The Rheumatoid Arthritis Articular Damage Score
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

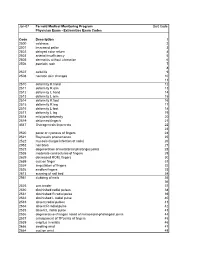
ICD-10 Diagnoses on Router
L ARTHRITIS R L HAND R L ANKLE R L FRACTURES R OSTEOARTHRITIS: PRIMARY, 2°, POST TRAUMA, POST _____ CONTUSION ACHILLES TEN DYSFUNCTION/TENDINITIS/RUPTURE FLXR TEN CLAVICLE: STERNAL END, SHAFT, ACROMIAL END CRYSTALLINE ARTHRITIS: GOUT: IDIOPATHIC, LEAD, CRUSH INJURY AMPUTATION TRAUMATIC LEVEL SCAPULA: ACROMION, BODY, CORACOID, GLENOID DRUG, RENAL, OTHER DUPUYTREN’S CONTUSION PROXIMAL HUMERUS: SURGICAL NECK 2 PART 3 PART 4 PART CRYSTALLINE ARTHRITIS: PSEUDOGOUT: HYDROXY LACERATION: DESCRIBE STRUCTURE CRUSH INJURY PROXIMAL HUMERUS: GREATER TUBEROSITY, LESSER TUBEROSITY DEP DIS, CHONDROCALCINOSIS LIGAMENT DISORDERS EFFUSION HUMERAL SHAFT INFLAMMATORY: RA: SEROPOSITIVE, SERONEGATIVE, JUVENILE OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ LOOSE BODY HUMERUS DISTAL: SUPRACONDYLAR INTERCONDYLAR REACTIVE: SECONDARY TO: INFECTION ELSEWHERE, EXTENSION OR NONE INTESTINAL BYPASS, POST DYSENTERIC, POST IMMUNIZATION PAIN OCD TALUS HUMERUS DISTAL: TRANSCONDYLAR NEUROPATHIC CHARCOT SPRAIN HAND: JOINT? OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ HUMERUS DISTAL: EPICONDYLE LATERAL OR MEDIAL AVULSION INFECT: PYOGENIC: STAPH, STREP, PNEUMO, OTHER BACT TENDON RUPTURES: EXTENSOR OR FLEXOR PAIN HUMERUS DISTAL: CONDYLE MEDIAL OR LATERAL INFECTIOUS: NONPYOGENIC: LYME, GONOCOCCAL, TB TENOSYNOVITIS SPRAIN, ANKLE, CALCANEOFIBULAR ELBOW: RADIUS: HEAD NECK OSTEONECROSIS: IDIOPATHIC, DRUG INDUCED, SPRAIN, ANKLE, DELTOID POST TRAUMATIC, OTHER CAUSE SPRAIN, ANKLE, TIB-FIB LIGAMENT (HIGH ANKLE) ELBOW: OLECRANON WITH OR WITHOUT INTRA ARTICULAR EXTENSION SUBLUXATION OF ANKLE, -

Upper Extremity
Upper Extremity Shoulder Elbow Wrist/Hand Diagnosis Left Right Diagnosis Left Right Diagnosis Left Right Adhesive capsulitis M75.02 M75.01 Anterior dislocation of radial head S53.015 [7] S53.014 [7] Boutonniere deformity of fingers M20.022 M20.021 Anterior dislocation of humerus S43.015 [7] S43.014 [7] Anterior dislocation of ulnohumeral joint S53.115 [7] S53.114 [7] Carpal Tunnel Syndrome, upper limb G56.02 G56.01 Anterior dislocation of SC joint S43.215 [7] S43.214 [7] Anterior subluxation of radial head S53.012 [7] S53.011 [7] DeQuervain tenosynovitis M65.42 M65.41 Anterior subluxation of humerus S43.012 [7] S43.011 [7] Anterior subluxation of ulnohumeral joint S53.112 [7] S53.111 [7] Dislocation of MCP joint IF S63.261 [7] S63.260 [7] Anterior subluxation of SC joint S43.212 [7] S43.211 [7] Contracture of muscle in forearm M62.432 M62.431 Dislocation of MCP joint of LF S63.267 [7] S63.266 [7] Bicipital tendinitis M75.22 M75.21 Contusion of elbow S50.02X [7] S50.01X [7] Dislocation of MCP joint of MF S63.263 [7] S63.262 [7] Bursitis M75.52 M75.51 Elbow, (recurrent) dislocation M24.422 M24.421 Dislocation of MCP joint of RF S63.265 [7] S63.264 [7] Calcific Tendinitis M75.32 M75.31 Lateral epicondylitis M77.12 M77.11 Dupuytrens M72.0 Contracture of muscle in shoulder M62.412 M62.411 Lesion of ulnar nerve, upper limb G56.22 G56.21 Mallet finger M20.012 M20.011 Contracture of muscle in upper arm M62.422 M62.421 Long head of bicep tendon strain S46.112 [7] S46.111 [7] Osteochondritis dissecans of wrist M93.232 M93.231 Primary, unilateral -

Vertical Perspective Medical Assistance Program
Kansas Vertical Perspective Medical Assistance Program December 2006 Provider Bulletin Number 688 General Providers Emergent and Nonemergent Diagnosis Code List Attached is a list of diagnosis codes and whether the Kansas Medical Assistance Program (KMAP) considers the code to be emergent or nonemergent. Providers are responsible for validating whether a particular diagnosis code is covered by KMAP under the beneficiary’s benefit plan and that all program requirements are met. This list does not imply or guarantee payment for listed diagnosis codes. Information about the Kansas Medical Assistance Program as well as provider manuals and other publications are on the KMAP Web site at https://www.kmap-state-ks.us. If you have any questions, please contact the KMAP Customer Service Center at 1-800-933-6593 (in-state providers) or (785) 274-5990 between 7:30 a.m. and 5:30 p.m., Monday through Friday. EDS is the fiscal agent and administrator of the Kansas Medical Assistance Program for the Kansas Health Policy Authority. Page 1 of 347 Emergency Indicators as noted by KMAP: N – Never considered emergent S – Sometimes considered emergent (through supporting medical documentation) Y – Always considered emergent Diagnosis Emergency Diagnosis Code Description Code Indicator 0010 Cholera due to Vibrio Cholerae S 0011 Cholera due to Vibrio Cholerae El Tor S 0019 Unspecified Cholera S 019 Late Effects of Tuberculosis N 0020 Typhoid Fever S 0021 Paratyphoid Fever A S 0022 Paratyphoid Fever B S 0023 Paratyphoid Fever C S 024 Glanders Y 025 Melioidosis -

Hughston Health Alert US POSTAGE PAID the Hughston Foundation, Inc
HughstonHughston HealthHealth AlertAlert 6262 Veterans Parkway, PO Box 9517, Columbus, GA 31908-9517 • www.hughston.com/hha VOLUME 26, NUMBER 4 - FALL 2014 Fig. 1. Knee Inside... anatomy and • Rotator Cuff Disease ACL injury. Extended (straight) knee • Bunions and Lesser Toe Deformities Femur • Tendon Injuries of the Hand (thighbone) Patella In Perspective: (kneecap) Anterior Cruciate Ligament Tears Medial In 1992, Dr. Jack C. Hughston (1917-2004), one of the meniscus world’s most respected authorities on knee ligament surgery, MCL LCL shared some of his thoughts regarding injuries to the ACL. (medial “You tore your anterior cruciate ligament.” On hearing (lateral collateral collateral your physician speak those words, you are filled with a sense ligament) of dread. You envision the end of your athletic life, even ligament) recreational sports. Today, a torn ACL (Fig. 1) has almost become a household Tibia word. Through friends, newspapers, television, sports Fibula (shinbone) magazines, and even our physicians, we are inundated with the hype that the knee joint will deteriorate and become arthritic if the ACL is not operated on as soon as possible. You have been convinced that to save your knee you must Flexed (bent) knee have an operation immediately to repair the ligament. Your surgery is scheduled for the following day. You are scared. Patella But there is an old truism in orthopaedic surgery that says, (kneecap) “no knee is so bad that it can’t be made worse by operating Articular Torn ACL on it.” cartilage (anterior For many years, torn ACLs were treated as an emergency PCL cruciate and were operated on immediately, even before the initial (posterior ligament) pain and swelling of the injury subsided. -

Mcmaster Musculoskeletal Clinical Skills Manual 1E
McMaster Musculoskeletal Clinical Skills Manual Authors Samyuktha Adiga Dr. Raj Carmona, MBBS, FRCPC Illustrator Jenna Rebelo Editors Caitlin Lees Dr. Raj Carmona, MBBS, FRCPC In association with the Medical Education Interest Group Narendra Singh and Jacqueline Ho (co-chairs) FOREWORD AND ACKNOWLEDGEMENTS The McMaster Musculoskeletal Clinical Skills Manual was produced by members of the Medical Education Interest Group (co-chairs Jacqueline Ho and Narendra Singh), and Dr. Raj Carmona, Assistant Professor of Medicine at McMaster University. Samyuktha Adiga and Dr. Carmona wrote the manual. Illustrations were done by Jenna Rebelo. Editing was performed by Caitlin Lees and Dr. Carmona. The Manual, completed in August 2012, is a supplement to the McMaster MSK Examination Video Series created by Dr. Carmona, and closely follows the format and content of these videos. The videos are available on Medportal (McMaster students), and also publicly accessible at RheumTutor.com and fhs.mcmaster.ca/medicine/rheumatology. McMaster Musculoskeletal Clinical Skills Manual S. Adiga, J. Rebelo, C. Lees, R. Carmona McMaster Musculoskeletal Clinical Skills Manual TABLE OF CONTENTS General Guide 1 Hip Examination 3 Knee Examination 6 Ankle and Foot Examination 12 Examination of the Back 15 Shoulder Examination 19 Elbow Examination 24 Hand and Wrist Examination 26 Appendix: Neurological Assessment 29 1 GENERAL GUIDE (Please see videos for detailed demonstration of examinations) Always wash your hands and then introduce yourself to the patient. As with any other exam, ensure adequate exposure while respecting patient's modesty. Remember to assess gait whenever doing an examination of the back or any part of the lower limbs. Inspection follows the format: ● S welling ● E rythema ● A trophy ● D eformities ● S cars, skin changes, etc. -
Degenerative Joint Disorders
[Color index : Important | Notes | Extra] Editing file link Degenerative Joint Disorders Objectives: ★ not given Done by: Norah AlAkeel Edited By: Bedoor Julaidan Revised by: Dalal Alhuzaimi References: 435 Lectures And Notes /Apley / 433 Team Background Articular cartilage ★ It is avascular and aneural hyaline cartilage ★ Viscoelastic material with variable load - bearing properties ★ Decreases joint friction. Cartilage composition: 1-Water (60% to 80% wet weight) most important part - pumped in and out of cartilage depending on load - contributes to lubrication and Nutrition 2-Collagen (10% to 20% wet weight) - secreted by chondrocytes - mostly type 2 collagen (90%) ﻗﻮة اﻟﺸﺪ - confers tensile strength to cartilage - 3-Proteoglycans (10% to 15% wet weight) - secreted by chondrocytes - composed of GAG1 (aggrecan , chondroitin ,and keratin sulfate) - negatively charged proteins holds water within matrix - provides compressive strength 4-Chondrocytes (5% wet weight) - only cell type in cartilage ★ Chondrocytes have little capacity for cell division in vivo and in vitro so when there is a direct damage to the articular surface, cartilage is poorly repaired, or repaired only with (poor cartilage) fibrocartilage which has inferior biomechanical properties than hyaline cartilage ★ If the collagen network is disrupted, initially the matrix becomes waterlogged and soft .later on it will be eroded, hard and underlying bone will be exposed ★ There will be loss of proteoglycans, cellular damage and splitting (‘fibrillation’ initially ) of articular cartilage. then later on complete loss of articular cartilage, In X ray we see it as a reduction in joint space initially then there is no joint space and it’s bone on bone ★ Damaged chondrocytes begin to release matrix-degrading enzymes inside the joint cause further damage. -

Boutonnière Deformity of the Finger
CLINICAL Boutonnière Deformity of the Finger REVIEW Indexing Metadata/Description › Title/condition: Boutonnière Deformity of the Finger › Synonyms: Finger deformity, boutonnière; buttonhole deformity; central slip injury; deformity of the finger, boutonnière; finger deformity, boutonnière › Anatomical location/body part affected: Any of the fingers on either hand might be affected. In the thumb, boutonnière deformity (BD) occurs at the metacarpophalangeal (MCP) joint, whereas in the remaining fingers BD occurs at the proximal interphalangeal (PIP) joint › Area(s) of specialty: Hand Therapy, Orthopedic Rehabilitation › Description: A rupture of the central slip causing a deformity characterized by flexion of the PIP joint and extension or hyperextension of the distal interphalangeal (DIP) joint. In some cases, MCP joint extension might also be present. This is usually a result of trauma or secondary to inflammatory arthritis (e.g., rheumatoid arthritis [RA]) › ICD-10 codes • M20.021 boutonnière deformity of right finger(s) • M20.022 boutonnière deformity of left finger(s) • M20.029 boutonnière deformity of unspecified finger(s) (ICD codes are provided for the reader’s reference, not for billing purposes) › Reimbursement: No specific issues or information regarding reimbursement has been identified › Presentation/signs and symptoms • The classic presentation is PIP joint flexion with DIP joint hyperextension. There is damage to the central slip that limits the extensor function of the affected digit(1) Causes, Pathogenesis, & Risk Factors -

Spectrum of Joint Deformities in Children with Juvenile Idiopathic Arthritis Samia Naz1, Misbah Asif2, Farrah Naz1, Hina Farooq3 and Muhammad Haroon Hamid1
CLINICAL PRACTICE ARTICLE Spectrum of Joint Deformities in Children with Juvenile Idiopathic Arthritis Samia Naz1, Misbah Asif2, Farrah Naz1, Hina Farooq3 and Muhammad Haroon Hamid1 ABSTRACT Objective: To determine the frequency and types of joint deformities in children with juvenile idiopathic arthritis and their association with clinical parameters and rheumatoid factor. Study Design: Cross-sectional study. Place and Duration of Study: Rheumatology Outpatient Clinic, the Children's Hospital and the Institute of Child Health, Lahore, from September 2014 to February 2015. Methodology: All patients of both genders of less than 16 years of age, who fulfilled the International League of Association for Rheumatology (ILAR) criteria for Juvenile Idiopathic Arthritis (JIA), were enrolled in this study. Their demographic data, duration of disease at the time of presentation, types of JIA, various joint deformities and rheumatoid factor (RF) were documented. Statistical analysis of data was done on SPSS version 16. Chi-square test was applied to determine the association of clinical deformity with age of patients, disease duration at presentation, types of JIA and RF. Results: Out of 70 patients enrolled during the study period, 51.4% were boys with mean age at presentation being 9.44 ±3.89 years (2-7 years) and median duration of disease being 24 months (interquartile range 42 months). Forty patients (57.1%) had joint deformities. Most common joints involved were hand (50%), wrist (50%), and knee (35.7%). The common types of joint deformities were boutonniere deformity (28.6%), ulnar deviation of wrist (28.6%), fixed flexion deformity of wrist (22.9%), and knee (31.4%). -

Joint-Preserving Surgery for Hyperextension Deformity of the Hallux Interphalangeal Joint in a Patient with Rheumatoid Arthritis
Hindawi Case Reports in Orthopedics Volume 2020, Article ID 5843095, 6 pages https://doi.org/10.1155/2020/5843095 Case Report Joint-Preserving Surgery for Hyperextension Deformity of the Hallux Interphalangeal Joint in a Patient with Rheumatoid Arthritis Takumi Matsumoto , Yuki Shimizu, Song Ho Chang, Taro Kasai, Jun Hirose, and Sakae Tanaka Department of Orthopaedic Surgery, Faculty of Medicine, The University of Tokyo, 7-3-1 Hongo, Bunkyo-ku, Tokyo 113-8655, Japan Correspondence should be addressed to Takumi Matsumoto; [email protected] Received 12 March 2020; Revised 31 May 2020; Accepted 29 June 2020; Published 8 July 2020 Academic Editor: George Mouzopoulos Copyright © 2020 Takumi Matsumoto et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Interphalangeal hyperextension is one of the major hallux deformities in patients with rheumatoid arthritis; however, there is yet no established surgical method for this deformity. We here present the case of a 69-year-old female patient with rheumatoid arthritis who developed hallux interphalangeal hyperextension and painful callosity on the plantar hallux accompanied by limited dorsiflexion at the metatarsophalangeal joint. Lateral weight-bearing radiograph of the foot revealed misalignment of the medial column and hallux, including a collapsed medial arch, elevated first metatarsal, plantar flexion and deviation of the proximal phalanx, and hyperextension of the distal phalanx. The foot was successfully treated and became symptom-free with opening wedge osteotomy of the medial cuneiform, plantar and proximal translation of the metatarsal head, and tenotomy of the extensor hallucis longus. -

Rotator Cuff Tendinitis Shoulder Joint Replacement Mallet Finger Low
We would like to thank you for choosing Campbell Clinic to care for you or your family member during this time. We believe that one of the best ways to ensure quality care and minimize reoccurrences is through educating our patients on their injuries or diseases. Based on the information obtained from today's visit and the course of treatment your physician has discussed with you, the following educational materials are recommended for additional information: Shoulder, Arm, & Elbow Hand & Wrist Spine & Neck Fractures Tears & Injuries Fractures Diseases & Syndromes Fractures & Other Injuries Diseases & Syndromes Adult Forearm Biceps Tear Distal Radius Carpal Tunnel Syndrome Cervical Fracture Chordoma Children Forearm Rotator Cuff Tear Finger Compartment Syndrome Thoracic & Lumbar Spine Lumbar Spine Stenosis Clavicle Shoulder Joint Tear Hand Arthritis of Hand Osteoporosis & Spinal Fx Congenital Scoliosis Distal Humerus Burners & Stingers Scaphoid Fx of Wrist Dupuytren's Comtracture Spondylolysis Congenital Torticollis Shoulder Blade Elbow Dislocation Thumb Arthritis of Wrist Spondylolisthesis Kyphosis of the Spine Adult Elbow Erb's Palsy Sprains, Strains & Other Injuries Kienböck's Disease Lumbar Disk Herniation Scoliosis Children Elbow Shoulder Dislocation Sprained Thumb Ganglion Cyst of the Wrist Neck Sprain Scoliosis in Children Diseases & Syndromes Surgical Treatments Wrist Sprains Arthritis of Thumb Herniated Disk Pack Pain in Children Compartment Syndrome Total Shoulder Replacement Fingertip Injuries Boutonnière Deformity Treatment -
Extremities Exam Codes Code Description 1 2500 Coldness
Jan-07 Fernald Medical Monitoring Program Sort Code Physician Exam - Extremities Exam Codes Code Description 1 2500 coldness 2 2501 increased pallor 3 2502 delayed color return 4 2503 arterial insufficiency 5 2505 dermatitis without ulceration 6 2506 psoriatic rash 7 8 2507 cellulitis 9 2508 necrotic skin changes 10 11 2510 deformity R hand 12 2511 deformity R arm 13 2512 deformity L hand 14 2513 deformity L arm 15 2514 deformity R foot 16 2515 deformity R leg 17 2516 deformity L foot 18 2517 deformity L leg 19 2518 mild joint deformity 20 2519 deformed finger/s 21 4547 Osteogenesis Imperecta 22 23 2520 pallor or cyanosis of fingers 24 2521 Raynaud's phenomenon 25 2522 mycosis (fungal infection of nails) 26 2952 nail bites 27 2523 degeneration of metatarsal phalanges joints 28 2538 moderate contractures of fingers 29 2629 decreased ROM, fingers 30 2659 cyst on finger 31 2524 amputation of fingers 32 2526 swollen fingers 33 2613 scarring of nail bed 34 2951 clubbing of nails 35 36 2525 arm tender 37 2530 diminished radial pulses 38 2531 diminished R radial pulse 39 2532 diminished L radial pulse 40 2533 absent radial pulses 41 2534 absent R radial pulse 42 2535 absent L radial pulse 43 2536 degenerative changes noted of metacarpal-phalangeal joints 44 2537 enlargement of TP joints of fingers 45 2539 crepitus in wrists 46 2666 swelling wrist 47 2664 cyst on wrist 48 Code Description 1 2529 subluxation of interphalangeal joint (IJ) 49 2609 protusion of proximal head of radius 50 51 2540 thenar atrophy 52 2541 carpal tunnel syndrome 53 2542 -

How Do I Wear the Oval-8? Wear an Oval-8 Finger Splint on the End of Your Finger to Hold It Straight While Still Allowing the Middle Joint to Bend
OVAL-8® FINGER SPLINT GUIDE 7 Ways for 7 Conditions A Publication of Oh My Arthritis © 2016 Oval-8 is a registered Trademark of 3-Point Products, Inc. 7 CONDITIONS Mallet or Baseball Finger Swan Neck Deformity Boutonniere Deformity Trigger Finger and Trigger Thumb Hypermobility (EDS) Crooked Fingers Jammed or Broken Fingers A Publication of Oh My Arthritis © 2016 MALLET OR BASEBALL FINGER Mallet Finger is a very common injury that can happen when catching a ball, hitting your finger against something hard or catching your finger in a drawer. Also called “baseball finger”, it is when the end of your finger droops in a bent position and won’t straighten by itself. You can push your finger into a straight position but it won’t stay straight without support. How Do I Wear the Oval-8? Wear an Oval-8 Finger Splint on the end of your finger to hold it straight while still allowing the middle joint to bend. The band is worn on top of the finger joint closest to your fingernail and the oval portion on the palm or inside to hold your finger straight. A Publication of Oh My Arthritis © 2016 SWAN NECK DEFORMITY The most common causes of a Swan Neck deformity are Rheumatoid Arthritis (RA), a ligament injury or an untreated Mallet or “Baseball” finger. A Swan Neck deformity is a condition where the middle joint of your finger hyperextends or bends backwards and the end joint, near the fingernail, flexes or bends downwards. How Do I Wear the Oval-8? Wear an Oval-8 Finger Splint to block the hyperextension at the middle joint of your finger while still allowing your finger to bend for full hand movement.