Upper Limb Injuries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ICD-10 Diagnoses on Router
L ARTHRITIS R L HAND R L ANKLE R L FRACTURES R OSTEOARTHRITIS: PRIMARY, 2°, POST TRAUMA, POST _____ CONTUSION ACHILLES TEN DYSFUNCTION/TENDINITIS/RUPTURE FLXR TEN CLAVICLE: STERNAL END, SHAFT, ACROMIAL END CRYSTALLINE ARTHRITIS: GOUT: IDIOPATHIC, LEAD, CRUSH INJURY AMPUTATION TRAUMATIC LEVEL SCAPULA: ACROMION, BODY, CORACOID, GLENOID DRUG, RENAL, OTHER DUPUYTREN’S CONTUSION PROXIMAL HUMERUS: SURGICAL NECK 2 PART 3 PART 4 PART CRYSTALLINE ARTHRITIS: PSEUDOGOUT: HYDROXY LACERATION: DESCRIBE STRUCTURE CRUSH INJURY PROXIMAL HUMERUS: GREATER TUBEROSITY, LESSER TUBEROSITY DEP DIS, CHONDROCALCINOSIS LIGAMENT DISORDERS EFFUSION HUMERAL SHAFT INFLAMMATORY: RA: SEROPOSITIVE, SERONEGATIVE, JUVENILE OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ LOOSE BODY HUMERUS DISTAL: SUPRACONDYLAR INTERCONDYLAR REACTIVE: SECONDARY TO: INFECTION ELSEWHERE, EXTENSION OR NONE INTESTINAL BYPASS, POST DYSENTERIC, POST IMMUNIZATION PAIN OCD TALUS HUMERUS DISTAL: TRANSCONDYLAR NEUROPATHIC CHARCOT SPRAIN HAND: JOINT? OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ HUMERUS DISTAL: EPICONDYLE LATERAL OR MEDIAL AVULSION INFECT: PYOGENIC: STAPH, STREP, PNEUMO, OTHER BACT TENDON RUPTURES: EXTENSOR OR FLEXOR PAIN HUMERUS DISTAL: CONDYLE MEDIAL OR LATERAL INFECTIOUS: NONPYOGENIC: LYME, GONOCOCCAL, TB TENOSYNOVITIS SPRAIN, ANKLE, CALCANEOFIBULAR ELBOW: RADIUS: HEAD NECK OSTEONECROSIS: IDIOPATHIC, DRUG INDUCED, SPRAIN, ANKLE, DELTOID POST TRAUMATIC, OTHER CAUSE SPRAIN, ANKLE, TIB-FIB LIGAMENT (HIGH ANKLE) ELBOW: OLECRANON WITH OR WITHOUT INTRA ARTICULAR EXTENSION SUBLUXATION OF ANKLE, -

Upper Extremity
Upper Extremity Shoulder Elbow Wrist/Hand Diagnosis Left Right Diagnosis Left Right Diagnosis Left Right Adhesive capsulitis M75.02 M75.01 Anterior dislocation of radial head S53.015 [7] S53.014 [7] Boutonniere deformity of fingers M20.022 M20.021 Anterior dislocation of humerus S43.015 [7] S43.014 [7] Anterior dislocation of ulnohumeral joint S53.115 [7] S53.114 [7] Carpal Tunnel Syndrome, upper limb G56.02 G56.01 Anterior dislocation of SC joint S43.215 [7] S43.214 [7] Anterior subluxation of radial head S53.012 [7] S53.011 [7] DeQuervain tenosynovitis M65.42 M65.41 Anterior subluxation of humerus S43.012 [7] S43.011 [7] Anterior subluxation of ulnohumeral joint S53.112 [7] S53.111 [7] Dislocation of MCP joint IF S63.261 [7] S63.260 [7] Anterior subluxation of SC joint S43.212 [7] S43.211 [7] Contracture of muscle in forearm M62.432 M62.431 Dislocation of MCP joint of LF S63.267 [7] S63.266 [7] Bicipital tendinitis M75.22 M75.21 Contusion of elbow S50.02X [7] S50.01X [7] Dislocation of MCP joint of MF S63.263 [7] S63.262 [7] Bursitis M75.52 M75.51 Elbow, (recurrent) dislocation M24.422 M24.421 Dislocation of MCP joint of RF S63.265 [7] S63.264 [7] Calcific Tendinitis M75.32 M75.31 Lateral epicondylitis M77.12 M77.11 Dupuytrens M72.0 Contracture of muscle in shoulder M62.412 M62.411 Lesion of ulnar nerve, upper limb G56.22 G56.21 Mallet finger M20.012 M20.011 Contracture of muscle in upper arm M62.422 M62.421 Long head of bicep tendon strain S46.112 [7] S46.111 [7] Osteochondritis dissecans of wrist M93.232 M93.231 Primary, unilateral -

SURGICAL TECHNIQUE PIP Total Joint – Dorsal Approach Table of Contents
® Ascension SURGICAL TECHNIQUE PIP Total Joint – Dorsal Approach Table of Contents Introduction Humanitarian Device .................................................................................................................................................................2 Indications ................................................................................................................................................................................2 Contraindications ......................................................................................................................................................................2 Warnings and Precautions ......................................................................................................................................................... 3 Keys to Successful PIP Replacement ...........................................................................................................................................4 Surgical Technique Preoperative Assessment .......................................................................................................................................................... 5 Step 1: Skin Incision, Capsular Opening and Exposure ................................................................................................................ 5 Step 2: Medullary Canal Opening and Alignment ........................................................................................................................6 Step 3: First -

Cancer Lung: an Unusual Presentation
www.ijmpo.org CA se Re po RT Cancer lung: An unusual presentation Shankar L. Jakhar, ABSTRACT Rohitashwa Dana, D. P. Punia Phalanx bone metastasis as the initial manifestation of lung cancer is a rare presentation. Department of Radiotherapy, A 70-year-old man presented with swelling and pain in his right ring finger. He had no Mathura Das Mathur Hospital, other complaints or abnormal findings on clinical examination. A right hand radiograph Dr. Sampurnanand Medical showed an osteolytic lesion in the first phalanx of the ring finger. Fine needle aspiration College, Jodhpur, Rajasthan, cytology of the swelling suggested a metastatic adenocarcinoma. A skeletal survey, India hematological, biochemical, and other radiological tests were found to be normal, except for an opacity seen in the right lung midzone. A bronchoscopic biopsy revealed Address for correspondence: adenocarcinoma of the lung. Dr. Shankar Lal Jakhar, Department of Radiotherapy, Mathura Das Mathur Hospital, Key words: Bone metastasis, cancer lung, phalanx Jodhpur, Rajasthan, India. E-mail: [email protected] DOI: 10.4103/0971-5851.65343 INTRODUCTION of the lung. A bone scan showed increased uptake in the proximal phalanx of the right ring finger. We planned Bone metastases from the lung cancer may occur early in systemic chemotherapy and palliative radiotherapy to the the clinical course and are usually discovered to exist with finger with a nonsteroidal analgesic for relieving pain. pain.[1,2] The spine and ribs are often the earliest sites of bone metastases, whereas, the skull, femur, humerus, and scapula DISCUSSION are involved later.[3] Metastases to the hands are rare events with around 200 cases reported in the literature.[4-8] They Bone metastasis in distal parts of the extremities is [9-11] comprise only 0.1% of all osseous metastases. -
Real Bodies Educator Guide
EDUCATOR GUIDE TABLE OF CONTENTS REAL BODIES EDUCATOR GUIDE INTRODUCTION TO THE EXHIBITION ........................................................................................................3 ABOUT THIS GUIDE ................................................................................................................................................3 ANATOMIST’S STUDY: THINK: SKELETAL SYSTEM ....................................... 4 NERVOUS SYSTEM .......................................... 14 Talking Points . 4 Talking Points . 14 Activity: Egg Carton Spinal Cord . 5 Activity: Memory Quiz . 15 BREATH: WHAT BECOMES OF US: RESPIRATORY SYSTEM ............................... 6 DEATH .................................................................... 16 Talking Points . 6 Talking Points . 16 Activity: Plastic Bottle Lung . 7 Activity: Living, Not Living, or Dead . 17 HUNGER: LOVE : DIGESTIVE SYSTEM ....................................... 8 REPRODUCTIVE SYSTEM ........................... 18 Talking Points . 8 Talking Points . 18 Activity: Bread Digestion . 9 Activity: What is Love? . 19 RYTHMN: FETAL DEVELOPMENT: ............................. 20 CIRCULATORY SYSTEM ............................... 10 Talking Points . 20 Talking Points . 10 Activity: Fruit Development . 20 Activity: What’s In Your Blood? . 11 REPAIRS: MOVE : MEDICINE AND BODY REPAIRS ............ 21 MUSCULAR SYSTEM ..................................... 12 Talking Points . 21 Talking Points . 12 Activity: Surgeons . 23 Activity: Which Muscle? . 13 REAL BODIES | EDUCATOR -

The Rheumatoid Thumb
THE RHEUMATOID THUMB BY ANDREW L. TERRONO, MD The thumb is frequently involved in patients with rheumatoid arthritis. Thumb postures can be grouped into a number of deformities. Deformity is determined by a complex interaction of the primary joint, the adjacent joints, and tendon function and integrity. Joints adjacent to the primarily affected one usually assume an opposite posture. If they do not, tendon ruptures should be suspected. Surgical treatment is individualized for each patient and each joint, with consideration given to adjacent joints. The treatment consists of synovectomy, capsular reconstruction, tendon reconstruction, joint stabilization, arthrodesis, or arthroplasty. Copyright © 2001 by the American Society for Surgery of the Hand he majority of patients with rheumatoid ar- ring between the various joints. Any alteration of thritis will develop thumb involvement.1,2,3 posture at one level has an effect on the adjacent joint. TThe deformities encountered in the rheuma- The 6 patterns of thumb postures described here, toid patient are varied and are the result of changes unfortunately, do not exhaust the deformities one taking place both intrinsically and extrinsically to the encounters in rheumatoid arthritis (Table 1). It is thumb. Synovial hypertrophy within the individual possible, for example, for the patient to stretch the thumb joints leads not only to destruction of articular supporting structures of a joint, causing a flexion, cartilage, but can also stretch out the supporting extension, or lateral deformity. However, instead of collateral ligaments and joint capsules. As a result, the adjacent joint assuming the opposite posture, it each joint can become unstable and react to the may assume an abnormal position secondary to a stresses applied to it both in function against the other tendon rupture. -
![August 2011 [KZ 6266] Sub](https://docslib.b-cdn.net/cover/0451/august-2011-kz-6266-sub-1440451.webp)
August 2011 [KZ 6266] Sub
August 2011 [KZ 6266] Sub. Code : 6266 BACHELOR OF PHYSIOTHERAPY EXAMINATION FOURTH YEAR / SEVENTH SEMESTER CLINICAL ORTHOPAEDICS Q.P. Code : 746266 Time : Three hours Maximum : 100 marks ANSWER ALL QUESTIONS I. LONG ESSAYS (2X20=40) 1. Describe the mechanism of injury, complications and management of supra- condylar fracture of humerus. 2. Outline the etiopathology of Rheumatoid arthritis. Describe the deformities that occur in a rheumatoid hand and its management. II. SHORT NOTES (8X5=40) 1. Periarthritis shoulder. 2. Scaphoid fracture. 3. Sequestrum. 4. Cobb’s angle. 5. Cervical rib. 6. Torticollis. 7. Spondylolisthesis. 8. Fracture Patella. III. SHORT ANSWERS (10X2=20) 1. Green stick fracture. 2. Hallux Valgus. 3. Subluxation. 4. Carpal bones. 5. Delayed union. 6. Volkman’s sign. 7. Mc. Murrays test. 8. Scapulo-humeral rhythm. 9. Antalgic gait. 10.Hypothenar muscles of hand. ******* February 2012 [LA 6266] Sub. Code: 6266 BACHELOR OF PHYSIOTHERAPY EXAMINATION FOURTH YEAR / SEVENTH SEMESTER CLINICAL ORTHOPAEDICS Q.P. Code: 746266 Time: Three Hours Maximum: 100 marks Answer ALL questions I. Elaborate on: (2X20=40) 1. Describe the causes, clinical features and management of recurrent dislocation of the shoulder. 2. Describe the clinical features, complications and management of a patient with fracture of D8 vertebra with paraplegia. II. Write notes on: (8X5=40) 1. DeQuervains disease. 2. March fracture. 3. Ulnar claw hand. 4. Fracture disease. 5. Anterior cruciate ligament. 6. Potts fracture. 7. Shoulder hand syndrome 8. Myositis Ossificans III. Short Answers: (10X2=20) 1. Z-Thumb deformity. 2. Hallux valgus. 3. Guillotine amputation. 4. Mallet finger. 5. Elys test 6. Complications of Scaphoid fracture. -

A Comprehensive Analysis of the Butchering Activities Performed at the Fincastle Bison Kill Site (D1ox-5)
University of Lethbridge Research Repository OPUS http://opus.uleth.ca Theses Arts and Science, Faculty of 2008 A comprehensive analysis of the butchering activities performed at the Fincastle Bison Kill Site (D1Ox-5) Watts, Angela (Ang) Lethbridge, Alta. : University of Lethbridge, Faculty of Arts and Science, 2008 http://hdl.handle.net/10133/748 Downloaded from University of Lethbridge Research Repository, OPUS A COMPREHENSIVE ANALYSIS OF THE BUTCHERING ACTIVITIES PERFORMED AT THE FINCASTLE BISON KILL SITE (DlOx-5) ANGELA (ANG) WATTS B.A., The University of Lethbridge, 2004 A Thesis Submitted to the School of Graduate Studies of The University of Lethbridge in Partial Fulfillment of the Requirements for the Degree MASTER OF SCIENCE Department of Geography, The University of Lethbridge LETHBRIDGE, ALBERTA, CANADA ©Angela (Ang) Watts, 2008 Dedication This thesis is dedicated to my family (Dad, Mum, Dave and crew!) who have been, and always will be, my #1 fan, no matter what I do, or where I end up. Finally, to Shawn, my professor, but even more so, my friend, who convinced me that I could win the hardest battle that I have ever been faced with; completing my masters. iii 1. ABSTRACT The Fincastle site (DlOx-5) is located in Southern Alberta, Canada. Excavations from 2004-2007 unearthed a significant number of lithic artefacts, fire-broken rock and a dense bone bed. Radiocarbon dates (ca. 2500 BP) place the single occupancy kill site in the Late Middle Prehistoric Period. This thesis investigates the butchering activities that took place in the East Block of the site, where 60,000 bone fragments were collected. -

Hollows and Folds of the Body
Hollows and folds of the body by David Mead 2017 Sulang Language Data and Working Papers: Topics in Lexicography, no. 31 Sulawesi Language Alliance http://sulang.org/ SulangLexTopics031-v2 LANGUAGES Language of materials : English DESCRIPTION/ABSTRACT In this paper I discuss certain hollows, notches, and folds of the surface anatomy of the human body, features which might otherwise go overlooked in your lexicographical research. Along the way I also mention names for wrinkles of the face and fold lines of the hands. TABLE OF CONTENTS Head; Face; Neck, chest, and abdomen; Back and buttocks; Arms and hands; Legs and feet; References; Appendix: Bones of the body. VERSION HISTORY Version 2 [29 May 2017] Edits to ‘fontanelle’ and ‘straie,’ order of references and appendix reversed, minor edits to appendix. Version 1 [15 May 2017] Drafted September 2010, revised June 2013, revised for publication May 2017. © 2017 by David Mead. Text is licensed under terms of the Creative Commons Attribution- ShareAlike 4.0 International license. Images are licensed as individually noted. Hollows and folds of the body by David Mead Who has measured the waters in the hollow of his hand, or with the breadth of his hand marked off the heavens? Isaiah 40:12 Names for the parts of the human body are universal to human language. In fact names for salient body parts are considered part of the basic or core vocabulary of a language, and are often some of the first words elicited when learning a language. In this paper I want to raise your awareness concerning certain less salient features of the surface anatomy of the body that may otherwise go overlooked in your lexicography research. -

Spectrum of Joint Deformities in Children with Juvenile Idiopathic Arthritis Samia Naz1, Misbah Asif2, Farrah Naz1, Hina Farooq3 and Muhammad Haroon Hamid1
CLINICAL PRACTICE ARTICLE Spectrum of Joint Deformities in Children with Juvenile Idiopathic Arthritis Samia Naz1, Misbah Asif2, Farrah Naz1, Hina Farooq3 and Muhammad Haroon Hamid1 ABSTRACT Objective: To determine the frequency and types of joint deformities in children with juvenile idiopathic arthritis and their association with clinical parameters and rheumatoid factor. Study Design: Cross-sectional study. Place and Duration of Study: Rheumatology Outpatient Clinic, the Children's Hospital and the Institute of Child Health, Lahore, from September 2014 to February 2015. Methodology: All patients of both genders of less than 16 years of age, who fulfilled the International League of Association for Rheumatology (ILAR) criteria for Juvenile Idiopathic Arthritis (JIA), were enrolled in this study. Their demographic data, duration of disease at the time of presentation, types of JIA, various joint deformities and rheumatoid factor (RF) were documented. Statistical analysis of data was done on SPSS version 16. Chi-square test was applied to determine the association of clinical deformity with age of patients, disease duration at presentation, types of JIA and RF. Results: Out of 70 patients enrolled during the study period, 51.4% were boys with mean age at presentation being 9.44 ±3.89 years (2-7 years) and median duration of disease being 24 months (interquartile range 42 months). Forty patients (57.1%) had joint deformities. Most common joints involved were hand (50%), wrist (50%), and knee (35.7%). The common types of joint deformities were boutonniere deformity (28.6%), ulnar deviation of wrist (28.6%), fixed flexion deformity of wrist (22.9%), and knee (31.4%). -
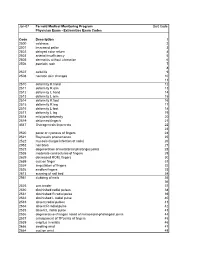
Extremities Exam Codes Code Description 1 2500 Coldness
Jan-07 Fernald Medical Monitoring Program Sort Code Physician Exam - Extremities Exam Codes Code Description 1 2500 coldness 2 2501 increased pallor 3 2502 delayed color return 4 2503 arterial insufficiency 5 2505 dermatitis without ulceration 6 2506 psoriatic rash 7 8 2507 cellulitis 9 2508 necrotic skin changes 10 11 2510 deformity R hand 12 2511 deformity R arm 13 2512 deformity L hand 14 2513 deformity L arm 15 2514 deformity R foot 16 2515 deformity R leg 17 2516 deformity L foot 18 2517 deformity L leg 19 2518 mild joint deformity 20 2519 deformed finger/s 21 4547 Osteogenesis Imperecta 22 23 2520 pallor or cyanosis of fingers 24 2521 Raynaud's phenomenon 25 2522 mycosis (fungal infection of nails) 26 2952 nail bites 27 2523 degeneration of metatarsal phalanges joints 28 2538 moderate contractures of fingers 29 2629 decreased ROM, fingers 30 2659 cyst on finger 31 2524 amputation of fingers 32 2526 swollen fingers 33 2613 scarring of nail bed 34 2951 clubbing of nails 35 36 2525 arm tender 37 2530 diminished radial pulses 38 2531 diminished R radial pulse 39 2532 diminished L radial pulse 40 2533 absent radial pulses 41 2534 absent R radial pulse 42 2535 absent L radial pulse 43 2536 degenerative changes noted of metacarpal-phalangeal joints 44 2537 enlargement of TP joints of fingers 45 2539 crepitus in wrists 46 2666 swelling wrist 47 2664 cyst on wrist 48 Code Description 1 2529 subluxation of interphalangeal joint (IJ) 49 2609 protusion of proximal head of radius 50 51 2540 thenar atrophy 52 2541 carpal tunnel syndrome 53 2542 -

The Ehlers-Danlos Syndromes, Rare Types
American Journal of Medical Genetics Part C (Seminars in Medical Genetics) 175C:70–115 (2017) RESEARCH REVIEW The Ehlers–Danlos Syndromes, Rare Types ANGELA F. BRADY, SERWET DEMIRDAS, SYLVIE FOURNEL-GIGLEUX, NEETI GHALI, CECILIA GIUNTA, INES KAPFERER-SEEBACHER, TOMOKI KOSHO, ROBERTO MENDOZA-LONDONO, MICHAEL F. POPE, MARIANNE ROHRBACH, TIM VAN DAMME, ANTHONY VANDERSTEEN, CAROLINE VAN MOURIK, NICOL VOERMANS, JOHANNES ZSCHOCKE, AND FRANSISKA MALFAIT * Dr. Angela F. Brady, F.R.C.P., Ph.D., is a Consultant Clinical Geneticist at the North West Thames Regional Genetics Service, London and she has a specialist interest in Ehlers–Danlos Syndrome. She was involved in setting up the UK National EDS Diagnostic Service which was established in 2009 and she has been working in the London part of the service since 2015. Dr. Serwet Demirdas, M.D., Ph.D., is a clinical geneticist in training at the Erasmus Medical Center (Erasmus University in Rotterdam, the Netherlands), where she is involved in the clinical service and research into the TNX deficient type of EDS. Prof. Sylvie Fournel-Gigleux, Pharm.D., Ph.D., is a basic researcher in biochemistry/pharmacology, Research Director at INSERM (Institut National de la Sante et de la Recherche Medicale) and co-head of the MolCelTEG Research Team at UMR 7561 CNRS-Universite de Lorraine. Her group is dedicated to the pathobiology of connective tissue disorders, in particular the Ehlers–Danlos syndromes, and specializes on the molecular and structural basis of glycosaminoglycan synthesis enzyme defects. Dr. Neeti Ghali, M.R.C.P.C.H., M.D., is a Consultant Clinical Geneticist at the North West Thames Regional Genetics Service, London and she has a specialist interest in Ehlers–Danlos Syndrome.