Hypoxia 3 Pannel Brochure V2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypothermia Brochure
Visit these websites for more water safety and hypothermia prevention in- formation. What is East Pierce Fire & Rescue Hypothermia? www.eastpiercefire.org Hypothermia means “low temperature”. Washington State Drowning When your body is exposed to cold tem- Prevention Coalition Hypothermia www.drowning-prevention.org perature, it tries to protect itself by keeping a normal body temperature of 98.6°F. It Children’s Hospital & tries to reduce heat loss by shivering and Regional Medical Center In Our Lakes moving blood from your arms and legs to www.seattlechildrens.org the core of your body—head, chest and and Rivers abdomen. Hypothermia Prevention, Recognition and Treatment www.hypothermia.org Stages of Hypothermia Boat Washington Mild Hypothermia www.boatwashington.org (Core body temperature of 98.6°— 93.2°F) Symptoms: Shivering; altered judg- ment; numbness; clumsiness; loss of Boat U.S. Foundation dexterity; pain from cold; and fast www.boatus.com breathing. Boat Safe Moderate Hypothermia www.boatsafe.com (Core body temperature of 93.2°—86°F) Symptoms: Semiconscious to uncon- scious; shivering reduced or absent; lips are blue; slurred speech; rigid n in muscles; appears drunk; slow Eve breathing; and feeling of warmth can occur. mer! Headquarters Station Sum Severe Hypothermia 18421 Old Buckley Hwy (Core body temperature below 86°F) Bonney Lake, WA 98391 Symptoms: Coma; heart stops; and clinical death. Phone: 253-863-1800 Fax: 253-863-1848 Email: [email protected] Know the water. Know your limits. Wear a life vest. By choosing to swim in colder water you Waters in Western Common Misconceptions Washington reduce your survival time. -

Asphyxia Neonatorum
CLINICAL REVIEW Asphyxia Neonatorum Raul C. Banagale, MD, and Steven M. Donn, MD Ann Arbor, Michigan Various biochemical and structural changes affecting the newborn’s well being develop as a result of perinatal asphyxia. Central nervous system ab normalities are frequent complications with high mortality and morbidity. Cardiac compromise may lead to dysrhythmias and cardiogenic shock. Coagulopathy in the form of disseminated intravascular coagulation or mas sive pulmonary hemorrhage are potentially lethal complications. Necrotizing enterocolitis, acute renal failure, and endocrine problems affecting fluid elec trolyte balance are likely to occur. Even the adrenal glands and pancreas are vulnerable to perinatal oxygen deprivation. The best form of management appears to be anticipation, early identification, and prevention of potential obstetrical-neonatal problems. Every effort should be made to carry out ef fective resuscitation measures on the depressed infant at the time of delivery. erinatal asphyxia produces a wide diversity of in molecules brought into the alveoli inadequately com Pjury in the newborn. Severe birth asphyxia, evi pensate for the uptake by the blood, causing decreases denced by Apgar scores of three or less at one minute, in alveolar oxygen pressure (P02), arterial P02 (Pa02) develops not only in the preterm but also in the term and arterial oxygen saturation. Correspondingly, arte and post-term infant. The knowledge encompassing rial carbon dioxide pressure (PaC02) rises because the the causes, detection, diagnosis, and management of insufficient ventilation cannot expel the volume of the clinical entities resulting from perinatal oxygen carbon dioxide that is added to the alveoli by the pul deprivation has been further enriched by investigators monary capillary blood. -

The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board
The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board Introduction • Nitrogen makes up 78% of the air we breath; because of this it is often assumed that nitrogen is not hazardous. • However, nitrogen is safe to breath only if it is mixed with an appropriate amount of oxygen. • Additional nitrogen (lower oxygen) cannot be detected by the sense of smell. Introduction • Nitrogen is used commercially as an inerting agent to keep material free of contaminants (including oxygen) that may corrode equipment, present a fire hazard, or be toxic. • A lower oxygen concentration (e.g., caused by an increased amount of nitrogen) can have a range of effects on the human body and can be fatal if if falls below 10% Effects of Oxygen Deficiency on the Human Body Atmospheric Oxygen Concentration (%) Possible Results 20.9 Normal 19.0 Some unnoticeable adverse physiological effects 16.0 Increased pulse and breathing rate, impaired thinking and attention, reduced coordination 14.0 Abnormal fatigue upon exertion, emotional upset, faulty coordination, poor judgment 12.5 Very poor judgment and coordination, impaired respiration that may cause permanent heart damage, nausea, and vomiting <10 Inability to move, loss of consciousness, convulsions, death Source: Compressed Gas Association, 2001 Statistics on Incidents CSB reviewed cases of nitrogen asphyxiation that occurred in the US between 1992 and 2002 and determined the following: • 85 incidents of nitrogen asphyxiation resulted in 80 deaths and 50 injuries. • The majority of -

Pulmonary Barotrauma During Hypoxia in a Diver While Underwater
POLISH HYPERBARIC RESEARCH 2(71)2020 Journal of Polish Hyperbaric Medicine and Technology Society PULMONARY BAROTRAUMA DURING HYPOXIA IN A DIVER WHILE UNDERWATER Brunon Kierznikowicz, Władysław Wolański, Romuald Olszański Institute of Maritime and Tropical Medicine of the Military Medical Academy, Gdynia, Poland ABSTRACT The article describes a diver performing a dive at small depths in a dry suit, breathing from a single-stage apparatus placed on his back. As a result of training deficiencies, the diver began breathing from inside the suit, which led to hypoxia and subsequent uncontrolled ascent. Upon returning to the surface, the diver developed neurological symptoms based on which a diagnosis of pulmonary barotrauma was made. The diver was successfully treated with therapeutic recompression-decompression. Keywords: diving, accident, hypoxia, pulmonary barotrauma. ARTICLE INFO PolHypRes 2020 Vol. 71 Issue 2 pp. 45 – 50 ISSN: 1734-7009 eISSN: 2084-0535 Casuistic (case description) article DOI: 10.2478/phr-2020-0009 Pages: 6, figures: 0, tables: 1 Originally published in the Naval Health Service Yearbook 1977-1978 page www of the periodical: www.phr.net.pl Acceptance for print in PHR: 27.10.2019 r. Publisher Polish Hyperbaric Medicine and Technology Society 2020 Vol. 71 Issue 2 INTRODUCTION that he suddenly experienced an "impact" from an increased amount of air flowing into his lungs during In recent years, we can observe a continuous inhalation. Fearing a lung injury, he immediately pulled the dynamic development of diving technology. At the same mouthpiece out of his mouth and started breathing air time, the spectrum of works carried out by scuba divers for from inside the suit for about 2 minutes. -

Clinical Management of Severe Acute Respiratory Infections When Novel Coronavirus Is Suspected: What to Do and What Not to Do
INTERIM GUIDANCE DOCUMENT Clinical management of severe acute respiratory infections when novel coronavirus is suspected: What to do and what not to do Introduction 2 Section 1. Early recognition and management 3 Section 2. Management of severe respiratory distress, hypoxemia and ARDS 6 Section 3. Management of septic shock 8 Section 4. Prevention of complications 9 References 10 Acknowledgements 12 Introduction The emergence of novel coronavirus in 2012 (see http://www.who.int/csr/disease/coronavirus_infections/en/index. html for the latest updates) has presented challenges for clinical management. Pneumonia has been the most common clinical presentation; five patients developed Acute Respira- tory Distress Syndrome (ARDS). Renal failure, pericarditis and disseminated intravascular coagulation (DIC) have also occurred. Our knowledge of the clinical features of coronavirus infection is limited and no virus-specific preven- tion or treatment (e.g. vaccine or antiviral drugs) is available. Thus, this interim guidance document aims to help clinicians with supportive management of patients who have acute respiratory failure and septic shock as a consequence of severe infection. Because other complications have been seen (renal failure, pericarditis, DIC, as above) clinicians should monitor for the development of these and other complications of severe infection and treat them according to local management guidelines. As all confirmed cases reported to date have occurred in adults, this document focuses on the care of adolescents and adults. Paediatric considerations will be added later. This document will be updated as more information becomes available and after the revised Surviving Sepsis Campaign Guidelines are published later this year (1). This document is for clinicians taking care of critically ill patients with severe acute respiratory infec- tion (SARI). -
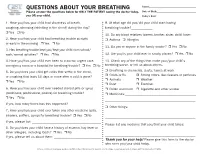
QUESTIONS ABOUT YOUR BREATHING Name:______Please Answer the Questions Below for ONLY the PATIENT Seeing the Doctor Today, Date of Birth:______You OR Your Child
QUESTIONS ABOUT YOUR BREATHING Name:_____________________________________ Please answer the questions below for ONLY THE PATIENT seeing the doctor today, Date of Birth:_______________________________ you OR your child. Today’s Date:_______________________________ 1. Have you/has your child had shortness of breath, 9. At what age did you/did your child start having coughing, wheezing (whistling in the chest) during the day? breathing trouble?_____________ r Yes r No 10. Do any blood relatives (parent, brother, sister, child) have: 2. Have you/has your child had breathing trouble at night r Asthma r Allergies or early in the morning r Yes r No 11. Do you or anyone in the family smoke? r Yes r No 3. Has breathing trouble kept you/kept your child from school/ work/normal activities? r Yes r No 12. Are you/is your child ever in smoky places? r Yes r No 4. Have you/has your child ever been to a doctor, urgent care, 13. Check any of the things that make your/your child’s emergency room or a hospital for breathing trouble? r Yes r No breathing worse, or tell us about others. 5. Do you/does your child get colds that settle in the chest, r Breathing in chemicals, dusts, fumes at work r Colds or flu r Strong odors, like cleaners or perfumes or coughing that lasts 10 days or more after a cold is gone? r Animals r Weather r Yes r No r Dust r Exercise 6. Have you/has your child ever needed steroid pills or syrup r Pollen and mold r Cigarette and other smoke (prednisone, prednisolone, prelone) for breathing trouble? r Medicines:___________________________________________ r Yes r No _______________________________________________________ If yes, how many times has this happened? ___________________ r Other things: 7. -

Gas Exchange in the Prone Posture
RESPIRATORY CARE Paper in Press. Published on May 30, 2017 as DOI: 10.4187/respcare.05512 Gas Exchange in the Prone Posture Nicholas J Johnson MD, Andrew M Luks MD, and Robb W Glenny MD Introduction Overview of Gas Exchange Lung Structure Normal Exchange of Oxygen and Carbon Dioxide Abnormal Exchange of Oxygen and Carbon Dioxide Gas Exchange in the Prone Posture Under Normal Conditions Spatial Distribution of Ventilation Spatial Distribution of Perfusion Ventilation and Perfusion Matching Mechanisms by Which the Prone Posture Improves Gas Exchange in Animal Models of ARDS Additional Physiologic Effects of the Prone Posture Clinical Trials Summary The prone posture is known to have numerous effects on gas exchange, both under normal condi- tions and in patients with ARDS. Clinical studies have consistently demonstrated improvements in oxygenation, and a multi-center randomized trial found that, when implemented within 48 h of moderate-to-severe ARDS, placing subjects in the prone posture decreased mortality. Improve- ments in gas exchange occur via several mechanisms: alterations in the distribution of alveolar ventilation, redistribution of blood flow, improved matching of local ventilation and perfusion, and reduction in regions of low ventilation/perfusion ratios. Ventilation heterogeneity is reduced in the prone posture due to more uniform alveolar size secondary to a more uniform vertical pleural pressure gradient. The prone posture results in more uniform pulmonary blood flow when com- pared with the supine posture, due to an anatomical bias for greater blood flow to dorsal lung regions. Because both ventilation and perfusion heterogeneity decrease in the prone posture, gas exchange improves. -

Near Drowning
Near Drowning McHenry Western Lake County EMS Definition • Near drowning means the person almost died from not being able to breathe under water. Near Drownings • Defined as: Survival of Victim for more than 24* following submission in a fluid medium. • Leading cause of death in children 1-4 years of age. • Second leading cause of death in children 1-14 years of age. • 85 % are caused from falls into pools or natural bodies of water. • Male/Female ratio is 4-1 Near Drowning • Submersion injury occurs when a person is submerged in water, attempts to breathe, and either aspirates water (wet) or has laryngospasm (dry). Response • If a person has been rescued from a near drowning situation, quick first aid and medical attention are extremely important. Statistics • 6,000 to 8,000 people drown each year. Most of them are within a short distance of shore. • A person who is drowning can not shout for help. • Watch for uneven swimming motions that indicate swimmer is getting tired Statistics • Children can drown in only a few inches of water. • Suspect an accident if you see someone fully clothed • If the person is a cold water drowning, you may be able to revive them. Near Drowning Risk Factor by Age 600 500 400 300 Male Female 200 100 0 0-4 yr 5-9 yr 10-14 yr 15-19 Ref: Paul A. Checchia, MD - Loma Linda University Children’s Hospital Near Drowning • “Tragically 90% of all fatal submersion incidents occur within ten yards of safety.” Robinson, Ped Emer Care; 1987 Causes • Leaving small children unattended around bath tubs and pools • Drinking -
Breathing Air Quality, Sampling and Testing
Breathing Air Quality, Sampling and Testing Environmental Health Laboratory Department of Environmental and Occupational Health Sciences School of Public Health University of Washington Funding and support from The State of Washington Department of Labor & Industries Safety & Health Investment Projects Medical Aid and Accident Fund Breathing Air Quality, Sampling, and Testing Environmental Health Laboratory Department of Environmental and Occupational Health Sciences School of Public Health University of Washington Funding and support from The State of Washington Department of Labor & Industries Safety & Health Investment Projects Medical Aid and Accident Funds 1 University of Washington Environmental Health Laboratory Table of Contents Overview ...............................................................................1 Background ...........................................................................2 Regulated Components of Breathing Air ...............................7 Performance of Breathing Air Testing Kits ............................9 Laboratory Accreditation .....................................................18 Guidance Summary .............................................................19 Glossary ..............................................................................20 References ...........................................................................22 List of Tables Table 1. Breathing Air Quality Specifications ........................2 Table 2. Description of Kits Tested ........................................9 -

Effects of Smoking on Acute Hypobaric Hypoxia Tolerance
Ercan et al. Effects of Smoking on Hypoxia Tolerance ORI GI NAL AR TIC LE DOI: 10.4274/hamidiyemedj.galenos.2021.29291 Hamidiye Med J 2021;2(1):37-42 Effects of Smoking on Acute Hypobaric Hypoxia Tolerance Sigara Kullanımının Akut Hipobarik Hipoksi Toleransı Üzerine Etkisi Erdinç Ercan1, Menduh Şavaş İlbasmış2, Cantürk Taşçı3 1Health Science University, Department of Aerospace Medicine, Ankara, Turkey 2Yunus Emre State Hospital, Clinic of Hyperbaric Oxygen Therapy, Eskişehir, Turkey 3Health Science University, Department of Pulmonology, Ankara, Turkey Background: Smoking may impair oxygen transport ability of blood and airway destructions might be seen in long term smokers. After 1-3 cigarette smoking, it leads to a rise in carboxyhemoglobin level in blood, and it has a negative effect such as taking extra 5,000-8,000 feet altitude. Thus, it is thought that smoking before or in-flight may contribute to altitude hypoxia. The objective of this study was to evaluate the effects of smoking on acute hypobaric hypoxia tolerance at 30,000 ft. simulated altitude. Materials and Methods: This study was planned prospectively, and a standardized survey that consisted of smoking status and demographic characteristics of subjects was applied before the procedures. Aircrews are exposed to high altitude during “Hypobaric Hypoxia Training” in an altitude chamber. Pulse oximeter measurements were done to analyze oxygen saturations during different stages of the hypoxia trainings. T C Results: Seventy eight male healthy aircrews were included in this study. Twenty five (32.1%) of subjects stated that they were currently smoking (4.9±2.6 years). Hypoxic pulse oximeter mean values of the Nonsmoker Group were higher than those of the Smoker Group (p>0.05). -

Diving Air Compressor - Wikipedia, the Free Encyclopedia Diving Air Compressor from Wikipedia, the Free Encyclopedia
2/8/2014 Diving air compressor - Wikipedia, the free encyclopedia Diving air compressor From Wikipedia, the free encyclopedia A diving air compressor is a gas compressor that can provide breathing air directly to a surface-supplied diver, or fill diving cylinders with high-pressure air pure enough to be used as a breathing gas. A low pressure diving air compressor usually has a delivery pressure of up to 30 bar, which is regulated to suit the depth of the dive. A high pressure diving compressor has a delivery pressure which is usually over 150 bar, and is commonly between 200 and 300 bar. The pressure is limited by an overpressure valve which may be adjustable. A small stationary high pressure diving air compressor installation Contents 1 Machinery 2 Air purity 3 Pressure 4 Filling heat 5 The bank 6 Gas blending 7 References 8 External links A small scuba filling and blending station supplied by a compressor and Machinery storage bank Diving compressors are generally three- or four-stage-reciprocating air compressors that are lubricated with a high-grade mineral or synthetic compressor oil free of toxic additives (a few use ceramic-lined cylinders with O-rings, not piston rings, requiring no lubrication). Oil-lubricated compressors must only use lubricants specified by the compressor's manufacturer. Special filters are used to clean the air of any residual oil and water(see "Air purity"). Smaller compressors are often splash lubricated - the oil is splashed around in the crankcase by the impact of the crankshaft and connecting A low pressure breathing air rods - but larger compressors are likely to have a pressurized lubrication compressor used for surface supplied using an oil pump which supplies the oil to critical areas through pipes diving at the surface control point and passages in the castings. -

Title: Recognizing Barotrauma As an Unexpected Complication of High Flow Nasal Cannula
Title: Recognizing barotrauma as an unexpected complication of high flow nasal cannula Introduction: Spontaneous pneumomediastinum (SPM) is a rare condition defined as free air in the mediastinum without an apparent trauma. It is commonly associated with barotrauma in asthma and COPD patients. High flow nasal cannula (HFNC) has been routinely used for hypoxemic respiratory failure. We present a case of the development of SPM with extensive subcutaneous emphysema with the use of HFNC for hypoxic respiratory failure. Case Presentation: 78 year old Caucasian female with history of interstitial pulmonary fibrosis and COPD was discharged to LTACH after prolonged hospitalization for influenza-A infection complicated by acute on chronic respiratory failure. She was started on supplemental oxygen using HFNC that was progressively increased to 60 liters/min with 100% FiO2 for persistent hypoxia. Over the next four days, she was noted to have worsening facial and neck swelling with progressive dyspnea leading to transfer to the hospital. CT scan of chest noted for extensive pneumomediastinum involving the middle and anterior mediastinum with extensive subcutaneous emphysema throughout the anterior and moderately posterior chest wall extending to lower neck. Lung parenchyma revealed underlying interstitial with patchy airspace disease without evident pneumothorax. She was started on 100% FIO2 with non- rebreather mask. For symptomatic relief, Cardiothoracic surgery performed bilateral anterior chest blowhole incisions and application of negative vacuum-assisted closure on anterior chest with dramatic improvement in subcutaneous emphysema and facial swelling with persistent pneumomediastinum. Patent’s pneumomediastinum and respiratory failure persisted with high oxygen requirement with non- rebreather mask. Due to underlying advanced lung disease and persistent respiratory failure , patient’s family opted for palliative management with comfort measure and patient was transferred to hospice care.