Musculoskeletal Exam
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Soonerstart Automatic Qualifying Syndromes and Conditions 001
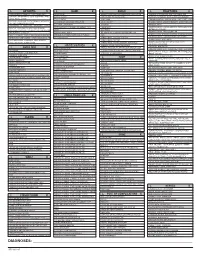
SoonerStart Automatic Qualifying Syndromes and Conditions 001 Abetalipoproteinemia 272.5 002 Acanthocytosis (see Abetalipoproteinemia) 272.5 003 Accutane, Fetal Effects of (see Fetal Retinoid Syndrome) 760.79 004 Acidemia, 2-Oxoglutaric 276.2 005 Acidemia, Glutaric I 277.8 006 Acidemia, Isovaleric 277.8 007 Acidemia, Methylmalonic 277.8 008 Acidemia, Propionic 277.8 009 Aciduria, 3-Methylglutaconic Type II 277.8 010 Aciduria, Argininosuccinic 270.6 011 Acoustic-Cervico-Oculo Syndrome (see Cervico-Oculo-Acoustic Syndrome) 759.89 012 Acrocephalopolysyndactyly Type II 759.89 013 Acrocephalosyndactyly Type I 755.55 014 Acrodysostosis 759.89 015 Acrofacial Dysostosis, Nager Type 756.0 016 Adams-Oliver Syndrome (see Limb and Scalp Defects, Adams-Oliver Type) 759.89 017 Adrenoleukodystrophy, Neonatal (see Cerebro-Hepato-Renal Syndrome) 759.89 018 Aglossia Congenita (see Hypoglossia-Hypodactylia) 759.89 019 Albinism, Ocular (includes Autosomal Recessive Type) 759.89 020 Albinism, Oculocutaneous, Brown Type (Type IV) 759.89 021 Albinism, Oculocutaneous, Tyrosinase Negative (Type IA) 759.89 022 Albinism, Oculocutaneous, Tyrosinase Positive (Type II) 759.89 023 Albinism, Oculocutaneous, Yellow Mutant (Type IB) 759.89 024 Albinism-Black Locks-Deafness 759.89 025 Albright Hereditary Osteodystrophy (see Parathyroid Hormone Resistance) 759.89 026 Alexander Disease 759.89 027 Alopecia - Mental Retardation 759.89 028 Alpers Disease 759.89 029 Alpha 1,4 - Glucosidase Deficiency (see Glycogenosis, Type IIA) 271.0 030 Alpha-L-Fucosidase Deficiency (see Fucosidosis) -
ICD-10 Diagnoses on Router
L ARTHRITIS R L HAND R L ANKLE R L FRACTURES R OSTEOARTHRITIS: PRIMARY, 2°, POST TRAUMA, POST _____ CONTUSION ACHILLES TEN DYSFUNCTION/TENDINITIS/RUPTURE FLXR TEN CLAVICLE: STERNAL END, SHAFT, ACROMIAL END CRYSTALLINE ARTHRITIS: GOUT: IDIOPATHIC, LEAD, CRUSH INJURY AMPUTATION TRAUMATIC LEVEL SCAPULA: ACROMION, BODY, CORACOID, GLENOID DRUG, RENAL, OTHER DUPUYTREN’S CONTUSION PROXIMAL HUMERUS: SURGICAL NECK 2 PART 3 PART 4 PART CRYSTALLINE ARTHRITIS: PSEUDOGOUT: HYDROXY LACERATION: DESCRIBE STRUCTURE CRUSH INJURY PROXIMAL HUMERUS: GREATER TUBEROSITY, LESSER TUBEROSITY DEP DIS, CHONDROCALCINOSIS LIGAMENT DISORDERS EFFUSION HUMERAL SHAFT INFLAMMATORY: RA: SEROPOSITIVE, SERONEGATIVE, JUVENILE OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ LOOSE BODY HUMERUS DISTAL: SUPRACONDYLAR INTERCONDYLAR REACTIVE: SECONDARY TO: INFECTION ELSEWHERE, EXTENSION OR NONE INTESTINAL BYPASS, POST DYSENTERIC, POST IMMUNIZATION PAIN OCD TALUS HUMERUS DISTAL: TRANSCONDYLAR NEUROPATHIC CHARCOT SPRAIN HAND: JOINT? OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ HUMERUS DISTAL: EPICONDYLE LATERAL OR MEDIAL AVULSION INFECT: PYOGENIC: STAPH, STREP, PNEUMO, OTHER BACT TENDON RUPTURES: EXTENSOR OR FLEXOR PAIN HUMERUS DISTAL: CONDYLE MEDIAL OR LATERAL INFECTIOUS: NONPYOGENIC: LYME, GONOCOCCAL, TB TENOSYNOVITIS SPRAIN, ANKLE, CALCANEOFIBULAR ELBOW: RADIUS: HEAD NECK OSTEONECROSIS: IDIOPATHIC, DRUG INDUCED, SPRAIN, ANKLE, DELTOID POST TRAUMATIC, OTHER CAUSE SPRAIN, ANKLE, TIB-FIB LIGAMENT (HIGH ANKLE) ELBOW: OLECRANON WITH OR WITHOUT INTRA ARTICULAR EXTENSION SUBLUXATION OF ANKLE, -

ICD-9CM Coding Achilles Bursitis Or Tendinitis 726.71 Adhesive
ICD-9CM CODING OF COMMON CHIROPRACTIC CONDITIONS CONDITION ICD-9CM coding Achilles bursitis or tendinitis 726.71 Adhesive capsulitis of shoulder 726 Anklyosing Spondylitis (spine only) 720 Anterior cruciate ligament (old disruption) 717.83 Bicipital tenosynovitis 726.12 Boutonniere deformity 736.21 Brachial neuritis or radiculitis 723.4 Bunion 727.1 Bursitis of knee 726.6 Calcaneal spur 726.73 Carpal tunnel syndrome 354 Cervical radiculitis 723.4 Cervical spondylosis with myelopathy 721.1 Cervical spondylosis without myelopathy 721 Cervicalgia 723.1 Chondromalacia of patella 717.7 Claw hand (acquired) 736.06 Claw toe (acquired) 735.5 Coccygodynia 724.79 Coxa plana 732.1 Coxa valga (acquired) 736.31 Coxa vara (acquired) 736.32 de Quervain's disease 727.04 Degeneration of cervical intervertebral disc 722.4 Degeneration of thoracic or lumbar intervertebral disc 722.5 Disc Degeneration (Cervical with myelopathy) 722.71 Disc Degeneration (Lumbar with myelopathy) 722.73 Disc Degeneration (Thoracic) 722.51 Disc Degeneration (Cervical) 722.4 Disc Degeneration (Lumbar) 722.52 Disc Degeneration (Thoracic with myelopathy) 722.72 Disc displacement without myelopathy (Thoracic) 722.11 Disc displacement of without myelopathy (Cervical ) 722 Disc displacement without myelopathy (Lumbar) 722.1 Dupuytren's contracture 728.6 Entrapment syndromes 354.0-355.9 Epicondylitis (Lateral) 726.32 Epicondylitis (Medial) 726.31 Flat foot-Pes planus (acquired) 734 Fracture (Lumbar) 805.4 Ganglion of tendon sheath 727.42 Genu recurvatum (acquired) 736.5 Genu valgum -

A Case Report on Charcot-Marie-Tooth Disease with a Novel Periaxin Gene Mutation
Open Access Case Report DOI: 10.7759/cureus.5111 A Case Report on Charcot-Marie-Tooth Disease with a Novel Periaxin Gene Mutation Sorabh Datta 1 , Saurabh Kataria 1 , Raghav Govindarajan 1 1. Neurology, University of Missouri, Columbia, USA Corresponding author: Sorabh Datta, [email protected] Abstract Charcot-Marie-Tooth (CMT) disease is one of the most common primary hereditary neuropathies causing peripheral neuropathies. More than 60 different gene mutations are causing this disease. The PRX gene codes for Periaxin proteins that are expressed by Schwann cells and are necessary for the formation and maintenance of myelination of peripheral nerves. Dejerine-Sottas neuropathy and Charcot-Marie-Tooth type 4F (CMT4F) are the two different clinical phenotypes observed in association with PRX gene mutation. This article describes a case of an elderly male with a novel mutation involving the PRX gene. Categories: Genetics, Internal Medicine, Neurology Keywords: neurology, sensorimotor neuropathy, congenital, gene expression, genetic mutation, protein, pes cavus, demyelinating diseases, charcot-marie-tooth, autosomal recessive disorder Introduction As per the Dyck classification in the year 1970, primary hereditary neuropathies are divided into hereditary motor sensory neuropathy (HMSN) and hereditary sensory autonomic neuropathy (HSAN) [1]. Charcot- Marie-Tooth (CMT) disease is a type of HMSN with an estimated prevalence of 1 in 2,500 [2]. CMT can follow autosomal recessive (ARCMT), X-linked recessive, and also an autosomal dominant pattern. CMT type 4 is a rapidly increasing ARCMT disease form in HMSN, although CMT type 1 and 2 still account for the most substantial proportion of the patient population [3]. CMT4F is a severe, demyelinating subtype of CMT type 4 and is characterized by childhood onset of slowly progressing weakness in the distal muscles associated with atrophy. -

Upper Extremity
Upper Extremity Shoulder Elbow Wrist/Hand Diagnosis Left Right Diagnosis Left Right Diagnosis Left Right Adhesive capsulitis M75.02 M75.01 Anterior dislocation of radial head S53.015 [7] S53.014 [7] Boutonniere deformity of fingers M20.022 M20.021 Anterior dislocation of humerus S43.015 [7] S43.014 [7] Anterior dislocation of ulnohumeral joint S53.115 [7] S53.114 [7] Carpal Tunnel Syndrome, upper limb G56.02 G56.01 Anterior dislocation of SC joint S43.215 [7] S43.214 [7] Anterior subluxation of radial head S53.012 [7] S53.011 [7] DeQuervain tenosynovitis M65.42 M65.41 Anterior subluxation of humerus S43.012 [7] S43.011 [7] Anterior subluxation of ulnohumeral joint S53.112 [7] S53.111 [7] Dislocation of MCP joint IF S63.261 [7] S63.260 [7] Anterior subluxation of SC joint S43.212 [7] S43.211 [7] Contracture of muscle in forearm M62.432 M62.431 Dislocation of MCP joint of LF S63.267 [7] S63.266 [7] Bicipital tendinitis M75.22 M75.21 Contusion of elbow S50.02X [7] S50.01X [7] Dislocation of MCP joint of MF S63.263 [7] S63.262 [7] Bursitis M75.52 M75.51 Elbow, (recurrent) dislocation M24.422 M24.421 Dislocation of MCP joint of RF S63.265 [7] S63.264 [7] Calcific Tendinitis M75.32 M75.31 Lateral epicondylitis M77.12 M77.11 Dupuytrens M72.0 Contracture of muscle in shoulder M62.412 M62.411 Lesion of ulnar nerve, upper limb G56.22 G56.21 Mallet finger M20.012 M20.011 Contracture of muscle in upper arm M62.422 M62.421 Long head of bicep tendon strain S46.112 [7] S46.111 [7] Osteochondritis dissecans of wrist M93.232 M93.231 Primary, unilateral -

ICD-9 to ICD-10 Mapping Tool Courtesy Of: the Paperwork Project
ICD-9 to ICD-10 Mapping Tool Courtesy of: The Paperwork Project Spinal Subluxation ICD-9 ICD-10 M99.00 Segmental and somatic dysfunction, Head region (occipito-cervical) 739.0 Segmental and somatic dysfunction, Head region (occipito-cervical) M99.10 Subluxation complex (vertebral), Head region M99.01 Segmental and somatic dysfunction, Cervical region 739.1 Segmental and somatic dysfunction, Cervical region M99.11 Subluxation complex (vertebral), Cervical region M99.02 Segmental and somatic dysfunction, Thoracic region 739.2 Segmental and somatic dysfunction, Thoracic region M99.12 Subluxation complex (vertebral), Thoracic region M99.03 Segmental and somatic dysfunction, Lumbar region 739.3 Segmental and somatic dysfunction, Lumbar region M99.13 Subluxation complex (vertebral), Lumbar region M99.04 Segmental and somatic dysfunction, Sacral region 739.4 Segmental and somatic dysfunction, Sacral region M99.14 Subluxation complex (vertebral), Sacral region M99.05 Segmental and somatic dysfunction, Sacroiliac, hip, pubic regions 739.5 Segmental and somatic dysfunction, Sacroiliac, hip, pubic regions M99.15 Subluxation complex (vertebral), Pelvic region 839.08 Closed dislocation, Multiple cervical vertebra (injury) S13.101_ Dislocation of unspecified cervical vertebra (injury) ** 839.20 Closed dislocation, Lumbar vertebra (injury) S33.101_ Dislocation of unspecified lumbar vertebra (injury) ** 839.21 Closed dislocation, Thoracic vertebra (injury) S23.101_ Dislocation of unspecified thoracic vertebra (injury) ** 839.42 Closed dislocation, Sacrum, -

The Nutrition and Food Web Archive Medical Terminology Book
The Nutrition and Food Web Archive Medical Terminology Book www.nafwa. -

Physician Service Fee Schedule-Affordable Care Act(ACA) Taxonomy Defined Rates Pricing Specialty 01E Fee Schedule Updated On: 6/26/2020
NC Medicaid Physician Services Fee Schedule (See Affordable Care Act (ACA) Tab for Applicable ACA Defined Taxonomy Rates) Provider Specialty 001 Fee Schedule Updated on: 6/26/2020 ***The Agency's fee schedule rates below were set as of January 1, 2014 unless otherwise noted*** Rate changes after January 1, 2014 are based on the January 1st RVU of the year in which the service was initally established. The inclusion of a rate on this table does not guarantee that a service is covered. Please refer to the Medicaid Billing Guide and the Medicaid and Health Choice Clinical Policies on the DHB Web Site. Providers should always bill their usual and customary charges. Please use the monthly NC Medicaid Bulletins for additions, changes and deletion to this schedule. Medicaid Maximum Allowable NON-FACILITY Effective FEE END DATE PROCEDURE CODE MODIFIER PROCEDURE DESCRIPTION FACILITY RATE RATE Date of Rate 01967 ANESTH/ANALG VAG DELIVERY $ 220.11 $ 220.11 3/1/2020 12/31/9999 01996 HOSP MANAGE CONT DRUG ADMIN $ 40.88 $ 40.88 3/1/2020 12/31/9999 10004 FNA BX W/O IMG GDN EA ADDL $ 38.83 $ 46.10 3/1/2020 12/31/9999 10005 FNA BX W/US GDN 1ST LES $ 65.75 $ 110.89 3/1/2020 12/31/9999 10006 FNA BX W/US GDN EA ADDL $ 44.80 $ 53.29 3/1/2020 12/31/9999 10007 FNA BX W/FLUOR GDN 1ST LES $ 84.41 $ 247.72 3/1/2020 12/31/9999 10008 FNA BX W/FLUOR GDN EA ADDL $ 55.05 $ 139.88 3/1/2020 12/31/9999 10009 FNA BX W/CT GDN 1ST LES $ 102.46 $ 404.53 3/1/2020 12/31/9999 10010 FNA BX W/CT GDN EA ADDL $ 74.89 $ 244.25 3/1/2020 12/31/9999 10011 FNA BX W/MR GDN 1ST LES $ 54.57 -

Vertical Perspective Medical Assistance Program
Kansas Vertical Perspective Medical Assistance Program December 2006 Provider Bulletin Number 688 General Providers Emergent and Nonemergent Diagnosis Code List Attached is a list of diagnosis codes and whether the Kansas Medical Assistance Program (KMAP) considers the code to be emergent or nonemergent. Providers are responsible for validating whether a particular diagnosis code is covered by KMAP under the beneficiary’s benefit plan and that all program requirements are met. This list does not imply or guarantee payment for listed diagnosis codes. Information about the Kansas Medical Assistance Program as well as provider manuals and other publications are on the KMAP Web site at https://www.kmap-state-ks.us. If you have any questions, please contact the KMAP Customer Service Center at 1-800-933-6593 (in-state providers) or (785) 274-5990 between 7:30 a.m. and 5:30 p.m., Monday through Friday. EDS is the fiscal agent and administrator of the Kansas Medical Assistance Program for the Kansas Health Policy Authority. Page 1 of 347 Emergency Indicators as noted by KMAP: N – Never considered emergent S – Sometimes considered emergent (through supporting medical documentation) Y – Always considered emergent Diagnosis Emergency Diagnosis Code Description Code Indicator 0010 Cholera due to Vibrio Cholerae S 0011 Cholera due to Vibrio Cholerae El Tor S 0019 Unspecified Cholera S 019 Late Effects of Tuberculosis N 0020 Typhoid Fever S 0021 Paratyphoid Fever A S 0022 Paratyphoid Fever B S 0023 Paratyphoid Fever C S 024 Glanders Y 025 Melioidosis -

The Rheumatoid Arthritis Articular Damage Score
20 EXTENDED REPORT Ann Rheum Dis: first published as 10.1136/ard.61.1.20 on 1 January 2002. Downloaded from The rheumatoid arthritis articular damage score: first steps in developing a clinical index of long term damage in RA T R Zijlstra, H J Bernelot Moens,MASBukhari ............................................................................................................................. Ann Rheum Dis 2002;61:20–23 Objective: To design and validate a clinical method for scoring irreversible long term articular dam- age in rheumatoid arthritis (RA). Methods: The rheumatoid arthritis articular damage score (RAAD score) is based on examination of 35 large and small joints. Concise definitions were formulated to score each joint on a three point scale See end of article for (0, no irreversible damage; 1, partially damaged; 2, severe damage, ankylosis, or prosthesis). The authors’ affiliations RAAD score was determined for 121 patients with RA with a large range of disease duration. Inter- ....................... observer agreement was studied in 39 patients scored by three observers. Data on disease duration, Correspondence to: Health Assessment Questionnaire, disease activity score, and Larsen score were collected for 121, 78, Dr T R Zijlstra, Medisch 47, and 45 patients, respectively. Spectrum Twente, Results: The RAAD score correlated well with the Larsen score (r =0.81) and disease duration (r =0.68) Secretariaat Reumatologie, s s Postbus 50000, 7500 KA and (as intended) not with disease activity (rs=0.10). Good interobserver agreement was found for total Enschede, The scores and individual joints. The wide range of RAAD scores for patients with the same disease dura- Netherlands; tion suggested good discriminating power, especially after >10 years. -

Hughston Health Alert US POSTAGE PAID the Hughston Foundation, Inc
HughstonHughston HealthHealth AlertAlert 6262 Veterans Parkway, PO Box 9517, Columbus, GA 31908-9517 • www.hughston.com/hha VOLUME 26, NUMBER 4 - FALL 2014 Fig. 1. Knee Inside... anatomy and • Rotator Cuff Disease ACL injury. Extended (straight) knee • Bunions and Lesser Toe Deformities Femur • Tendon Injuries of the Hand (thighbone) Patella In Perspective: (kneecap) Anterior Cruciate Ligament Tears Medial In 1992, Dr. Jack C. Hughston (1917-2004), one of the meniscus world’s most respected authorities on knee ligament surgery, MCL LCL shared some of his thoughts regarding injuries to the ACL. (medial “You tore your anterior cruciate ligament.” On hearing (lateral collateral collateral your physician speak those words, you are filled with a sense ligament) of dread. You envision the end of your athletic life, even ligament) recreational sports. Today, a torn ACL (Fig. 1) has almost become a household Tibia word. Through friends, newspapers, television, sports Fibula (shinbone) magazines, and even our physicians, we are inundated with the hype that the knee joint will deteriorate and become arthritic if the ACL is not operated on as soon as possible. You have been convinced that to save your knee you must Flexed (bent) knee have an operation immediately to repair the ligament. Your surgery is scheduled for the following day. You are scared. Patella But there is an old truism in orthopaedic surgery that says, (kneecap) “no knee is so bad that it can’t be made worse by operating Articular Torn ACL on it.” cartilage (anterior For many years, torn ACLs were treated as an emergency PCL cruciate and were operated on immediately, even before the initial (posterior ligament) pain and swelling of the injury subsided. -
Orthotic Management of Pt's With
David B. Misener, B.Sc.(H.K.), CPO, MBA ABC Certified Orthotist & Prosthetist CMTa Advisory Board Member Clinical Prosthetics & Orthotics, LLC, Albany, NY CMT 1B Contributors: Ken Cornell, CO, FAAOP Cornell O&P, Peabody, MA S Sean McCale, CO Midwest Orthotic & Technology Center, Chicago, IL Point of view from Orthotist S Description of CMT S Some History S Understand the disease process S Pathophysiology S Pathomechanics S Critical insight into best designs S Patient Evaluation S Orthotic Management Options History 1886 2 papers were submitted Howard Henry Tooth Cambridge Thesis: “The Peroneal type of Jean-Martin Charcot Progressive Muscular Atrophy” 61 y/o 29 y/o Pierre Marie 33 y/o S Other names: Peroneal Muscular Atrophy, HMSN: Hereditary Motor Sensory Neuropathy, Charcot-Marie-Tooth-Hoffman, Tooth’s Motor sensory neuropathy S Description: A progressive inherited neuropathy that is characterized by motor and sensory loss, predominantly in the feet and legs but also in the hands and arms. Proportion of CMT S CMT1 Demyelination S CMT2 Axonal degeneration S Currently there are ~ 80 different kinds of CMT EMG Studies Demyelinating Axonal Degeneration S peripheral neuropathy characterized by: S Chronic denervation on EMG in distal muscles with S Slow nerve conduction velocity typically 5-30 meters per second; S Reduced compound motor action potentials S Normal CV S Normal action potentials S Tibial nerve 47.8 m/s S Tibial nerve 8.8 mV S Peroneal nerve 47.1 m/s S Peroneal nerve 6.0 mV S Hypertrophic peripheral nerves with onion S Near-normal