1,767 3,710 1,219 27.4 Mugoye Sub County 6,777 5,447 12,224 3,811 23.9 Bbeta 3,246 2,585 5,831 1,909 24.9 Kagulube 1,772 1,392 3,164 1,003 23.3 Kayunga 1,759 1,470 3,229 899 22.6 Bubeke Sub County 3,023 2,110 5,133 2,036 26.7 Bubeke 2,275 1,554 3,829 1,518 28.0 Jaana 748 556 1,304 518 23.0 Bufumira Sub County 6,019 4,273 10,292 3,967 22.8 Bufumira 2,177 1,404 3,581 1,373 21.4 Lulamba 3,842 2,869 6,711 2,594 23.5 Kyamuswa Sub County 2,733 1,998 4,731 1,820 20.3 Buwanga 1,226 865 2,091 770 19.5 Buzingo 1,507 1,133 2,640 1,050 20.9 Maziga Sub County 3,431 1,946 5,377 2,350 20.8 Buggala 2,190 1,228 3,418 1,484 21.4 Butulume 1,241 718 1,959 866 19.9 Kampala District 712,762 794,318 1,507,080 414,406 30.3 Central Division 37,435 37,733 75,168 23,142 32.7 Bukesa 4,326 4,711 9,037 2,809 37.0 Civic Centre 224 151 375 161 14.9 Industrial Area 383 262 645 259 13.9 Kagugube 2,983 3,246 6,229 2,608 42.7 Kamwokya -

BMAU BRIEFING PAPER (12/17) May 2017
BMAU BRIEFING PAPER (12/17) May 2017 WHAT ARE THE KEY ISSUES IN THE HEALTH SECTOR? Overview Key Issues The health sector aims at producing a healthy and productive population that effectively contributes to socio- Remuneration packages for health staff are economic growth. This is achievable through provision of inadequate . accessible and quality health care to all people in Uganda through delivery of promotive, preventive, curative, Inadequate staffing has in part resulted in palliative and rehabilitative care (Second National non-utilisation of some key service delivery Development Plan [NDP II] 2015/16-2019/20 p.188) equipment. Human capital development is a key priority in NDPII. The The health facilities are experiencing drug sector was allocated Ug shs 1,827.26billion in FY2016/17 stock out in part due poor planning and representing a 44% increase in the allocation from the Ug budgeting resulting into a mismatch of supply shs 1,270.81billion allocated in FY2015/16. and demand. The health sector has exhibited a good allocative efficiency through the investments in infrastructure and Health facilities either lack, or received poor other services but a number of aspects in the sector that quality or incomplete packages of equipment. affect service delivery remain less attended. The briefing paper highlights the three important aspects that require attention to enhance service delivery. the 112 districts in Uganda had either a hospital or HCIV or both regardless of the infrastructure condition. Despite this progress in service availability, significant challenges remain to Introduction improve the quality of service delivery and address Good health is instrumental in facilitating socio- continuing health status issues such as infant and economic transformation. -

Strengthening OVCMIS Repor and Utilisation in Ngthening OVCMIS
Strengthening OVCMIS reporting and Utilisation in Gomba district Presented by Kashemeire e Obadiah & Magall Moritz MAKSPH‐CDC Medium m Term M&E Fellows 2011/12 Presentation Outline line • Background • Problem Statement • Project Objectives • Project Implementation • Project deliverables • Challenges • Lessons learnt • Recommendations • Acknowledgements Background • The Ministry of Gender, Labour and Social Development (MGLSD) is a lead government agency mandated to ensure that the rights of all children including Orphans and other Vulnerable (OVC) are promoted and upheld . • The Ministry works through district local governments to deliver decentralized child care and protection services for children. OVC‐ ‐MIS The OVC‐ Management Information System was established by the Ministry to monitor OVC implementation and evaluate performance of all stakeholders to ensure effective implementation of National OVC response esponse. The OVCMIS is based on the conceptual framework that links; • The needs of OVC and their households • The provision of services by government, donors and CSOs. • The demand and utilization of services by the OVC and their households ds. OVCMIS data flow flow • OVCMIS data flow Problem Statement 32 “new” Districts including Gomba do not receive any support to roll out OVCMIS from SUNRISE project which operates in 80 “old” districts. In Gomba, staff lacked the basic skills for OVCMIS data collection, analysis and online reporting. The focal office does not have a printer for printing data collection tools. There was no internet connectivity for online reporting. Parishes are very large with many villages. CDOs have no motorcycles. Project Implementation Area In view of the problems and the time and budget allocated to this project, Gomba district which is within easy reach of project implementers was selected to act as a pilot district where success stories, good practices and challenges will be documented and shared to inform implementation in the rest of the districts and municipalities. -

STATUTORY INSTRUMENTS SUPPLEMENT No. 5 3Rd February
STATUTORY INSTRUMENTS SUPPLEMENT No. 5 3rd February, 2012 STATUTORY INSTRUMENTS SUPPLEMENT to The Uganda Gazette No. 7 Volume CV dated 3rd February, 2012 Printed by UPPC, Entebbe, by Order of the Government. STATUTORY INSTRUMENTS 2012 No. 5. The Local Government (Declaration of Towns) Regulations, 2012. (Under sections 7(3) and 175(1) of the Local Governments Act, Cap. 243) In exercise of the powers conferred upon the Minister responsible for local governments by sections 7(3) and 175(1) of the Local Governments Act, in consultation with the districts and with the approval of Cabinet, these Regulations are made this 14th day of July, 2011. 1. Title These Regulations may be cited as the Local Governments (Declaration of Towns) Regulations, 2012. 2. Declaration of Towns The following areas are declared to be towns— (a) Amudat - consisting of Amudat trading centre in Amudat District; (b) Buikwe - consisting of Buikwe Parish in Buikwe District; (c) Buyende - consisting of Buyende Parish in Buyende District; (d) Kyegegwa - consisting of Kyegegwa Town Board in Kyegegwa District; (e) Lamwo - consisting of Lamwo Town Board in Lamwo District; - consisting of Otuke Town Board in (f) Otuke Otuke District; (g) Zombo - consisting of Zombo Town Board in Zombo District; 259 (h) Alebtong (i) Bulambuli (j) Buvuma (k) Kanoni (l) Butemba (m) Kiryandongo (n) Agago (o) Kibuuku (p) Luuka (q) Namayingo (r) Serere (s) Maracha (t) Bukomansimbi (u) Kalungu (v) Gombe (w) Lwengo (x) Kibingo (y) Nsiika (z) Ngora consisting of Alebtong Town board in Alebtong District; -

Uganda Country Operational Plan 2018 Strategic Direction Summary
UGANDA Country Operational Plan (COP) 2018 Strategic Direction Summary April 17, 2018 Table of Contents 1.0 Goal Statement .................................................................................................................... 3 2.0 Epidemic, Response, and Program Context ....................................................................... 5 2.1 Summary Statistics, Disease Burden and Country Profile .......................................................... 5 2.2 Investment Profile ...................................................................................................................... 18 2.3 National Sustainability Profile Update ..................................................................................... 22 2.4 Alignment of PEPFAR Investments Geographically to Disease Burden ................................. 26 2.5 Stakeholder Engagement ........................................................................................................... 28 3.0 Geographic and Population Prioritization ....................................................................... 31 4.0 Program Activities for Epidemic Control in Scale-Up Locations and Populations........ 33 4.1 Finding the missing, getting them on treatment, and retaining them .................................... 33 4.2 Prevention, specifically detailing programs for priority programming................................... 50 HIV prevention and risk avoidance for AGYW and OVC .......................................................... 50 Key and Priority -

Office of the Auditor General the Republic of Uganda
OFFICE OF THE AUDITOR GENERAL THE REPUBLIC OF UGANDA REPORT OF THE AUDITOR GENERAL ON THE FINANCIAL STATEMENTS OF GOMBA DISTRICT LOCAL GOVERNMENT FOR THE YEAR ENDED 30TH JUNE 2017 OFFICE OF THE AUDITOR GENERAL UGANDA TABLE OF CONTENTS LIST OF ACRONYMS ......................................................................................................... 2 Key Audit Matters ............................................................................................................. 2 Utilization of Medicines and Medical Supplies .......................................... 2 Stock out ..................................................................................................................... 3 Expired drugs ............................................................................................................. 3 Key Vacant Positions ................................................................................................. 4 Other Matter ...................................................................................................................... 4 Low Recovery of Youth Livelihood Program funds. ............................................. 4 Encroachment on Forest Reserves ......................................................................... 5 Unoperational Theatre at Maddu HC IV ................................................................ 5 Understaffing ............................................................................................................. 6 Management’s Responsibility -
Of the Constitution Providing for Creation of New Counties
A MOTION FOR RESOLUTION OF PARLIAMENT UNDER ARTICLE 179 CLAUSE (4) OF THE CONSTITUTION PROVIDING FOR CREATION OF NEW COUNTIES WHEREAS Article 179(4) provides for the criteria for alteration of boundaries of or creation of administrative units including counties; AND WHEREAS Section 7(7) empowers Parliament to approve alteration of boundaries of or creation of a new county; AND WHEREAS it is considered necessary to create the counties specified hereunder for the effective representation and streamlining administration, internal emancipation and the reduction of marginalization and the need to improve planning of those areas and bring services closer to the people; having taken into account the means of communication, the geographical features, the destiny of the population and the wishes of the people concerned; AND WHEREAS the creation of the said new counties is supported by a majority of all the Members of Parliament: NOW THEREFORE BE IT RESOLVED BY PARLIAMENT 1) That the following new counties be created in Uganda as indicated herein: i. Agago North County out of Agago County in Agago District and the remaining part be called Agago County; ii. Orungo County out of Amuria County in Amuria District and the remaining part be called Amuria County; iii. Lutseshe County out of Manjiya County in Bududa District and the remaining part be called Manjiya County; iv. Kachumbala County out of Bukedea County in Bukedea District and the remaining part be called Bukedea County; v. Bukomansimbi South County out of Bukomansimbi County in Bukomansimbi District and the remaining part be called Bukomansimbi North County; vi. Elgon County out of Bulambuli County in Bulambuli District and the remaining part be called Bulambuli County; vii. -

Human Resources for Health Audit Report
HUMAN RESOURCES FOR HEALTH AUDIT REPORT SEPTEMBER, 2014 Table of Contents Executive Summary ............................................................................................................................................... 10 1. Methods ........................................................................................................................................................ 11 1.1. Staffing norms ........................................................................................................................................... 11 1.2. Population ................................................................................................................................................. 11 1.3. Data collection method ............................................................................................................................. 11 1.4. Data management, analysis and presentations ........................................................................................ 12 2. Findings ......................................................................................................................................................... 12 2.1. Overall staffing level ................................................................................................................................. 12 2.2. Staffing in Regional Referral Hospitals ...................................................................................................... 13 3.3 Staffing in General Hospitals .................................................................................................................... -

Achieving Reliable Access to Water in Rural Communities
Achieving Reliable Access to Water in Rural Communities A Study for the Water Compass Authors: Marije van den Broek and Dr. Julia Brown [email protected] [email protected] Figure 1: Children collecting water from a valley dam 1 Contents page Executive Summary…………………………………………………………....3 1. Introduction and Rationale………………………………………………...6 2. Background…………………………………………………………………..8 2.1. Country overview of rural water provision and policy in Uganda…………….. 8 2.2. Gomba District……………………………………………………………………... 9 3. Achieving Reliable Access to Water in Rural Communities………..11 3.1. The Community Based Management (CBM) model…………………………..12 3.2 The case for investing in the sustainability of rural water services………….. 13 3.3 What are the recurrent costs of handpumps?.................................................14 3.4 Rural Water Management Models………………………………………………. 15 4. Study Methods …………………………………………………………….. 17 5. Findings……………………………………………………………………....23 5.1 Assessment of current water arrangements and management practices ……23 5.2 Selection of the water management model……………………………………..28 5.3 Visiting Demonstration Sites……………………………………………………....34 6. Recommendations and Conclusions……………………………………37 References………………………………………………………………………40 Appendix 1 Water Management Models……………………………………42 2 Executive summary The Water Compass is a Water, Sanitation, and Hygiene (WASH) organisation operational in Gomba District in Uganda. The ambition of the organisation is to improve access to water in rural sub-Saharan regions with a special emphasis on post-construction sustainability of boreholes equipped with a handpump. The focus of the Water Compass on post-construction sustainability prior to hardware construction represents a unique and forward-thinking approach that differentiates the organisation from other NGOs in the rural water sector. The poor functionality performance of constructed sources is a concern for the sector in general and the focus of academic studies by van den Broek and Brown. -

PEPFAR Uganda Country Operational Plan (COP) 2019 Strategic Direction Summary April 12, 2019
PEPFAR Uganda Country Operational Plan (COP) 2019 Strategic Direction Summary April 12, 2019 Table of Contents 1.0 Goal Statement .................................................................................................................... 4 2.0 Epidemic, Response, and Program Context ....................................................................... 7 2.1 Summary Statistics, Disease Burden and Country Profile ................................................. 7 2.2 Investment Profile ............................................................................................................................. 19 2.3 National Sustainability Profile Update .............................................................................................. 24 2.4 Alignment of PEPFAR Investments Geographically to Disease Burden ............................................ 28 2.5 Stakeholder Engagement .................................................................................................................. 29 3.0 Geographic and Population Prioritization ...................................................................... 32 4.0 Program Activities for Epidemic Control in Scale-Up Locations and Populations .. 33 4.1 Finding the missing, getting them on treatment, and retaining them ensuring viral suppression .. 34 4.2 Prevention, specifically detailing programs for priority programming: ........................................... 52 4.2.a. OVC and Child-Focused COP19 Interventions ..........................................................................