Drugs Used in Depression Old &
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MDPV Bath Salts Test
One Step Methylenedioxypyrovalerone Drug of Abuse Test MATERIALS Analytical Sensitivity The cut-off concentration of the One Step Methylenedioxypyrovalerone Drug of Abuse Test is determined to be 1,000ng/mL. (Dip Card) Materials Provided: Test was run in 30 replicates with negative urine and standard control at ±25% cut-off and ±50% cut-off concentration levels. Test results ● Dip cards are summarized below. For Forensic Use Only ● Desiccants ● Package insert Test Result INTENDED USE Percent of Cut-off n Materials Required But Not Provided: Methylenedioxypyrovalerone Concentration in ng/mL The One Step Methylenedioxypyrovalerone Drug of Abuse Test is a lateral flow chromatographic immunoassay for the ● Specimen collection container Negative Positive qualitative detection of Methylenedioxypyrovalerone (MDPV) in human urine specimen at the cut-off level of 1,000ng/mL. This ● Disposable gloves 0% Cut-off assay is intended for forensic use only. ● Timer 30 30 0 This assay provides only a preliminary qualitative test result. A more specific confirmatory reference method, such as Liquid (No Drug Present) chromatogra -50% Cut-off phy tandem mass spectrometry (LC/MS/MS) or gas chromatography/mass spectrometry (GC/MS) must be use in INSTRUCTIONS FOR USE] 30 30 0 order to obtain a confirmed analytical result. (500ng/mL) 1) Remove the dip card from the foil pouch. -25% Cut-off 30 30 0 BACKGROUND 2) Remove the cap from the dip card. Label the device with patient or control identifications. (750ng/mL) 3) Immerse the absorbent tip into the urine sample for 5 seconds. Urine sample should not touch the plastic device. Cut-off ‘Bath salts’, a form of designer drugs, also promoted as ‘plant food’ or ‘research chemicals’, is sold mainly in head shops, on 4) Replace the cap over the absorbent tip and lay the dip card on a clean, flat, and non-absorptive surface. -

Octopamine and Tyramine Regulate the Activity of Reproductive Visceral Muscles in the Adult Female Blood-Feeding Bug, Rhodnius Prolixus Sam Hana* and Angela B
© 2017. Published by The Company of Biologists Ltd | Journal of Experimental Biology (2017) 220, 1830-1836 doi:10.1242/jeb.156307 RESEARCH ARTICLE Octopamine and tyramine regulate the activity of reproductive visceral muscles in the adult female blood-feeding bug, Rhodnius prolixus Sam Hana* and Angela B. Lange ABSTRACT Monastirioti et al., 1996). Octopamine and tyramine signal via The role of octopamine and tyramine in regulating spontaneous G-protein coupled receptors (GPCRs), leading to changes in second contractions of reproductive tissues was examined in the messenger levels. The recently updated receptor classification α β female Rhodnius prolixus. Octopamine decreased the amplitude of (Farooqui, 2012) divides the receptors into Oct -R, Oct -Rs β β β spontaneous contractions of the oviducts and reduced RhoprFIRFa- (Oct 1-R, Oct 2-R, Oct 3-R), TYR1-R and TYR2-R. In general, β α induced contractions in a dose-dependent manner, whereas tyramine Oct -Rs lead to elevation of cAMP while Oct -R and TYR-Rs lead to 2+ only reduced the RhoprFIRFa-induced contractions. Both octopamine an increase in Ca (Farooqui, 2012). and tyramine decreased the frequency of spontaneous bursal The movement of eggs in the reproductive system of contractions and completely abolished the contractions at Rhodnius prolixus starts at the ovaries, the site of egg maturation. 5×10−7 mol l−1 and above. Phentolamine, an octopamine receptor Upon ovulation, mature eggs are released into the oviducts antagonist, attenuated the inhibition induced by octopamine on the (Wigglesworth, 1942). Eggs are then guided, via oviductal oviducts and the bursa. Octopamine also increased the levels of peristaltic and phasic contractions, to the common oviduct, where cAMP in the oviducts, and this effect was blocked by phentolamine. -

Can Hepatic Coma Be Caused by a Reduction of Brain Noradrenaline Or Dopamine?
Gut: first published as 10.1136/gut.18.9.688 on 1 September 1977. Downloaded from Gut, 1977, 18, 688-691 Can hepatic coma be caused by a reduction of brain noradrenaline or dopamine? L. ZIEVE AND R. L. OLSEN From the Department ofMedicine, Minneapolis Veterans Hospital, University of Minnesota, Minneapolis, and Department of Chemistry, Hamline University, St. Paul, Minnesota, USA SUMMARY Intraventricular infusions of octopamine which raised brain octopamine concentrations more than 20 000-fold resulted in reductions in brain noradrenaline and dopamine by as much as 90% without affecting the alertness or activity of normal rats. As this reduction of brain catechol- amines is much greater than any reported in hepatic coma, we do not believe that values observed in experimental hepatic failure have aetiological significance for the encephalopathy that ensues. Though catecholaminergic nerve terminals represent dopamine and noradrenaline had no discernible only a small proportion of brain synapses (Snyder et effect on the state of alertness of the animals. al., 1973), the reduction in brain dopamine or nor- adrenaline by the accumulation of false neuro- Methods transmitterssuch as octopamine or of aromaticamino acids such as phenylalanine or tyrosine has been ANIMALS suggested as a cause of hepatic coma (Fischer and Male Sprague-Dawley rats weighing between 300 and Baldessarini, 1971; Dodsworth et al., 1974; Fischer 350 were g prepared by the method of Peterson and http://gut.bmj.com/ and Baldessarini, 1975; Munro et al., 1975). The Sparber (1974) for intraventricular infusions of following data have been cited in support of this octopamine. Rats of 250-400 g were used as controls. -

Neuroenhancement in Healthy Adults, Part I: Pharmaceutical
l Rese ca arc ni h li & C f B o i o l e Journal of a t h n Fond et al., J Clinic Res Bioeth 2015, 6:2 r i c u s o J DOI: 10.4172/2155-9627.1000213 ISSN: 2155-9627 Clinical Research & Bioethics Review Article Open Access Neuroenhancement in Healthy Adults, Part I: Pharmaceutical Cognitive Enhancement: A Systematic Review Fond G1,2*, Micoulaud-Franchi JA3, Macgregor A2, Richieri R3,4, Miot S5,6, Lopez R2, Abbar M7, Lancon C3 and Repantis D8 1Université Paris Est-Créteil, Psychiatry and Addiction Pole University Hospitals Henri Mondor, Inserm U955, Eq 15 Psychiatric Genetics, DHU Pe-psy, FondaMental Foundation, Scientific Cooperation Foundation Mental Health, National Network of Schizophrenia Expert Centers, F-94000, France 2Inserm 1061, University Psychiatry Service, University of Montpellier 1, CHU Montpellier F-34000, France 3POLE Academic Psychiatry, CHU Sainte-Marguerite, F-13274 Marseille, Cedex 09, France 4 Public Health Laboratory, Faculty of Medicine, EA 3279, F-13385 Marseille, Cedex 05, France 5Inserm U1061, Idiopathic Hypersomnia Narcolepsy National Reference Centre, Unit of sleep disorders, University of Montpellier 1, CHU Montpellier F-34000, Paris, France 6Inserm U952, CNRS UMR 7224, Pierre and Marie Curie University, F-75000, Paris, France 7CHU Carémeau, University of Nîmes, Nîmes, F-31000, France 8Department of Psychiatry, Charité-Universitätsmedizin Berlin, Campus Benjamin Franklin, Eschenallee 3, 14050 Berlin, Germany *Corresponding author: Dr. Guillaume Fond, Pole de Psychiatrie, Hôpital A. Chenevier, 40 rue de Mesly, Créteil F-94010, France, Tel: (33)178682372; Fax: (33)178682381; E-mail: [email protected] Received date: January 06, 2015, Accepted date: February 23, 2015, Published date: February 28, 2015 Copyright: © 2015 Fond G, et al. -

Octopamine Regulates Sleep Indrosophilathrough Protein Kinase A-Dependent Mechanisms
The Journal of Neuroscience, September 17, 2008 • 28(38):9377–9385 • 9377 Behavioral/Systems/Cognitive Octopamine Regulates Sleep in Drosophila through Protein Kinase A-Dependent Mechanisms Amanda Crocker and Amita Sehgal Department of Neuroscience, Howard Hughes Medical Institute, University of Pennsylvania, Philadelphia, Pennsylvania 19104 Sleep is a fundamental process, but its regulation and function are still not well understood. The Drosophila model for sleep provides a powerful system to address the genetic and molecular mechanisms underlying sleep and wakefulness. Here we show that a Drosophila biogenic amine, octopamine, is a potent wake-promoting signal. Mutations in the octopamine biosynthesis pathway produced a pheno- type of increased sleep, which was restored to wild-type levels by pharmacological treatment with octopamine. Moreover, electrical silencing of octopamine-producing cells decreased wakefulness, whereas excitation of these neurons promoted wakefulness. Because protein kinase A (PKA) is a putative target of octopamine signaling and is also implicated in Drosophila sleep, we investigated its role in the effects of octopamine on sleep. We found that decreased PKA activity in neurons rendered flies insensitive to the wake-promoting effects of octopamine. However, this effect of PKA was not exerted in the mushroom bodies, a site previously associated with PKA action on sleep. These studies identify a novel pathway that regulates sleep in Drosophila. Key words: Drosophila; octopamine; sleep; locomotion; norepinephrine; biogenic amine; arousal Introduction The only arousal-promoting signal identified in Drosophila is Sleep is a core process that spans genetically diverse eukaryotes dopamine (Andretic et al., 2005; Kume et al., 2005). from mammals to arthropods (Tobler, 2005). -

Recent Trends in the Quantification of Biogenic Amines in Biofluids
Journal of Clinical Medicine Review Recent Trends in the Quantification of Biogenic Amines in Biofluids as Biomarkers of Various Disorders: A Review Alina Plenis 1,* , Ilona Ol˛edzka 1 , Piotr Kowalski 1 , Natalia Mi˛ekus 1,2 and Tomasz B ˛aczek 1 1 Department of Pharmaceutical Chemistry, Medical University of Gda´nsk,Hallera 107, 80-416 Gda´nsk, Poland; [email protected] (I.O.); [email protected] (P.K.); [email protected] (N.M.); [email protected] (T.B.) 2 Department of Animal and Human Physiology, Faculty of Biology, University of Gda´nsk,Wita Stwosza 59, 80-308 Gda´nsk,Poland * Correspondence: [email protected]; Fax: +48-58-349-16-35 Received: 4 April 2019; Accepted: 6 May 2019; Published: 9 May 2019 Abstract: Biogenic amines (BAs) are bioactive endogenous compounds which play a significant physiological role in many cell processes like cell proliferation and differentiation, signal transduction and membrane stability. Likewise, they are important in the regulation of body temperature, the increase/decrease of blood pressure or intake of nutrition, as well as in the synthesis of nucleic acids and proteins, hormones and alkaloids. Additionally, it was confirmed that these compounds can be considered as useful biomarkers for the diagnosis, therapy and prognosis of several neuroendocrine and cardiovascular disorders, including neuroendocrine tumours (NET), schizophrenia and Parkinson’s Disease. Due to the fact that BAs are chemically unstable, light-sensitive and possess a high tendency for spontaneous oxidation and decomposition at high pH values, their determination is a real challenge. Moreover, their concentrations in biological matrices are extremely low. -

Traxoprodil, a Selective Antagonist of the NR2B Subunit of the NMDA
Metab Brain Dis (2016) 31:803–814 DOI 10.1007/s11011-016-9810-5 ORIGINAL ARTICLE Traxoprodil, a selective antagonist of the NR2B subunit of the NMDA receptor, potentiates the antidepressant-like effects of certain antidepressant drugs in the forced swim test in mice Ewa Poleszak1 & Weronika Stasiuk 2 & Aleksandra Szopa1 & Elżbieta Wyska3 & Anna Serefko1 & Anna Oniszczuk4 & Sylwia Wośko 1 & Katarzyna Świąder1 & Piotr Wlaź5 Received: 25 November 2015 /Accepted: 17 February 2016 /Published online: 29 February 2016 # The Author(s) 2016. This article is published with open access at Springerlink.com Abstract One of the newest substances, whose antidepres- these changes were not due to the severity of locomotor ac- sant activity was shown is traxoprodil, which is a selective tivity. The observed effect of traxoprodil is only partially as- antagonist of the NR2B subunit of the NMDA receptor. The sociated with serotonergic system and is independent of the main goal of the present study was to evaluate the effect of effect on the 5-HT1A and 5-HT2 serotonin receptors. The re- traxoprodil on animals’ behavior using the forced swim test sults of an attempt to assess the nature of the interaction be- (FST), as well as the effect of traxoprodil (10 mg/kg) on the tween traxoprodil and the tested drugs show that in the case of activity of antidepressants, such as imipramine (15 mg/kg), joint administration of traxoprodil and fluoxetine, imip- fluoxetine (5 mg/kg), escitalopram (2 mg/kg) and reboxetine ramine or escitalopram, there were interactions in the (2.5 mg/kg). Serotonergic lesion and experiment using the pharmacokinetic phase. -

Catecholamines and the Hydroxylation of Tyrosine in Synaptosomes Isolated from Rat Brain (DOPA/Tyramine/Dopamine/Norepinephrine/Octopamine) M
Proc. Nat. Acad. Sci. USA Vol. 68, No. 10, pp. 2370-2373, October 1971 Catecholamines and the Hydroxylation of Tyrosine in Synaptosomes Isolated from Rat Brain (DOPA/tyramine/dopamine/norepinephrine/octopamine) M. KAROBATH Psychiatric Research Laboratories, Massachusetts General Hospital, Boston, Mass. 02114 Communicated by Seymour S. Kety, July 16, 1971 ABSTRACT Tyrosine hydroxylase activity of synapto- removing transmitters from an extraneuronal location at the somes isolated from rat brain was examined. A modified synapse, then incubation of synaptosomes with catechol- tritium-displacement assay was used, which allowed the measurement of tyrosine hydroxylase activity without the amines should inhibit the formation of DOPA from tyrosine. addition of either inhibitors of the metabolism of the The experiments demonstrate that tyrosine hydroxylase hydroxylated products or added exogenous cofactor. The activity is affected by catecholamine uptake. The concentra- enzyme activity was strongly inhibited by the addition of tions required to inhibit the synthesis of catechols are in the exogenous catecholamines and 3,4-dihydroxy-L-phenyl- M. alanine. Aromatic amines other than catechols did not range of 10-7 markedly influence tyrosine hydroxylase activity. These MATERIALS AND METHODS in vitro findings support the hypothesis that synthesis of catecholamines is regulated by a mechanism of end- [3,5-H]HifTyrosine (Tracerlab) was purified by column chro- product inhibition at the tyrosine hydroxylase step. matography. Catechol impurities were absorbed on alumina and tritiated water and anions were removed by Synaptosomes are pinched-off nerve endings with relatively columns (8), by non-neuronal elements (1, 2). They absorption on Dowex-50 resin. Tyrosine was eluted from little contamination Dowex-50 with 25 ml of 4 N HCl; after distillation of the eluate contain the enzymes necessary for the synthesis of dopamine (v/v) from tyrosine (3, 4). -
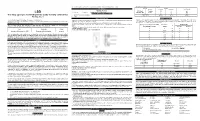
(LSD) Test Dip Card (Urine) • Specimen Collection Container % Agreement 98.8% 99
frozen and stored below -20°C. Frozen specimens should be thawed and mixed before testing. GC/MS. The following results were tabulated: Method GC/MS MATERIALS Total Results Results Positive Negative Materials Provided LSD Rapid Positive 79 1 80 LSD • Test device • Desiccants • Package insert • Urine cups Test Dip card Negative 1 99 100 Materials Required But Not Provided Total Results 80 100 180 One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) • Specimen collection container % Agreement 98.8% 99. % 98.9% • Timer Package Insert DIRECTIONS FOR USE Analytical Sensitivity This Instruction Sheet is for testing of Lysergic acid diethylamide. Allow the test device, and urine specimen to come to room temperature [15-30°C (59-86°F)] prior to testing. A drug-free urine pool was spiked with LSD at the following concentrations: 0 ng/mL, -50%cutoff, -25%cutoff, cutoff, A rapid, one step test for the qualitative detection of Lysergic acid diethylamide and its metabolites in human urine. 1) Remove the test device from the foil pouch. +25%cutoff and +50%cutoff. The result demonstrates >99% accuracy at 50% above and 50% below the cut-off For forensic use only. 2) Remove the cap from the test device. Label the device with patient or control identifications. concentration. The data are summarized below: INTENDED USE 3) Immerse the absorbent tip into the urine sample for 10-15 seconds. Urine sample should not touch the plastic Lysergic acid diethylamide (LSD) Percent of Visual Result The One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) is a lateral flow chromatographic device. -

Amphetamine, 3,4
0026-895X/01/6006-1181–1188$3.00 MOLECULAR PHARMACOLOGY Vol. 60, No. 6 Copyright © 2001 The American Society for Pharmacology and Experimental Therapeutics 1304/951292 Mol Pharmacol 60:1181–1188, 2001 Printed in U.S.A. ACCELERATED COMMUNICATION Amphetamine, 3,4-Methylenedioxymethamphetamine, Lysergic Acid Diethylamide, and Metabolites of the Catecholamine Neurotransmitters Are Agonists of a Rat Trace Amine Receptor JAMES R. BUNZOW, MARK S. SONDERS, SEKSIRI ARTTAMANGKUL, LAURA M. HARRISON, GE ZHANG, DENISE I. QUIGLEY, TRISTAN DARLAND, KATHERINE L. SUCHLAND, SHAILAJA PASUMAMULA, JAMES L. KENNEDY, SUSAN B. OLSON, R. ELLEN MAGENIS, SUSAN G. AMARA, and DAVID K. GRANDY Departments of Physiology & Pharmacology (J.R.B., S.A., L.M.H., G.Z., D.I.Q., T.D., K.L.S., S.P., S.B.O., R.E.M., D.K.G.) and Molecular and Medical Genetics (S.B.O., R.E.M), School of Medicine, the Vollum Institute (M.S.S., S.G.A.), and the Howard Hughes Medical Institute (S.G.A.), Oregon Health & Science University, Portland, Oregon; and Centre for Addiction and Mental Health, University of Toronto, Canada (J.L.K.) Received August 21, 2001; accepted September 28, 2001 This paper is available online at http://molpharm.aspetjournals.org ABSTRACT The trace amine para-tyramine is structurally and functionally re- goline derivatives, adrenergic ligands, and 3-methylated metabo- lated to the amphetamines and the biogenic amine neurotrans- lites of the catecholamine neurotransmitters are also good ago- mitters. It is currently thought that the biological activities elicited nists at the rat trace amine receptor 1 (rTAR1). These results by trace amines such as p-tyramine and the psychostimulant suggest that the trace amines and catecholamine metabolites amphetamines are manifestations of their ability to inhibit the may serve as the endogenous ligands of a novel intercellular clearance of extracellular transmitter and/or stimulate the efflux of signaling system found widely throughout the vertebrate brain and transmitter from intracellular stores. -

Adrenergic-Like Octopamine Receptor Affects Locomotion and Reproduction of Tribolium Castaneum
International Journal of Molecular Sciences Article Knockdown of a β-Adrenergic-Like Octopamine Receptor Affects Locomotion and Reproduction of Tribolium castaneum Li-Sha Zheng 1,2,†, Xiao-Qiang Liu 1,3,†, Ge-Ge Liu 1, Qian-Qiao Huang 1, Jin-Jun Wang 1,2 and Hong-Bo Jiang 1,2,* 1 Key Laboratory of Entomology and Pest Control Engineering, College of Plant Protection, Southwest University, Chongqing 400715, China; [email protected] (L.-S.Z.); [email protected] (X.-Q.L.); [email protected] (G.-G.L.); [email protected] (Q.-Q.H.); [email protected] (J.-J.W.) 2 Academy of Agricultural Sciences, Southwest University, Chongqing 400715, China 3 Laboratory of Integrated Pest Management on Tropical Crops, Environment and Plant Protection Institute, Chinese Academy of Tropical Agriculture Sciences, Ministry of Agriculture, Haikou 570100, China * Correspondence: [email protected]; Tel.: +86-23-6825-0255; Fax: +86-23-6825-1269 † These authors contributed equally to this work. Abstract: The neurohormone octopamine regulates many crucial physiological processes in insects and exerts its activity via typical G-protein coupled receptors. The roles of octopamine receptors in regulating behavior and physiology in Coleoptera (beetles) need better understanding. We used the red flour beetle, Tribolium castaneum, as a model species to study the contribution of the octopamine receptor to behavior and physiology. We cloned the cDNA of a β-adrenergic-like octopamine receptor (TcOctb2R). This was heterologously expressed in human embryonic kidney (HEK) 293 cells and Citation: Zheng, L.-S.; Liu, X.-Q.; was demonstrated to be functional using an in vitro cyclic AMP assay. -

Serotonin (5HT), Fluoxetine, Imipramine and Dopamine Target Distinct 5HT Receptor Signaling to Modulate Caenorhabditis Elegans Egg-Laying Behavior
Copyright © 2005 by the Genetics Society of America DOI: 10.1534/genetics.104.032540 Serotonin (5HT), Fluoxetine, Imipramine and Dopamine Target Distinct 5HT Receptor Signaling to Modulate Caenorhabditis elegans Egg-Laying Behavior Catherine M. Dempsey, Scott M. Mackenzie, Andrew Gargus, Gabriela Blanco and Ji Ying Sze1 Department of Anatomy and Neurobiology, College of Medicine, University of California, Irvine, California 92697-4040 Manuscript received June 18, 2004 Accepted for publication November 22, 2004 ABSTRACT Drugs that target the serotonergic system are the most commonly prescribed therapeutic agents and are used for treatment of a wide range of behavioral and neurological disorders. However, the mechanism of the drug action remain a conjecture. Here, we dissect the genetic targets of serotonin (5HT), the selective 5HT reuptake inhibitor (SSRI) fluoxetine (Prozac), the tricyclic antidepressant imipramine, and dopamine. Using the well-established serotonergic response in C. elegans egg-laying behavior as a paradigm, we show that action of fluoxetine and imipramine at the 5HT reuptake transporter (SERT) and at 5HT receptors are separable mechanisms. Even mutants completely lacking 5HT or SERT can partially respond to fluoxetine and imipramine. Furthermore, distinct mechanisms for each drug can be recognized to mediate these responses. Deletion of SER-1, a 5HT1 receptor, abolishes the response to 5HT but has only a minor effect on the response to imipramine and no effect on the response to fluoxetine. In contrast, deletion of SER-4, a 5HT2 receptor, confers significant resistance to imipramine while leaving the responses to 5HT or fluoxetine intact. Further, fluoxetine can stimulate egg laying via the Gq protein EGL-30, independent of SER-1, SER-4, or 5HT.