The First Year of a Brief Psychiatric Screening Clinic in Primary Care
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

THE PINNING STONES Culture and Community in Aberdeenshire
THE PINNING STONES Culture and community in Aberdeenshire When traditional rubble stone masonry walls were originally constructed it was common practice to use a variety of small stones, called pinnings, to make the larger stones secure in the wall. This gave rubble walls distinctively varied appearances across the country depend- ing upon what local practices and materials were used. Historic Scotland, Repointing Rubble First published in 2014 by Aberdeenshire Council Woodhill House, Westburn Road, Aberdeen AB16 5GB Text ©2014 François Matarasso Images ©2014 Anne Murray and Ray Smith The moral rights of the creators have been asserted. ISBN 978-0-9929334-0-1 This work is licensed under the Creative Commons Attribution-Non-Commercial-No Derivative Works 4.0 UK: England & Wales. You are free to copy, distribute, or display the digital version on condition that: you attribute the work to the author; the work is not used for commercial purposes; and you do not alter, transform, or add to it. Designed by Niamh Mooney, Aberdeenshire Council Printed by McKenzie Print THE PINNING STONES Culture and community in Aberdeenshire An essay by François Matarasso With additional research by Fiona Jack woodblock prints by Anne Murray and photographs by Ray Smith Commissioned by Aberdeenshire Council With support from Creative Scotland 2014 Foreword 10 PART ONE 1 Hidden in plain view 15 2 Place and People 25 3 A cultural mosaic 49 A physical heritage 52 A living heritage 62 A renewed culture 72 A distinctive voice in contemporary culture 89 4 Culture and -

The Fishing-Boat Harbours of Fraserburgh, Sandhaven, Arid Portsoy, on the North-East Coaxt of Scotland.” by JOHNWILLET, M
Prooeedings.1 WILLET ON FRASERBURGH HARBOUR. 123 (Paper No. 2197.) ‘I The Fishing-Boat Harbours of Fraserburgh, Sandhaven, arid Portsoy, on the North-East Coaxt of Scotland.” By JOHNWILLET, M. Inst. C.E. ALONGthe whole line of coast lying between the Firth of Forth and Cromarty Firth, at least 160 miles in length, little natural protection exists for fishing-boats. The remarkable development, however, of the herring-fishery, during the last thirty years, has induced Harbour Boards and owners of private harbours, at several places along the Aberdeenshire and Banffshire coasts, to improve theshelter and increase the accommodation of their harbours, in the design and execution of which works the Author has been engaged for the last twelve years. FIXASERBURGHHARBOUR. Fraserburgh may be regarded as t,he chief Scottish port of the herring-fishery. In 1854, the boats hailing from Fraserburgh during the fishing season were three hundred and eighty-nine, and in 1885 seven hundred and forty-two, valued with their nets and lines atS’255,OOO ; meanwhile the revenue of the harbour increased from 51,743 in 1854 to 59,281 in 1884. The town and harbour are situated on the west side of Fraserburgh Bay, which faces north- north-east, and is about 2 miles longand 1 mile broad. The harbour is sheltered by land, except between north-west and east- south-east. The winds from north round to east bring the heaviest seas into the harbour. The flood-tide sets from Kinnaird Head, at the western extremity of the bay, to Cairnbulg Point at the east, with a velocity of 24 knots an hour ; and the ebb-tide runs in a north-easterly direction from the end of thebreakwater. -

Short Walks in Scotland Under 10 Km Cairnbulg-Whitelinks Bay-St Combs
The Mack Walks: Short Walks in Scotland Under 10 km Cairnbulg-Whitelinks Bay-St Combs Circuit (Aberdeenshire) Route Summary This is a bracing walk along the windy coastline at the NE corner of Scotland passing through evocative old fishing villages and crossing the wonderful crescent-shaped beach at Whitelinks Bay. Duration: 2.75 hours. Route Overview Duration: 2.75 hours. Transport/Parking: Stagecoach 69 bus service from Fraserburgh. Check timetable. Free parking at walk start/finish, Cairnbulg Harbour. Length: 8.170 km / 5.11 mi Height Gain: 60 meter. Height Loss: 60 meter. Max Height: 16 meter. Min Height: 0 meter. Surface: Moderate. Mostly on paved surfaces. Some walking on good grassy tracks and a section of beach walking. Difficulty: Easy. Child Friendly: Yes, if children are used to walks of this distance. Dog Friendly: Yes, but keep dogs on lead on public roads. Refreshments: Options in Fraserburgh. Description This is an enjoyable circuit along the airy coast between Cairnbulg and St Combs, on the “Knuckle of North East Scotland”, where the coastline turns west from the more exposed North Sea to the increasingly more sheltered Moray Firth. The combined villages of Cairnbulg and Inverallochy (the local Community Council is now called “Invercairn”) have a long association with the fishing industry, although as the nature of fishing operations changed, the locus moved to nearby Fraserburgh. The inadequate nature of the original fisher huts was cruelly exposed in the cholera epidemics of the 1860s and they were cleared to make way for planned settlements centred on Inverallochy and Cairnbulg and, a little further down the coast, at St Combs. -
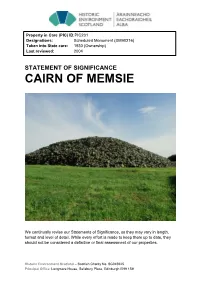
Cairn of Memsie Statement of Significance
Property in Care (PIC) ID: PIC231 Designations: Scheduled Monument (SM90216) Taken into State care: 1930 (Ownership) Last reviewed: 2004 STATEMENT OF SIGNIFICANCE CAIRN OF MEMSIE We continually revise our Statements of Significance, so they may vary in length, format and level of detail. While every effort is made to keep them up to date, they should not be considered a definitive or final assessment of our properties. Historic Environment Scotland – Scottish Charity No. SC045925 Principal Office: Longmore House, Salisbury Place, Edinburgh EH9 1SH © Historic Environment Scotland 2018 You may re-use this information (excluding logos and images) free of charge in any format or medium, under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit http://nationalarchives.gov.uk/doc/open- government-licence/version/3/ or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email: [email protected] Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned. Any enquiries regarding this document should be sent to us at: Historic Environment Scotland Longmore House Salisbury Place Edinburgh EH9 1SH +44 (0) 131 668 8600 www.historicenvironment.scot You can download this publication from our website at www.historicenvironment.scot Historic Environment Scotland – Scottish Charity No. SC045925 Principal Office: Longmore House, Salisbury Place, Edinburgh EH9 1SH CAIRN OF MEMSIE BRIEF DESCRIPTION The Cairn of Memsie stands about 4.5km SSW of Fraserburgh in agricultural land. It is a splendid and well-preserved example of a large round burial cairn built in latter half of the 3rd millennium BC, and was once accompanied by two other large burial cairns and many smaller cairns. -

Banffshire and Buchan Coast Polling Scheme
Polling Station Number Constituency Polling Place Name Polling Place Address Polling District Code Ballot Box Number Eligible electors Vote in person Vote by post BBC01 Banffshire and Buchan Coast DESTINY CHURCH AND COMMUNITY HALL THE SQUARE, PORTSOY, BANFF, AB45 2NX BB0101 BBC01 1342 987 355 BBC02 Banffshire and Buchan Coast FORDYCE COMMUNITY HALL EAST CHURCH STREET, FORDYCE, BANFF, AB45 2SL BB0102 BBC02 642 471 171 BBC03 Banffshire and Buchan Coast WHITEHILLS PUBLIC HALL 4 REIDHAVEN STREET, WHITEHILLS, BANFF, AB45 2NJ BB0103 BBC03 1239 1005 234 BBC04 Banffshire and Buchan Coast ST MARY'S HALL BANFF PARISH CHURCH, HIGH STREET, BANFF, AB45 1AE BBC04 BBC05 Banffshire and Buchan Coast ST MARY'S HALL BANFF PARISH CHURCH, HIGH STREET, BANFF, AB45 1AE BBC05 BBC06 Banffshire and Buchan Coast ST MARY'S HALL BANFF PARISH CHURCH, HIGH STREET, BANFF, AB45 1AE BB0104 BBC06 3230 2478 752 BBC07 Banffshire and Buchan Coast WRI HALL HILTON HILTON CROSSROADS, BANFF, AB45 3AQ BB0105 BBC07 376 292 84 BBC08 Banffshire and Buchan Coast ALVAH PARISH HALL LINHEAD, ALVAH, BANFF, AB45 3XB BB0106 BBC08 188 141 47 BBC09 Banffshire and Buchan Coast HAY MEMORIAL HALL 19 MID STREET, CORNHILL, BANFF, AB45 2ES BB0107 BBC09 214 169 45 BBC10 Banffshire and Buchan Coast ABERCHIRDER COMMUNITY PAVILION PARKVIEW, ABERCHIRDER, AB54 7SW BBC10 BBC11 Banffshire and Buchan Coast ABERCHIRDER COMMUNITY PAVILION PARKVIEW, ABERCHIRDER, AB54 7SW BB0108 BBC11 1466 1163 303 BBC12 Banffshire and Buchan Coast FORGLEN PARISH CHURCH HALL FORGLEN, TURRIFF, AB53 4JL BB0109 BBC12 250 216 34 -

Ritchie Road
Ritchie Road 5 Rosehearty, Fraserburgh, AB43 7NY Ritchie Road 5 Rosehearty, Fraserburgh, AB43 7NY Located within the coastal village of Rosehearty, we are delighted to offer to the market this substantial five bedroom executive detached family dwelling house situated on a large plot with fabulous views over the sea. The property was architecturally designed in 1997 and built by the current owners in 1998 with quality fixtures and fittings throughout. The property would serve as an excellent family home as it is located in a safe and quiet cul-de-sac. The accommodation comprises:- The ground floor: An expansive reception hallway providing access to the staircase with a large walk in cupboard below as well as an additional storage cupboard. A well proportioned lounge with bay window is currently being used as a games room. There is also a bright and airy sun room with 180 degree views overlooking the garden with excellent sea views with French doors leading outside. The ground floor bathroom has split level four piece bathroom suit comprises of corner bath, single shower cubicle with mains shower over, and wash hand basin and WC. Open plan dining kitchen, dining room and family room. The kitchen has large bay windows overlooking the rear garden and sea and is fitted with solid wood base and wall mounted units with complimenting worktops, sink and tiled splashback. Integrated ceramic hob with extractor hood, double oven and American fridge freezer. Large dining area leading to the family area with patio doors leading to the rear garden. The utility room is fitted with cream base and wall mounted units, stainless steel sink, under counter washing machine and tumble dryer, external door to the garden and door providing access to the double garage. -

Cottonhill Quarry to Bodychell Quarry
The institute of quarrying Quarry Trails SCOTLAND | ENGLAND | WALES | N.Ireland The Institute of Quarrying From Cottonhill Quarry to Bodychell Quarry Approximate journey time: 1 hourS 41 MINUTES Distance: 20.2 miles QuarrIES Fact file: Address: Address: Macduff, Banff, Aberdeenshire Memsie, Fraserburgh, Aberdeenshire, AB43 7DB (57.664583° -2.4642653°) (57.659841° -2.0805119°) Operator Name: Operator Name: Lovie Ltd Lovie Ltd Planning Region: Planning Region: Scotland Scotland Commodity Produce: Commodity Produce: Igneous & Metamorphic Rock Sand & Gravel lithostratigraphy: lithostratigraphy: Macduff Formation (Macduff Slates) Glaciofluvial Sheet Deposits Age: Age: Neoproterozoic Quaternary www.quarrying.org The Institute of Quarrying Route planner Distance to directions travel Start at Cottonhill Quarry Macduff, Banff, Aberdeenshire 0.0 mi (57.664583° -2.4642653°) 0.2 mi Head south-west towards B9031 0.8 mi Turn left onto B9031 0.7 mi Turn right 17.9 mi Turn left onto A98 0.7 mi Turn right onto B9032 Arrive at Bodychell Quarry Memsie, Fraserburgh, Aberdeenshire, AB43 7DB 0.0 mi (57.659841° -2.0805119°) www.quarrying.org The Institute of Quarrying Safety Advice Please ensure you do not enter onto any quarry site. Ensure follow all road markings and are aware of your surroundings. Wear appropriate clothing and be prepared for changing weather conditions. Only undertake the route if it is within your cycling and fitness capability and ensure you schedule in refreshment breaks in along the way. Check all of your equipment is in good condition. Environmental conditions can change the nature of the trails within a short space of time, you should only continue if safe to do so. -

Fraserburgh Town Profile
From mountain to sea What’s Happening in…. Aberdeenshire’s Towns Fraserburgh August 2019 A publication by the Planning Information and Delivery Team Web: Aberdeenshire Statistics Contact: [email protected] 1 | P a g e August 2018 What's Happening in… Aberdeenshire's Settlements Settlement Average 18 Settlement Fraserburgh YES Please note the settlement you have selected does not have a defined boundary. YES Therefore all figures provided relate to the entire local data zone/s YES 1. Locality Fraserburgh Aberdeenshire (Total number of each locality type) Administrative area Banff & Buchan 6 Civil Parish Fraserburgh 105 Fraserburgh North Primary/ Fraserburgh School Catchment Primary South Park Primary/ St Andrews 152 Primary/ Lochpots School Catchment Secondary Fraserburgh Academy 17 Community Council Fraserburgh 71 Multi-member Ward Fraserburgh and District 19 Scottish Parliamentary Constituency Banffshire and Buchan Coast 3 UK Parliamentary Constituency Banff and Buchan 3 Housing Market Area Rural 2 Travel to Work Area Fraserburgh 4 Urban rural 8 fold classification Other Urban Areas 7 (no large urban centres) Is settlement in the Local Development Plan? Yes 163 Scottish Government Settlement Yes 60 No of Data zones with make up settlement 18 340 Data zones Postcodes which make up settlement 294 9,431 2. Demographics Fraserburgh Aberdeenshire Population 2016 Estimates Population 2018 Estimates Total Population by settlement 13,180 261,470 a) Under 16 2,381 49,033 i. 16-64 8,289 162,638 ii Over 65s 2,510 49,799 ii % Working -

Christmas Classic Thainstone
Web Catalogue For the Christmas Classic Texel In-Lamb Sale of 143 Pedigree In Lamb Texel Females at Thainstone on Monday, 30th November Sale: 5pm Further details Aberdeen & Northern Marts Tel: 01467 623715 INDEX Prefix Lot Number Name ALEXANDER, E, AUCHENBREDDIE FARM, INSCH, BREDDIE'S F64-73 ABERDEENSHIRE, AB52 6LY BRADLEY, JAMES, CLASHINDARROCH COTTAGE, GARTLY, TILLYMINATE F115-116 HUNTLY, ABERDEENSHIRE, AB54 4QS BUCHAN, GAVIN, WYREEMA, CLINTERTY FARM, NEW PENNAN F96-99 ABERDOUR, ABERDEENSHIRE, AB43 6HS BUCHAN Jr, BRIAN, WYREEMA, CLINTERTY FARM, NEW CLINTERTY F89-95 ABERDOUR, FRASERBURGH, ABERDEENSHIRE, AB43 6HS HOWIE, A & G, WEST KNOCK, STUARTFIELD, PETERHEAD, KNOCK F46-53 ABERDEENSHIRE, AB42 8DJ HUNTER, HELEN, BRAEHEAD, BAINSHOLE, HUNTLY, FOUDLAND F125-126 ABERDEENSHIRE, AB54 6AS IMLAH, PATRICIA, 2 WOOD COTTAGES, KINGSEAT, BENNACHIE F16-19, NEWMACHAR, ABERDEENSHIRE, AB21 0UE F127-130 INNES & SONS, JAMES, DUNSCROFT, HUNTLY, STRATHBOGIE F1-2, F54-60 ABERDEENSHIRE, AB54 4SA KNOX, WILLIAM J, MID HADDO, FYVIE, TURRIFF, HADDO F26-35 ABERDEENSHIRE, AB53 8LB LEE, A C, FEURDIES, MEMSIE, FRASERBURGH, FORDAFOURIE F3-5, F20-25 ABERDEENSHIRE, AB43 7UD LEEK, DAVID, ROWANHILL FARM, KININMONTH, ROWANHILL F100-108 PETERHEAD, ABERDEENSHIRE, AB42 4JG LEGGAT, MICHAEL, CAIRNTON FARM, FORGUE, HUNTLY, FOREMAN HILL F61-63 ABERDEENSHIRE, AB54 6BL MCRAE, A & H, NEWTONHILL, CLATT, HUNTLY, NEWTONHILL F117, F124 ABERDEENSHIRE, AB54 4PL MORRISON, GRAHAM A S, INCHBRUICH FARM, CORNHILL, DEVERONVALE F74-83 BANFF, ABERDEENSHIRE, AB45 2HA MUTCH, EDWARD, BURNSIDE, SOUTH -

Sponsors Rtn 153: the Towns, the Villages
153 ROUTE INVENTORY >>> @ride_the north rtn.ridethenorth www.ride-the-north.co.uk SPONSORS RTN 153: THE TOWNS, THE VILLAGES & THE ROUTES RTN Routes are categorised by geography. Routes153 which begin in Aberdeen City, in North Aberdeenshire (broadly north of the River Don), in South Aberdeenshire and in Moray Speyside. The entire network is created trying to link towns and villages that are roughly 15 miles apart and ACROSS while the average route will be approximately 15 miles, the routes range from 5 miles to 25 miles. Each route has been allocated a points value that reflects it’s length, total ascent and any particularly tough hills to be climbed. Individual routes vary from 2 points for short (or almost entirely downhill) to 10 points for the most challenging. ROUTE INVENTORY OR DAYS LOSSIEMOUTH GARMOUTH CULLEN FRASERBURGH BANFF ELGIN FORRES 7, 4 2 STRICHEN ABERCHIRDER KEITH TURRIFF PETERHEAD ARCHIESTOWN DUFFTOWN HUNTLY FYVIE RHYNIE ELLON GRANTOWN INSCH INVERURIE TOMINTOUL ALFORD STRATHDON ABERDEEN WESTHILL BANCHORY ABOYNE BALLATER BRAEMAR STONEHAVEN GLENSHEE FETTERCAIRN INVERBERVIE NORTH ABERDEEN ABERDEENSHIRE/ DEPARTING CITY >>> BANFFSHIRE COAST >>> ABERDEEN CITY: ABERCHIRDER: SEGMENT DISTANCE ELEVATION GAIN POINTS COMPLETE/DATE SEGMENT DISTANCE ELEVATION GAIN POINTS COMPLETE/DATE Aberdeen to Banchory (N Deeside route) 20.5 miles 1,089 ft climbing 6 Aberchirder to Banff 11.6 miles 630 ft climbing 3 Add Link to Segment: Add Link to Segment: Aberdeen to Banchory (S Deeside route) 22 miles 1,594 ft climbing 7 Aberchirder to Huntly -

The Coast; the Persistent Influence of the Sea Dominates This Landscape Character Type
Landscape Character Area: Cliffs of the North and South East coasts Landscape character type: The Coast; the persistent influence of the sea dominates this landscape character type. The landscape fluctuates between sandy beaches and dunes, to rocky headlands and sheer cliffs. Overview Along the entirety of the northern shoreline of Banff & Buchan, and on the eastern coast south of Peterhead, the coastal strip is dominated by cliff- edged headlands, frequently fissured and bitten into narrow inlets and, more rarely, hugging sheltered sandy bays. Despite the physical restrictions of this narrow rocky coastline, the overall impression is of an open, large-scale landscape, the wide expanses of sea and sky merging into one at the uninterrupted horizon line. Cliffs of the North and South East Coasts Location: Key Landscape Features Sensitivity This character area is of increased landscape sensitivity due to the characteristics described below. This area is coincident with what was historically identified as an Area of Landscape Significance. Landform High headlands give way to sheer cliffs, pitted by waves and shattering into jagged reefs. Cliff edged headlands are frequently fissured and bitten into by narrow inlets and more rarely hugging sheltered sandy bays such as Cruden and Sandend. South of Peterhead the sea has gnawed the pink granite into a ragged coastline of highly sculpted and fractured cliffs, broken reefs and dramatic features such as the Bullers of Buchan blowhole. The cliffs of the northern coastline are relatively cohesive and form a more defined edge to the headlands compared to those on the east shore. Vegetation Short creeping grasses and occasional wind pruned gorse bushes on cliff faces. -

Coastal Trail and Explore the Delights of This Incredible Part of Bordering Cullen Golf Club, Follow One Project
01 Cullen Beach B1 09 Portsoy Boatshed B1 17 Crovie D1 25 Maggie’s Hoosie, Inverallochy F1 Stroll along the golden sands of Cullen Home to a team of enthusiastic Crovie (pronounced Crivie) is a This is no ordinary step back in time; one of the finest coasts in the world beach and admire the striking natural volunteers with a passion for boat collection of houses appearing to Maggie’s Hoosie has been lovingly rock formation of the Three Kings, building, you are certain of a friendly almost emerge from the crisp North restored to represent the life of the perfect for photo opportunities. The welcome. Come along and work on Sea, sandwiched between water and fisherwoman who lived there, and Did you know that parts of Aberdeenshire’s coastline were rated as one of the most scenic in the world by beach is renowned for its excellent a boat building or woodwork project cliffs. There’s nowhere else on earth her parents and siblings before her. National Geographic magazine? water quality and is ideal for paddling you’ve always dreamed of bringing quite like this enchanting village – it And when we say restored: picture or, for the more adventurous, to fruition, or join the team to lend a truly is a spellbinding place. As well as earthen floors, no electricity or swimming. Play a round of golf at the hand whilst they work on their latest being the best preserved fishing village running water and four walls that Jump in the car and follow the 165-mile signposted Aberdeenshire Coastal Trail and explore the delights of this incredible part of bordering Cullen Golf Club, follow one project.