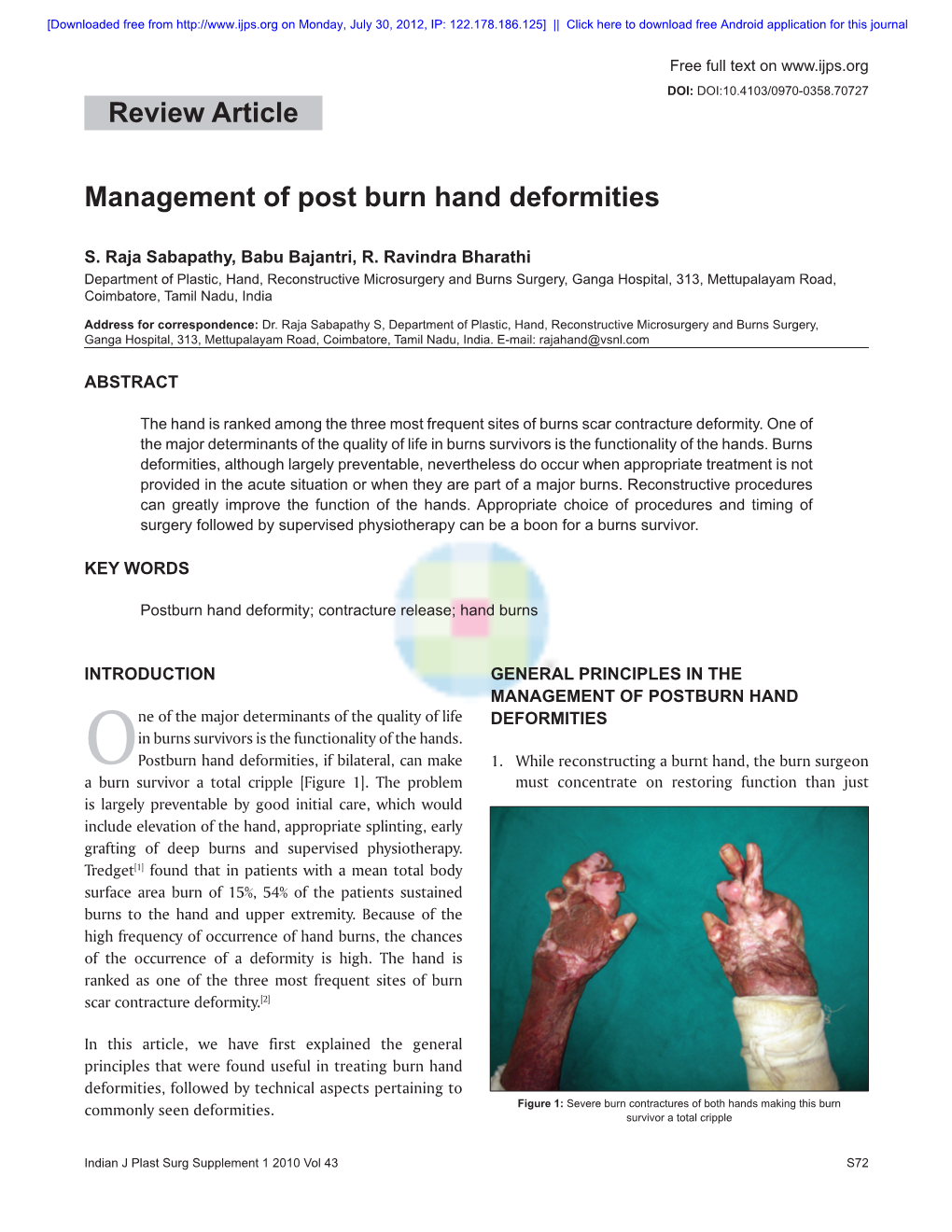
Management of Post Burn Hand Deformities Review Article
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Soonerstart Automatic Qualifying Syndromes and Conditions 001
SoonerStart Automatic Qualifying Syndromes and Conditions 001 Abetalipoproteinemia 272.5 002 Acanthocytosis (see Abetalipoproteinemia) 272.5 003 Accutane, Fetal Effects of (see Fetal Retinoid Syndrome) 760.79 004 Acidemia, 2-Oxoglutaric 276.2 005 Acidemia, Glutaric I 277.8 006 Acidemia, Isovaleric 277.8 007 Acidemia, Methylmalonic 277.8 008 Acidemia, Propionic 277.8 009 Aciduria, 3-Methylglutaconic Type II 277.8 010 Aciduria, Argininosuccinic 270.6 011 Acoustic-Cervico-Oculo Syndrome (see Cervico-Oculo-Acoustic Syndrome) 759.89 012 Acrocephalopolysyndactyly Type II 759.89 013 Acrocephalosyndactyly Type I 755.55 014 Acrodysostosis 759.89 015 Acrofacial Dysostosis, Nager Type 756.0 016 Adams-Oliver Syndrome (see Limb and Scalp Defects, Adams-Oliver Type) 759.89 017 Adrenoleukodystrophy, Neonatal (see Cerebro-Hepato-Renal Syndrome) 759.89 018 Aglossia Congenita (see Hypoglossia-Hypodactylia) 759.89 019 Albinism, Ocular (includes Autosomal Recessive Type) 759.89 020 Albinism, Oculocutaneous, Brown Type (Type IV) 759.89 021 Albinism, Oculocutaneous, Tyrosinase Negative (Type IA) 759.89 022 Albinism, Oculocutaneous, Tyrosinase Positive (Type II) 759.89 023 Albinism, Oculocutaneous, Yellow Mutant (Type IB) 759.89 024 Albinism-Black Locks-Deafness 759.89 025 Albright Hereditary Osteodystrophy (see Parathyroid Hormone Resistance) 759.89 026 Alexander Disease 759.89 027 Alopecia - Mental Retardation 759.89 028 Alpers Disease 759.89 029 Alpha 1,4 - Glucosidase Deficiency (see Glycogenosis, Type IIA) 271.0 030 Alpha-L-Fucosidase Deficiency (see Fucosidosis) -

ICD-10 Diagnoses on Router
L ARTHRITIS R L HAND R L ANKLE R L FRACTURES R OSTEOARTHRITIS: PRIMARY, 2°, POST TRAUMA, POST _____ CONTUSION ACHILLES TEN DYSFUNCTION/TENDINITIS/RUPTURE FLXR TEN CLAVICLE: STERNAL END, SHAFT, ACROMIAL END CRYSTALLINE ARTHRITIS: GOUT: IDIOPATHIC, LEAD, CRUSH INJURY AMPUTATION TRAUMATIC LEVEL SCAPULA: ACROMION, BODY, CORACOID, GLENOID DRUG, RENAL, OTHER DUPUYTREN’S CONTUSION PROXIMAL HUMERUS: SURGICAL NECK 2 PART 3 PART 4 PART CRYSTALLINE ARTHRITIS: PSEUDOGOUT: HYDROXY LACERATION: DESCRIBE STRUCTURE CRUSH INJURY PROXIMAL HUMERUS: GREATER TUBEROSITY, LESSER TUBEROSITY DEP DIS, CHONDROCALCINOSIS LIGAMENT DISORDERS EFFUSION HUMERAL SHAFT INFLAMMATORY: RA: SEROPOSITIVE, SERONEGATIVE, JUVENILE OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ LOOSE BODY HUMERUS DISTAL: SUPRACONDYLAR INTERCONDYLAR REACTIVE: SECONDARY TO: INFECTION ELSEWHERE, EXTENSION OR NONE INTESTINAL BYPASS, POST DYSENTERIC, POST IMMUNIZATION PAIN OCD TALUS HUMERUS DISTAL: TRANSCONDYLAR NEUROPATHIC CHARCOT SPRAIN HAND: JOINT? OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ HUMERUS DISTAL: EPICONDYLE LATERAL OR MEDIAL AVULSION INFECT: PYOGENIC: STAPH, STREP, PNEUMO, OTHER BACT TENDON RUPTURES: EXTENSOR OR FLEXOR PAIN HUMERUS DISTAL: CONDYLE MEDIAL OR LATERAL INFECTIOUS: NONPYOGENIC: LYME, GONOCOCCAL, TB TENOSYNOVITIS SPRAIN, ANKLE, CALCANEOFIBULAR ELBOW: RADIUS: HEAD NECK OSTEONECROSIS: IDIOPATHIC, DRUG INDUCED, SPRAIN, ANKLE, DELTOID POST TRAUMATIC, OTHER CAUSE SPRAIN, ANKLE, TIB-FIB LIGAMENT (HIGH ANKLE) ELBOW: OLECRANON WITH OR WITHOUT INTRA ARTICULAR EXTENSION SUBLUXATION OF ANKLE, -

Upper Extremity
Upper Extremity Shoulder Elbow Wrist/Hand Diagnosis Left Right Diagnosis Left Right Diagnosis Left Right Adhesive capsulitis M75.02 M75.01 Anterior dislocation of radial head S53.015 [7] S53.014 [7] Boutonniere deformity of fingers M20.022 M20.021 Anterior dislocation of humerus S43.015 [7] S43.014 [7] Anterior dislocation of ulnohumeral joint S53.115 [7] S53.114 [7] Carpal Tunnel Syndrome, upper limb G56.02 G56.01 Anterior dislocation of SC joint S43.215 [7] S43.214 [7] Anterior subluxation of radial head S53.012 [7] S53.011 [7] DeQuervain tenosynovitis M65.42 M65.41 Anterior subluxation of humerus S43.012 [7] S43.011 [7] Anterior subluxation of ulnohumeral joint S53.112 [7] S53.111 [7] Dislocation of MCP joint IF S63.261 [7] S63.260 [7] Anterior subluxation of SC joint S43.212 [7] S43.211 [7] Contracture of muscle in forearm M62.432 M62.431 Dislocation of MCP joint of LF S63.267 [7] S63.266 [7] Bicipital tendinitis M75.22 M75.21 Contusion of elbow S50.02X [7] S50.01X [7] Dislocation of MCP joint of MF S63.263 [7] S63.262 [7] Bursitis M75.52 M75.51 Elbow, (recurrent) dislocation M24.422 M24.421 Dislocation of MCP joint of RF S63.265 [7] S63.264 [7] Calcific Tendinitis M75.32 M75.31 Lateral epicondylitis M77.12 M77.11 Dupuytrens M72.0 Contracture of muscle in shoulder M62.412 M62.411 Lesion of ulnar nerve, upper limb G56.22 G56.21 Mallet finger M20.012 M20.011 Contracture of muscle in upper arm M62.422 M62.421 Long head of bicep tendon strain S46.112 [7] S46.111 [7] Osteochondritis dissecans of wrist M93.232 M93.231 Primary, unilateral -

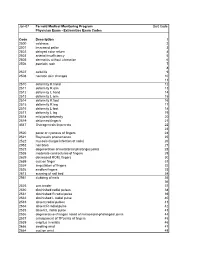
Physician Service Fee Schedule-Affordable Care Act(ACA) Taxonomy Defined Rates Pricing Specialty 01E Fee Schedule Updated On: 6/26/2020
NC Medicaid Physician Services Fee Schedule (See Affordable Care Act (ACA) Tab for Applicable ACA Defined Taxonomy Rates) Provider Specialty 001 Fee Schedule Updated on: 6/26/2020 ***The Agency's fee schedule rates below were set as of January 1, 2014 unless otherwise noted*** Rate changes after January 1, 2014 are based on the January 1st RVU of the year in which the service was initally established. The inclusion of a rate on this table does not guarantee that a service is covered. Please refer to the Medicaid Billing Guide and the Medicaid and Health Choice Clinical Policies on the DHB Web Site. Providers should always bill their usual and customary charges. Please use the monthly NC Medicaid Bulletins for additions, changes and deletion to this schedule. Medicaid Maximum Allowable NON-FACILITY Effective FEE END DATE PROCEDURE CODE MODIFIER PROCEDURE DESCRIPTION FACILITY RATE RATE Date of Rate 01967 ANESTH/ANALG VAG DELIVERY $ 220.11 $ 220.11 3/1/2020 12/31/9999 01996 HOSP MANAGE CONT DRUG ADMIN $ 40.88 $ 40.88 3/1/2020 12/31/9999 10004 FNA BX W/O IMG GDN EA ADDL $ 38.83 $ 46.10 3/1/2020 12/31/9999 10005 FNA BX W/US GDN 1ST LES $ 65.75 $ 110.89 3/1/2020 12/31/9999 10006 FNA BX W/US GDN EA ADDL $ 44.80 $ 53.29 3/1/2020 12/31/9999 10007 FNA BX W/FLUOR GDN 1ST LES $ 84.41 $ 247.72 3/1/2020 12/31/9999 10008 FNA BX W/FLUOR GDN EA ADDL $ 55.05 $ 139.88 3/1/2020 12/31/9999 10009 FNA BX W/CT GDN 1ST LES $ 102.46 $ 404.53 3/1/2020 12/31/9999 10010 FNA BX W/CT GDN EA ADDL $ 74.89 $ 244.25 3/1/2020 12/31/9999 10011 FNA BX W/MR GDN 1ST LES $ 54.57 -
Orthotic Management of Pt's With
David B. Misener, B.Sc.(H.K.), CPO, MBA ABC Certified Orthotist & Prosthetist CMTa Advisory Board Member Clinical Prosthetics & Orthotics, LLC, Albany, NY CMT 1B Contributors: Ken Cornell, CO, FAAOP Cornell O&P, Peabody, MA S Sean McCale, CO Midwest Orthotic & Technology Center, Chicago, IL Point of view from Orthotist S Description of CMT S Some History S Understand the disease process S Pathophysiology S Pathomechanics S Critical insight into best designs S Patient Evaluation S Orthotic Management Options History 1886 2 papers were submitted Howard Henry Tooth Cambridge Thesis: “The Peroneal type of Jean-Martin Charcot Progressive Muscular Atrophy” 61 y/o 29 y/o Pierre Marie 33 y/o S Other names: Peroneal Muscular Atrophy, HMSN: Hereditary Motor Sensory Neuropathy, Charcot-Marie-Tooth-Hoffman, Tooth’s Motor sensory neuropathy S Description: A progressive inherited neuropathy that is characterized by motor and sensory loss, predominantly in the feet and legs but also in the hands and arms. Proportion of CMT S CMT1 Demyelination S CMT2 Axonal degeneration S Currently there are ~ 80 different kinds of CMT EMG Studies Demyelinating Axonal Degeneration S peripheral neuropathy characterized by: S Chronic denervation on EMG in distal muscles with S Slow nerve conduction velocity typically 5-30 meters per second; S Reduced compound motor action potentials S Normal CV S Normal action potentials S Tibial nerve 47.8 m/s S Tibial nerve 8.8 mV S Peroneal nerve 47.1 m/s S Peroneal nerve 6.0 mV S Hypertrophic peripheral nerves with onion S Near-normal -

On the Inheritance of Hand and Foot Anomalies in Six Families
On the Inheritance of Hand and Foot Anomalies in Six Families OLA JOHNSTON AND RALPH WALDO DAVIS Department of Biology, North Texas State College, Denton, Texas INTRODUCTION Malformations of the hands and feet are common and of many kinds. Ac- cording to Gates (1946) there probably are more abnormalities of the hands and feet than of any other part of the body, with the exception of the eye. It is true that some hand and foot anomalies are the result of accident and disease but it is equally true that many are the result of variation in heredity. The extent to which the latter is true and the mode of inheritance of those variations which have some genetic basis are questions which are not com- pletely answered. Hence when an opportunity presented itself to study a number of different hand and foot anomalies which appeared to have a he- reditary basis, it seemed worthwhile to investigate them and to present the findings. The malformations which are included are syndactyly and split hand and foot, polydactyly, and brachydactyly. Each will be considered more or less independently and in the order indicated. A BRIEF REVIEW OF LITERATURE 1. Syndactyly and Split Hand and Foot Syndactyly is the condition in which two or more fingers or toes are adherent or are more or less completely grown together. Split hand and foot (also called lobster claw) is a deformity in which the central digits of the hands and/or feet are lacking. It may represent an extreme variant of syndactyly. According to Lewis (1909) a description of split hand and foot is difficult because of the great variation in the deformity even within the same family. -

The Rheumatoid Thumb
THE RHEUMATOID THUMB BY ANDREW L. TERRONO, MD The thumb is frequently involved in patients with rheumatoid arthritis. Thumb postures can be grouped into a number of deformities. Deformity is determined by a complex interaction of the primary joint, the adjacent joints, and tendon function and integrity. Joints adjacent to the primarily affected one usually assume an opposite posture. If they do not, tendon ruptures should be suspected. Surgical treatment is individualized for each patient and each joint, with consideration given to adjacent joints. The treatment consists of synovectomy, capsular reconstruction, tendon reconstruction, joint stabilization, arthrodesis, or arthroplasty. Copyright © 2001 by the American Society for Surgery of the Hand he majority of patients with rheumatoid ar- ring between the various joints. Any alteration of thritis will develop thumb involvement.1,2,3 posture at one level has an effect on the adjacent joint. TThe deformities encountered in the rheuma- The 6 patterns of thumb postures described here, toid patient are varied and are the result of changes unfortunately, do not exhaust the deformities one taking place both intrinsically and extrinsically to the encounters in rheumatoid arthritis (Table 1). It is thumb. Synovial hypertrophy within the individual possible, for example, for the patient to stretch the thumb joints leads not only to destruction of articular supporting structures of a joint, causing a flexion, cartilage, but can also stretch out the supporting extension, or lateral deformity. However, instead of collateral ligaments and joint capsules. As a result, the adjacent joint assuming the opposite posture, it each joint can become unstable and react to the may assume an abnormal position secondary to a stresses applied to it both in function against the other tendon rupture. -

Four Unusual Cases of Congenital Forelimb Malformations in Dogs
animals Article Four Unusual Cases of Congenital Forelimb Malformations in Dogs Simona Di Pietro 1 , Giuseppe Santi Rapisarda 2, Luca Cicero 3,* , Vito Angileri 4, Simona Morabito 5, Giovanni Cassata 3 and Francesco Macrì 1 1 Department of Veterinary Sciences, University of Messina, Viale Palatucci, 98168 Messina, Italy; [email protected] (S.D.P.); [email protected] (F.M.) 2 Department of Veterinary Prevention, Provincial Health Authority of Catania, 95030 Gravina di Catania, Italy; [email protected] 3 Institute Zooprofilattico Sperimentale of Sicily, Via G. Marinuzzi, 3, 90129 Palermo, Italy; [email protected] 4 Veterinary Practitioner, 91025 Marsala, Italy; [email protected] 5 Ospedale Veterinario I Portoni Rossi, Via Roma, 57/a, 40069 Zola Predosa (BO), Italy; [email protected] * Correspondence: [email protected] Simple Summary: Congenital limb defects are sporadically encountered in dogs during normal clinical practice. Literature concerning their diagnosis and management in canine species is poor. Sometimes, the diagnosis and description of congenital limb abnormalities are complicated by the concurrent presence of different malformations in the same limb and the lack of widely accepted classification schemes. In order to improve the knowledge about congenital limb anomalies in dogs, this report describes the clinical and radiographic findings in four dogs affected by unusual congenital forelimb defects, underlying also the importance of reviewing current terminology. Citation: Di Pietro, S.; Rapisarda, G.S.; Cicero, L.; Angileri, V.; Morabito, Abstract: Four dogs were presented with thoracic limb deformity. After clinical and radiographic S.; Cassata, G.; Macrì, F. Four Unusual examinations, a diagnosis of congenital malformations was performed for each of them. -
![August 2011 [KZ 6266] Sub](https://docslib.b-cdn.net/cover/0451/august-2011-kz-6266-sub-1440451.webp)
August 2011 [KZ 6266] Sub
August 2011 [KZ 6266] Sub. Code : 6266 BACHELOR OF PHYSIOTHERAPY EXAMINATION FOURTH YEAR / SEVENTH SEMESTER CLINICAL ORTHOPAEDICS Q.P. Code : 746266 Time : Three hours Maximum : 100 marks ANSWER ALL QUESTIONS I. LONG ESSAYS (2X20=40) 1. Describe the mechanism of injury, complications and management of supra- condylar fracture of humerus. 2. Outline the etiopathology of Rheumatoid arthritis. Describe the deformities that occur in a rheumatoid hand and its management. II. SHORT NOTES (8X5=40) 1. Periarthritis shoulder. 2. Scaphoid fracture. 3. Sequestrum. 4. Cobb’s angle. 5. Cervical rib. 6. Torticollis. 7. Spondylolisthesis. 8. Fracture Patella. III. SHORT ANSWERS (10X2=20) 1. Green stick fracture. 2. Hallux Valgus. 3. Subluxation. 4. Carpal bones. 5. Delayed union. 6. Volkman’s sign. 7. Mc. Murrays test. 8. Scapulo-humeral rhythm. 9. Antalgic gait. 10.Hypothenar muscles of hand. ******* February 2012 [LA 6266] Sub. Code: 6266 BACHELOR OF PHYSIOTHERAPY EXAMINATION FOURTH YEAR / SEVENTH SEMESTER CLINICAL ORTHOPAEDICS Q.P. Code: 746266 Time: Three Hours Maximum: 100 marks Answer ALL questions I. Elaborate on: (2X20=40) 1. Describe the causes, clinical features and management of recurrent dislocation of the shoulder. 2. Describe the clinical features, complications and management of a patient with fracture of D8 vertebra with paraplegia. II. Write notes on: (8X5=40) 1. DeQuervains disease. 2. March fracture. 3. Ulnar claw hand. 4. Fracture disease. 5. Anterior cruciate ligament. 6. Potts fracture. 7. Shoulder hand syndrome 8. Myositis Ossificans III. Short Answers: (10X2=20) 1. Z-Thumb deformity. 2. Hallux valgus. 3. Guillotine amputation. 4. Mallet finger. 5. Elys test 6. Complications of Scaphoid fracture. -

Report: Rs04362-R1362 North Carolina Department of Health and Human Services Nurse Practitioners Fee Schedule As Of: 9/19/2019
REPORT: RS04362-R1362 NORTH CAROLINA DEPARTMENT OF HEALTH AND HUMAN SERVICES NURSE PRACTITIONERS FEE SCHEDULE AS OF: 9/19/2019 Nurse Practitioner Fee Schedule Provider Specialty 061 Fee Schedule Updated on: 9/19/2019 ***The Agency's fee schedule rates below were set as of January 1, 2014 unless otherwise noted*** Rate changes after January 1, 2014 are based on the January 1st RVU of the year in which the service was initally established The inclusion of a rate on this table does not guarantee that a service is covered. Please refer to the Medicaid Billing Guide and the Medicaid and Health Choice Clinical Policies on the DHB Web Site. Providers should always bill their usual and customary charges. Please use the monthly NC Medicaid Bulletins for additions, changes and deletion to this schedule. Medicaid Maximum Allowable PROCEDURE NON-FACILITY Effective Date of CODE MODIFIER PROCEDURE DESCRIPTION FACILITY RATE RATE Rate 10004 FNA BX W/O IMG GDN EA ADDL $ 36.98 $ 43.90 2019-01-01 10005 FNA BX W/US GDN 1ST LES $ 62.62 $ 105.61 2019-01-01 10006 FNA BX W/US GDN EA ADDL $ 42.67 $ 50.75 2019-01-01 10007 FNA BX W/FLUOR GDN 1ST LES $ 80.39 $ 235.92 2019-01-01 10008 FNA BX W/FLUOR GDN EA ADDL $ 52.43 $ 133.22 2019-01-01 10009 FNA BX W/CT GDN 1ST LES $ 97.58 $ 385.27 2019-01-01 10010 FNA BX W/CT GDN EA ADDL $ 71.32 $ 232.62 2019-01-01 11055 PARING OR CUTTING OF BENIGN HYPERKERATOT $ 17.61 $ 34.39 11056 TRIM SKIN LESIONS 2 TO 4 $ 24.83 $ 42.18 11057 TRIM SKIN LESIONS OVER 4 $ 32.24 $ 50.98 11102 TANGNTL BX SKIN SINGLE LES $ 33.65 $ 81.55 2019-01-01 -

Spectrum of Joint Deformities in Children with Juvenile Idiopathic Arthritis Samia Naz1, Misbah Asif2, Farrah Naz1, Hina Farooq3 and Muhammad Haroon Hamid1
CLINICAL PRACTICE ARTICLE Spectrum of Joint Deformities in Children with Juvenile Idiopathic Arthritis Samia Naz1, Misbah Asif2, Farrah Naz1, Hina Farooq3 and Muhammad Haroon Hamid1 ABSTRACT Objective: To determine the frequency and types of joint deformities in children with juvenile idiopathic arthritis and their association with clinical parameters and rheumatoid factor. Study Design: Cross-sectional study. Place and Duration of Study: Rheumatology Outpatient Clinic, the Children's Hospital and the Institute of Child Health, Lahore, from September 2014 to February 2015. Methodology: All patients of both genders of less than 16 years of age, who fulfilled the International League of Association for Rheumatology (ILAR) criteria for Juvenile Idiopathic Arthritis (JIA), were enrolled in this study. Their demographic data, duration of disease at the time of presentation, types of JIA, various joint deformities and rheumatoid factor (RF) were documented. Statistical analysis of data was done on SPSS version 16. Chi-square test was applied to determine the association of clinical deformity with age of patients, disease duration at presentation, types of JIA and RF. Results: Out of 70 patients enrolled during the study period, 51.4% were boys with mean age at presentation being 9.44 ±3.89 years (2-7 years) and median duration of disease being 24 months (interquartile range 42 months). Forty patients (57.1%) had joint deformities. Most common joints involved were hand (50%), wrist (50%), and knee (35.7%). The common types of joint deformities were boutonniere deformity (28.6%), ulnar deviation of wrist (28.6%), fixed flexion deformity of wrist (22.9%), and knee (31.4%). -
Extremities Exam Codes Code Description 1 2500 Coldness
Jan-07 Fernald Medical Monitoring Program Sort Code Physician Exam - Extremities Exam Codes Code Description 1 2500 coldness 2 2501 increased pallor 3 2502 delayed color return 4 2503 arterial insufficiency 5 2505 dermatitis without ulceration 6 2506 psoriatic rash 7 8 2507 cellulitis 9 2508 necrotic skin changes 10 11 2510 deformity R hand 12 2511 deformity R arm 13 2512 deformity L hand 14 2513 deformity L arm 15 2514 deformity R foot 16 2515 deformity R leg 17 2516 deformity L foot 18 2517 deformity L leg 19 2518 mild joint deformity 20 2519 deformed finger/s 21 4547 Osteogenesis Imperecta 22 23 2520 pallor or cyanosis of fingers 24 2521 Raynaud's phenomenon 25 2522 mycosis (fungal infection of nails) 26 2952 nail bites 27 2523 degeneration of metatarsal phalanges joints 28 2538 moderate contractures of fingers 29 2629 decreased ROM, fingers 30 2659 cyst on finger 31 2524 amputation of fingers 32 2526 swollen fingers 33 2613 scarring of nail bed 34 2951 clubbing of nails 35 36 2525 arm tender 37 2530 diminished radial pulses 38 2531 diminished R radial pulse 39 2532 diminished L radial pulse 40 2533 absent radial pulses 41 2534 absent R radial pulse 42 2535 absent L radial pulse 43 2536 degenerative changes noted of metacarpal-phalangeal joints 44 2537 enlargement of TP joints of fingers 45 2539 crepitus in wrists 46 2666 swelling wrist 47 2664 cyst on wrist 48 Code Description 1 2529 subluxation of interphalangeal joint (IJ) 49 2609 protusion of proximal head of radius 50 51 2540 thenar atrophy 52 2541 carpal tunnel syndrome 53 2542