Assessment of the Hand in Cerebral Palsy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ICD-10 Diagnoses on Router
L ARTHRITIS R L HAND R L ANKLE R L FRACTURES R OSTEOARTHRITIS: PRIMARY, 2°, POST TRAUMA, POST _____ CONTUSION ACHILLES TEN DYSFUNCTION/TENDINITIS/RUPTURE FLXR TEN CLAVICLE: STERNAL END, SHAFT, ACROMIAL END CRYSTALLINE ARTHRITIS: GOUT: IDIOPATHIC, LEAD, CRUSH INJURY AMPUTATION TRAUMATIC LEVEL SCAPULA: ACROMION, BODY, CORACOID, GLENOID DRUG, RENAL, OTHER DUPUYTREN’S CONTUSION PROXIMAL HUMERUS: SURGICAL NECK 2 PART 3 PART 4 PART CRYSTALLINE ARTHRITIS: PSEUDOGOUT: HYDROXY LACERATION: DESCRIBE STRUCTURE CRUSH INJURY PROXIMAL HUMERUS: GREATER TUBEROSITY, LESSER TUBEROSITY DEP DIS, CHONDROCALCINOSIS LIGAMENT DISORDERS EFFUSION HUMERAL SHAFT INFLAMMATORY: RA: SEROPOSITIVE, SERONEGATIVE, JUVENILE OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ LOOSE BODY HUMERUS DISTAL: SUPRACONDYLAR INTERCONDYLAR REACTIVE: SECONDARY TO: INFECTION ELSEWHERE, EXTENSION OR NONE INTESTINAL BYPASS, POST DYSENTERIC, POST IMMUNIZATION PAIN OCD TALUS HUMERUS DISTAL: TRANSCONDYLAR NEUROPATHIC CHARCOT SPRAIN HAND: JOINT? OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ HUMERUS DISTAL: EPICONDYLE LATERAL OR MEDIAL AVULSION INFECT: PYOGENIC: STAPH, STREP, PNEUMO, OTHER BACT TENDON RUPTURES: EXTENSOR OR FLEXOR PAIN HUMERUS DISTAL: CONDYLE MEDIAL OR LATERAL INFECTIOUS: NONPYOGENIC: LYME, GONOCOCCAL, TB TENOSYNOVITIS SPRAIN, ANKLE, CALCANEOFIBULAR ELBOW: RADIUS: HEAD NECK OSTEONECROSIS: IDIOPATHIC, DRUG INDUCED, SPRAIN, ANKLE, DELTOID POST TRAUMATIC, OTHER CAUSE SPRAIN, ANKLE, TIB-FIB LIGAMENT (HIGH ANKLE) ELBOW: OLECRANON WITH OR WITHOUT INTRA ARTICULAR EXTENSION SUBLUXATION OF ANKLE, -

Upper Extremity
Upper Extremity Shoulder Elbow Wrist/Hand Diagnosis Left Right Diagnosis Left Right Diagnosis Left Right Adhesive capsulitis M75.02 M75.01 Anterior dislocation of radial head S53.015 [7] S53.014 [7] Boutonniere deformity of fingers M20.022 M20.021 Anterior dislocation of humerus S43.015 [7] S43.014 [7] Anterior dislocation of ulnohumeral joint S53.115 [7] S53.114 [7] Carpal Tunnel Syndrome, upper limb G56.02 G56.01 Anterior dislocation of SC joint S43.215 [7] S43.214 [7] Anterior subluxation of radial head S53.012 [7] S53.011 [7] DeQuervain tenosynovitis M65.42 M65.41 Anterior subluxation of humerus S43.012 [7] S43.011 [7] Anterior subluxation of ulnohumeral joint S53.112 [7] S53.111 [7] Dislocation of MCP joint IF S63.261 [7] S63.260 [7] Anterior subluxation of SC joint S43.212 [7] S43.211 [7] Contracture of muscle in forearm M62.432 M62.431 Dislocation of MCP joint of LF S63.267 [7] S63.266 [7] Bicipital tendinitis M75.22 M75.21 Contusion of elbow S50.02X [7] S50.01X [7] Dislocation of MCP joint of MF S63.263 [7] S63.262 [7] Bursitis M75.52 M75.51 Elbow, (recurrent) dislocation M24.422 M24.421 Dislocation of MCP joint of RF S63.265 [7] S63.264 [7] Calcific Tendinitis M75.32 M75.31 Lateral epicondylitis M77.12 M77.11 Dupuytrens M72.0 Contracture of muscle in shoulder M62.412 M62.411 Lesion of ulnar nerve, upper limb G56.22 G56.21 Mallet finger M20.012 M20.011 Contracture of muscle in upper arm M62.422 M62.421 Long head of bicep tendon strain S46.112 [7] S46.111 [7] Osteochondritis dissecans of wrist M93.232 M93.231 Primary, unilateral -

The Rheumatoid Thumb
THE RHEUMATOID THUMB BY ANDREW L. TERRONO, MD The thumb is frequently involved in patients with rheumatoid arthritis. Thumb postures can be grouped into a number of deformities. Deformity is determined by a complex interaction of the primary joint, the adjacent joints, and tendon function and integrity. Joints adjacent to the primarily affected one usually assume an opposite posture. If they do not, tendon ruptures should be suspected. Surgical treatment is individualized for each patient and each joint, with consideration given to adjacent joints. The treatment consists of synovectomy, capsular reconstruction, tendon reconstruction, joint stabilization, arthrodesis, or arthroplasty. Copyright © 2001 by the American Society for Surgery of the Hand he majority of patients with rheumatoid ar- ring between the various joints. Any alteration of thritis will develop thumb involvement.1,2,3 posture at one level has an effect on the adjacent joint. TThe deformities encountered in the rheuma- The 6 patterns of thumb postures described here, toid patient are varied and are the result of changes unfortunately, do not exhaust the deformities one taking place both intrinsically and extrinsically to the encounters in rheumatoid arthritis (Table 1). It is thumb. Synovial hypertrophy within the individual possible, for example, for the patient to stretch the thumb joints leads not only to destruction of articular supporting structures of a joint, causing a flexion, cartilage, but can also stretch out the supporting extension, or lateral deformity. However, instead of collateral ligaments and joint capsules. As a result, the adjacent joint assuming the opposite posture, it each joint can become unstable and react to the may assume an abnormal position secondary to a stresses applied to it both in function against the other tendon rupture. -
![August 2011 [KZ 6266] Sub](https://docslib.b-cdn.net/cover/0451/august-2011-kz-6266-sub-1440451.webp)
August 2011 [KZ 6266] Sub
August 2011 [KZ 6266] Sub. Code : 6266 BACHELOR OF PHYSIOTHERAPY EXAMINATION FOURTH YEAR / SEVENTH SEMESTER CLINICAL ORTHOPAEDICS Q.P. Code : 746266 Time : Three hours Maximum : 100 marks ANSWER ALL QUESTIONS I. LONG ESSAYS (2X20=40) 1. Describe the mechanism of injury, complications and management of supra- condylar fracture of humerus. 2. Outline the etiopathology of Rheumatoid arthritis. Describe the deformities that occur in a rheumatoid hand and its management. II. SHORT NOTES (8X5=40) 1. Periarthritis shoulder. 2. Scaphoid fracture. 3. Sequestrum. 4. Cobb’s angle. 5. Cervical rib. 6. Torticollis. 7. Spondylolisthesis. 8. Fracture Patella. III. SHORT ANSWERS (10X2=20) 1. Green stick fracture. 2. Hallux Valgus. 3. Subluxation. 4. Carpal bones. 5. Delayed union. 6. Volkman’s sign. 7. Mc. Murrays test. 8. Scapulo-humeral rhythm. 9. Antalgic gait. 10.Hypothenar muscles of hand. ******* February 2012 [LA 6266] Sub. Code: 6266 BACHELOR OF PHYSIOTHERAPY EXAMINATION FOURTH YEAR / SEVENTH SEMESTER CLINICAL ORTHOPAEDICS Q.P. Code: 746266 Time: Three Hours Maximum: 100 marks Answer ALL questions I. Elaborate on: (2X20=40) 1. Describe the causes, clinical features and management of recurrent dislocation of the shoulder. 2. Describe the clinical features, complications and management of a patient with fracture of D8 vertebra with paraplegia. II. Write notes on: (8X5=40) 1. DeQuervains disease. 2. March fracture. 3. Ulnar claw hand. 4. Fracture disease. 5. Anterior cruciate ligament. 6. Potts fracture. 7. Shoulder hand syndrome 8. Myositis Ossificans III. Short Answers: (10X2=20) 1. Z-Thumb deformity. 2. Hallux valgus. 3. Guillotine amputation. 4. Mallet finger. 5. Elys test 6. Complications of Scaphoid fracture. -

Spectrum of Joint Deformities in Children with Juvenile Idiopathic Arthritis Samia Naz1, Misbah Asif2, Farrah Naz1, Hina Farooq3 and Muhammad Haroon Hamid1
CLINICAL PRACTICE ARTICLE Spectrum of Joint Deformities in Children with Juvenile Idiopathic Arthritis Samia Naz1, Misbah Asif2, Farrah Naz1, Hina Farooq3 and Muhammad Haroon Hamid1 ABSTRACT Objective: To determine the frequency and types of joint deformities in children with juvenile idiopathic arthritis and their association with clinical parameters and rheumatoid factor. Study Design: Cross-sectional study. Place and Duration of Study: Rheumatology Outpatient Clinic, the Children's Hospital and the Institute of Child Health, Lahore, from September 2014 to February 2015. Methodology: All patients of both genders of less than 16 years of age, who fulfilled the International League of Association for Rheumatology (ILAR) criteria for Juvenile Idiopathic Arthritis (JIA), were enrolled in this study. Their demographic data, duration of disease at the time of presentation, types of JIA, various joint deformities and rheumatoid factor (RF) were documented. Statistical analysis of data was done on SPSS version 16. Chi-square test was applied to determine the association of clinical deformity with age of patients, disease duration at presentation, types of JIA and RF. Results: Out of 70 patients enrolled during the study period, 51.4% were boys with mean age at presentation being 9.44 ±3.89 years (2-7 years) and median duration of disease being 24 months (interquartile range 42 months). Forty patients (57.1%) had joint deformities. Most common joints involved were hand (50%), wrist (50%), and knee (35.7%). The common types of joint deformities were boutonniere deformity (28.6%), ulnar deviation of wrist (28.6%), fixed flexion deformity of wrist (22.9%), and knee (31.4%). -
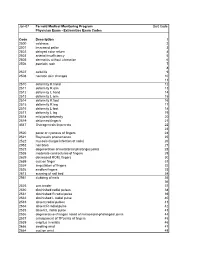
Extremities Exam Codes Code Description 1 2500 Coldness
Jan-07 Fernald Medical Monitoring Program Sort Code Physician Exam - Extremities Exam Codes Code Description 1 2500 coldness 2 2501 increased pallor 3 2502 delayed color return 4 2503 arterial insufficiency 5 2505 dermatitis without ulceration 6 2506 psoriatic rash 7 8 2507 cellulitis 9 2508 necrotic skin changes 10 11 2510 deformity R hand 12 2511 deformity R arm 13 2512 deformity L hand 14 2513 deformity L arm 15 2514 deformity R foot 16 2515 deformity R leg 17 2516 deformity L foot 18 2517 deformity L leg 19 2518 mild joint deformity 20 2519 deformed finger/s 21 4547 Osteogenesis Imperecta 22 23 2520 pallor or cyanosis of fingers 24 2521 Raynaud's phenomenon 25 2522 mycosis (fungal infection of nails) 26 2952 nail bites 27 2523 degeneration of metatarsal phalanges joints 28 2538 moderate contractures of fingers 29 2629 decreased ROM, fingers 30 2659 cyst on finger 31 2524 amputation of fingers 32 2526 swollen fingers 33 2613 scarring of nail bed 34 2951 clubbing of nails 35 36 2525 arm tender 37 2530 diminished radial pulses 38 2531 diminished R radial pulse 39 2532 diminished L radial pulse 40 2533 absent radial pulses 41 2534 absent R radial pulse 42 2535 absent L radial pulse 43 2536 degenerative changes noted of metacarpal-phalangeal joints 44 2537 enlargement of TP joints of fingers 45 2539 crepitus in wrists 46 2666 swelling wrist 47 2664 cyst on wrist 48 Code Description 1 2529 subluxation of interphalangeal joint (IJ) 49 2609 protusion of proximal head of radius 50 51 2540 thenar atrophy 52 2541 carpal tunnel syndrome 53 2542 -

The Ehlers-Danlos Syndromes, Rare Types
American Journal of Medical Genetics Part C (Seminars in Medical Genetics) 175C:70–115 (2017) RESEARCH REVIEW The Ehlers–Danlos Syndromes, Rare Types ANGELA F. BRADY, SERWET DEMIRDAS, SYLVIE FOURNEL-GIGLEUX, NEETI GHALI, CECILIA GIUNTA, INES KAPFERER-SEEBACHER, TOMOKI KOSHO, ROBERTO MENDOZA-LONDONO, MICHAEL F. POPE, MARIANNE ROHRBACH, TIM VAN DAMME, ANTHONY VANDERSTEEN, CAROLINE VAN MOURIK, NICOL VOERMANS, JOHANNES ZSCHOCKE, AND FRANSISKA MALFAIT * Dr. Angela F. Brady, F.R.C.P., Ph.D., is a Consultant Clinical Geneticist at the North West Thames Regional Genetics Service, London and she has a specialist interest in Ehlers–Danlos Syndrome. She was involved in setting up the UK National EDS Diagnostic Service which was established in 2009 and she has been working in the London part of the service since 2015. Dr. Serwet Demirdas, M.D., Ph.D., is a clinical geneticist in training at the Erasmus Medical Center (Erasmus University in Rotterdam, the Netherlands), where she is involved in the clinical service and research into the TNX deficient type of EDS. Prof. Sylvie Fournel-Gigleux, Pharm.D., Ph.D., is a basic researcher in biochemistry/pharmacology, Research Director at INSERM (Institut National de la Sante et de la Recherche Medicale) and co-head of the MolCelTEG Research Team at UMR 7561 CNRS-Universite de Lorraine. Her group is dedicated to the pathobiology of connective tissue disorders, in particular the Ehlers–Danlos syndromes, and specializes on the molecular and structural basis of glycosaminoglycan synthesis enzyme defects. Dr. Neeti Ghali, M.R.C.P.C.H., M.D., is a Consultant Clinical Geneticist at the North West Thames Regional Genetics Service, London and she has a specialist interest in Ehlers–Danlos Syndrome. -

Operative Correction of Swan-Neck and Boutonniere Deformities in the Rheumatoid Hand
Operative Correction of Swan-Neck and Boutonniere Deformities in the Rheumatoid Hand Martin I. Boyer, MD, MSc, FRCSC, and Richard H. Gelberman, MD Abstract A swan-neck or boutonniere deformity occurs in approximately half of patients to evaluate for atlantoaxial subluxa- with rheumatoid arthritis. The cause of boutonniere deformity is chronic syno- tion, basilar impression, and subaxial vitis of the proximal interphalangeal joint. Swan-neck deformity may be caused instability. Previous radiographs, if by synovitis of the metacarpophalangeal, proximal interphalangeal, or distal available, are compared with current interphalangeal joints. Numerous procedures are available for the operative films for signs of progressive instabil- correction of these finger deformities. The choice of surgical procedure is depen- ity. If the tip of the dens cannot be dent on accurate staging of the deformity, which is based on the flexibility of the adequately visualized on plain lateral proximal interphalangeal joint and the state of the articular cartilage. The radiographs of the cervical spine or patientÕs overall medical status and corticosteroid use, the condition of the cer- base of the skull, magnetic resonance vical spine, the need for operative treatment of large joints, and the presence of imaging of the cervical spine is indi- deformities of the wrist and metacarpophalangeal joints must also be considered cated. when planning treatment. In the later stages of both deformities, soft-tissue Regional anesthesia, such as axil- procedures alone may not result in lasting operative correction. lary block, is preferable to general J Am Acad Orthop Surg 1999;7:92-100 anesthesia for correction of finger deformities because postoperative pain control is better and systemic side effects are fewer. -

Monteggia Fracture Galeazzi Fracture
Monteggia Fracture Galeazzi Fracture • Fracture on ulna with radial • Fracture of radial shaft head dislocation with disruption of distal o ORIF in adults radioulnar joint o Non op for children possible o 3x more common than Monteggia o Requires ORIF Metacarpal Fractures o Metacarpal neck • May need to be closed reduced • Acceptable angulation for non op management o < 10 deg for 2nd and 3rd o < 30-40 deg for 4th and 5th (Boxers fracture) • Casting for non op o Ulnar gutter splint/cast for 6 weeks • Surgery o CRPP vs ORIF Boxer’s Fx Metacarpal fractures • Metacarpal shaft fractures o Non op management • if < 10 deg dorsal angulation 2nd and 3rd • If < 20 deg dorsal angulation 4th and 5th o Surgery • Rotational deformity o (causes overlap of fingers) Scaphoid Fractures • Most common carpal fracture • FOOSH injury • Pain in anatomic snuffbox • High potential for slow healing or non union based on location of fracture • non op management o Thumb spica splint/cast 6-24 weeks • Surgical consideration o Any displacement or angulation o Insertion of screw Scaphoid Fractures Common Wrist Problems • Other carpal fractures • Scapholunate o hook of hamate Dissociation • Sprains o “carpal keystone” o FOOSH • DeQuervain’s o Letterman sign tenosynovitis o Positive Finkelstein test o Tx: splint/injection Carpal Tunnel Syndrome • Carpal Tunnel Syndrome o Compression of median nerve in carpal tunnel o Tinel’s sign positive o Thenar muscle wasting o Hand wringing o Non operative • Injection • Wrist splinting o Surgical • Carpal tunnel release Common Hand -

Musculoskeletal Exam
Introduction to the Practice of Medicine Semester III MUSCULOSKELETAL EXAM I. MUSCULOSKELETAL DISEASE A. Magnitude Over 3 7 million people in the United States suffer from one or another form of arthritis or related condition. It represents one of the five leading problems in patients presenting to the primary care physician. B. Rheumatology This is the branch of medicine dealing with arthritis and related disorders of the musculoskeletal system including the multi system autoimmune diseases. Rheumatologists are medical specialists in musculoskeletal disease. C. Value of the History and Physical The history and physical are critical to arriving at an accurate diagnosis of musculoskeletal disorders. Although the same might be said for all systems, it is particularly true in this area. In the diagnosis of musculoskeletal disease, 70% of the weight might be placed on the history, 20% on the physical and 10% on laboratory data. II. TERMS-YOU SHOULD BE FAMILIAR WITH A. Arthralgia: Pain in the joint. B. Arthritis: Inflammation of the joint. Implies presence of warmth, swelling, heat, tenderness and possibly erythema. C. Baker's cyst: A synovial cyst found in the popliteal space, which may occasionally rupture into the calf and mimic thrombophlebitis. D. Bouchard's nodes: Bony enlargement of the proximal interphalangeal joints found in osteoarthritis. E. Boutonniere deformity: A characteristic deformity found in rheumatoid arthritis, which includes a flexion contracture of the proximal phalangeal, joint associated with hyperextension of the distal interphalangeal joint. F. Bursitis: Inflammation of a bursa, which is a synovial lined sac, which may or may not be in communication with a joint cavity. -

This Presentation Is the Intellectual Property of the Author. Contact Them for Permission to Reprint And/Or Distribute
Extensor Mechanism The Stiff Hand: Boutonniere & Swan Neck • Central slip inserts into base of the middle phalanx • Lateral bands lie dorsal to the PIP joint center of rotation Sylvia Dávila, PT, CHT San Antonio, Texas • Lateral bands secured palmarly by the transverse retinacular ligaments & dorsally by the triangular ligament Boutonniere Deformity Extensor Mechanism • Disruption or lengthening of • Central slip inserts into central slip base of the middle • Lateral bands slip volar to phalanx PIP axis of motion & act as • Lateral bands lie dorsal flexors to the PIP joint center of rotation • Lateral bands secured palmarly by the transverse retinacular ligaments & dorsally by the triangular ligament This presentation is the intellectual property of the author. Contact them for permission to reprint and/or distribute. Pathomechanics of Boutonniere Deformity Elson’s Test • Flex PIP to 90 degrees over edge of table • Disruption of central slip • Patient attempts to extend PIP • Lateral bands migrate palmar to axis of • (A) With an intact central slip there is good extensor rotation of PIP due to tone at the PIP & little extensor force at DIP attenuation of triangular ligament • Overpull through the lateral bands due to volar position • Exaggerated extension pull of DIP & flexion of PIP Elson’s Test • (B) With central slip disruption there is decreased extensor force at PIP & prominent extensor tone at DIP • Lateral bands are palmar to axis of rotation This presentation is the intellectual property of the author. Contact them for permission -

A Primer on the Musculoskeletal Examination Technique and Commonly Missed Injuries in Student Health C.S
Division of Student Affairs A Primer on the Musculoskeletal Examination Technique and Commonly Missed Injuries in Student Health C.S. Nasin, MD, CAQ Sports Medicine Medical Director Head Team Physician University of Rhode Island Learning Objectives • Identify commonly missed orthopedic injuries of the upper extremities • Identify commonly missed orthopedic injuries of the lower extremities • Demonstrate proper technique to perform common orthopedic examinations Approach to the MSK exam • History is the most important component of the MSK evaluation – 85% of diagnoses are from the history alone • Know an appropriate DDX for each major joint in the college aged student – DDX of MSK injuries varies with age Bayesian theorem • In probability theory and statistics, Bayes' theorem (alternatively Bayes' law or Bayes' rule) describes the probability of an event, based on prior knowledge of conditions that might be related to the event. Bayesian theorem + MSK exam • Differential Diagnosis – traumatic vs overuse • Was there a recalled injury? • Pre-test probability • Commonly performed MSK exams – Knowledge of what structure each exam is responsible for Caution • Few MSK tests are both highly sensitive and specific. • Most are highly sensitive and poorly specific Approach to the MSK exam • Inspection – Swelling, ecchymosis, deformity • Palpation – Knowledge of anatomy & landmarks • Range of Motion (active vs. passive) – Compare sides, don’t get bogged down with measurements • Special tests – Learn one for each injury/diagnosis Shoulder: Inspection/Palpation