Comparing Circulating Tumor Cell Counts with Dynamic Tumor Size Changes As Predictor of Overall Survival - a Quantitative Modeling Framework
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cable Channels
HD Channel Lineup for: Tampa Bay Area: Manatee County Displaying 459 channels. Ch. Network Ch. Network Ch. Network 3 WEDU - PBS 154 BET Jams 221 Cinemax - E 1003 WEDU - PBS 96 BET Soul 226 Cinemáx - E 605 WEDU - PBS Encore 809 BTN 61 Comedy Central 8 WFLA - NBC 820 BTN - Extra1 95 Community Programming 1008 WFLA - NBC 821 BTN - Extra2 142 Cooking Channel 11 WFTS - ABC 197 BYUtv 170 Crime & Investigation 1011 WFTS - ABC 174 Baby First TV 949 Cubaplay 10 WTSP - CBS 974 BabyFirstTV (SAP) 136 DIY Network 1010 WTSP - CBS 975 BabyTV (SAP) 524 DWLS Filipino Audio 13 WTVT - FOX 961 Bandamax 525 DZBB Filipino Audio 1013 WTVT - FOX 9 Bay News 9 171 Daystar 16 WUSF - PBS 831 BeIN SPORTS 979 De Película 1016 WUSF - PBS 913 BeIN SPORTS Español 980 De Película Clásico 617 WUSF - PBS Kids 127 Bloomberg Television 108 Destination America 7 WWSB - ABC 124 Boomerang 34 Discovery Channel 1007 WWSB - ABC 51 Bravo 922 Discovery Familia 227 5 StarMAX - E 14 C-SPAN 102 Discovery Family 48 A&E 176 C-SPAN2 114 Discovery Life Channel 567 ABP News 177 C-SPAN3 925 Discovery en Español 64 AMC 529 C1R (Russia) 40 Disney Channel 501 ART Cable 139 CBS Sports Network 179 Disney Junior 180 ASPiRE TV 590 CCTV-4 122 Disney XD 1303 AXS TV 45 CMT 923 Disney XD 223 ActionMAX - E 42 CNBC 70 E! 103 American Heroes Channel 141 CNBC World 364 EPIX 35 Animal Planet 29 CNN 365 EPIX 2 - E 557 Ant1 Greek 904 CNN en Español 367 EPIX Drive-In 960 Antena 3 Internacional 532 CTC Russian Network 1366 EPIX HITS 972 Atres Series 906 Canal Sur 27 ESPN 986 AyM Sports 936 Caracol 810 ESPN Classic 75 BBC America 58 Cartoon Network 1791 ESPN College Extra 1278 BBC America 970 Cartoon Network (SAP) 153 ESPN Deportes 123 BBC World News 907 CentroamericaTV 1196 ESPN Goal Line/Bases Loaded 71 BET 912 Cine Mexicano 28 ESPN2 107 BET HER 928 Cinelatino 150 ESPNEWS Ch. -

Apo-Nid63005.Pdf
AUSTRALIAN BROADCASTING TRIBUNAL ANNUAL REPORT 1991-92 Australian Broadcasting Tribunal Sydney 1992 ©Commonwealth of Australia ISSN 0728-8883 Design by Media and Public Relations Branch, Australian Broadcasting Tribunal. Printed in Australia by Pirie Printers Sales Pty Ltd, Fyshwick, A.CT. 11 Contents 1. MEMBERSIDP OF THE TRIBUNAL 1 2. THE YEAR IN REVIEW 7 3. POWERS AND FUNCTIONS OF THE TRIBUNAL 13 Responsible Minister 16 4. LICENSING 17 Number and Type of Licences on Issue 19 Grant of Limited Licences 20 Commercial Radio Licence Grant Inquiries 21 Supplementary Radio Grant Inquiries 23 Joined Supplementary /Independent Radio Grant Inquiries 24 Remote Licences 26 Public Radio Licence Grants 26 Renewal of Licences with Conditions or Licensee Undertaking 30 Revocation/Suspension/Conditions Inquiries 32 Allocation of Call Signs 37 5. OWNERSHIP AND CONTROL 39 Applications and Notices Received 41 Most Significant Inquiries 41 Unfinished Inquiries 47 Contraventions Amounting To Offences 49 Licence Transfers 49 Uncompleted Inquiries 50 Operation of Service by Other than Licensee 50 Registered Lender and Loan Interest Inquiries 50 6. PROGRAM AND ADVERTISING STANDARDS 51 Program and Advertising Standards 53 Australian Content 54 Compliance with Australian Content Television Standard 55 Children's Television Standards 55 Compliance with Children's Standards 58 Comments and Complaints 59 Broadcasting of Political Matter 60 Research 61 iii 7. PROGRAMS - PUBLIC INQUIRIES 63 Public Inquiries 65 Classification of Television Programs 65 Foreign Content In Television Advertisements 67 Advertising Time On Television 68 Film And Television Co-productions 70 Australian Documentary Programs 71 Cigarette Advertising During The 1990 Grand Prix 72 Test Market Provisions For Foreign Television Advertisements 72 Public Radio Sponsorship Announcements 73 Teenage Mutant Ninja Turtles 74 John Laws - Comments About Aborigines 75 Anti-Discrimination Standards 75 Accuracy & Fairness in Current Affairs 76 Religious Broadcasts 77 Review of Classification Children's Television Programs 78 8. -

Alpha ELT Listing
Lienholder Name Lienholder Address City State Zip ELT ID 1ST ADVANTAGE FCU PO BX 2116 NEWPORT NEWS VA 23609 CFW 1ST COMMAND BK PO BX 901041 FORT WORTH TX 76101 FXQ 1ST FNCL BK USA 47 SHERMAN HILL RD WOODBURY CT 06798 GVY 1ST LIBERTY FCU PO BX 5002 GREAT FALLS MT 59403 ESY 1ST NORTHERN CA CU 1111 PINE ST MARTINEZ CA 94553 EUZ 1ST NORTHERN CR U 230 W MONROE ST STE 2850 CHICAGO IL 60606 GVK 1ST RESOURCE CU 47 W OXMOOR RD BIRMINGHAM AL 35209 DYW 1ST SECURITY BK WA PO BX 97000 LYNNWOOD WA 98046 FTK 1ST UNITED SVCS CU 5901 GIBRALTAR DR PLEASANTON CA 94588 W95 1ST VALLEY CU 401 W SECOND ST SN BERNRDNO CA 92401 K31 360 EQUIP FIN LLC 300 BEARDSLEY LN STE D201 AUSTIN TX 78746 DJH 360 FCU PO BX 273 WINDSOR LOCKS CT 06096 DBG 4FRONT CU PO BX 795 TRAVERSE CITY MI 49685 FBU 777 EQUIPMENT FIN LLC 600 BRICKELL AVE FL 19 MIAMI FL 33131 FYD A C AUTOPAY PO BX 40409 DENVER CO 80204 CWX A L FNCL CORP PO BX 11907 SANTA ANA CA 92711 J68 A L FNCL CORP PO BX 51466 ONTARIO CA 91761 J90 A L FNCL CORP PO BX 255128 SACRAMENTO CA 95865 J93 A L FNCL CORP PO BX 28248 FRESNO CA 93729 J95 A PLUS FCU PO BX 14867 AUSTIN TX 78761 AYV A PLUS LOANS 500 3RD ST W SACRAMENTO CA 95605 GCC A/M FNCL PO BX 1474 CLOVIS CA 93613 A94 AAA FCU PO BX 3788 SOUTH BEND IN 46619 CSM AAC CU 177 WILSON AVE NW GRAND RAPIDS MI 49534 GET AAFCU PO BX 619001 MD2100 DFW AIRPORT TX 75261 A90 ABLE INC 503 COLORADO ST AUSTIN TX 78701 CVD ABNB FCU 830 GREENBRIER CIR CHESAPEAKE VA 23320 CXE ABOUND FCU PO BX 900 RADCLIFF KY 40159 GKB ACADEMY BANK NA PO BX 26458 KANSAS CITY MO 64196 ATF ACCENTRA CU 400 4TH -

Project ASPIRE: Empowering Families of Children Wi H H I L with Hearing Loss
Project ASPIRE: Empowering Families of Children Wit h Hear ing Loss Sophie Shay, MSII Lyra Repplinger, M.S. Dana L. Suskind, M.D. AdAgenda { Pro jec t ASPIRE { Exploring Health Disparities { Developing A Best Practices Curriculum { The Modules { Module Components { The Dream { Research Protocol/Pilot Testing { Q & A What i s P roj ec t ASPIRE? { Pro ject ASPIRE: Achiev ing Superior Parental Involvement for Rehabilitative Excellence z A comprehensive interactive multimedia intervention z Imparts knowledge and skills for parents of economically disadvantaged children to aid in their children’s listening, language and spppeech development after im plantation z Empowers parents Impetus for the Program: IltOtImplant Outcome Di Diitisparities { Econom ica lly disa dvan tage d imp lan t recip ien ts have less favorable outcomes than their more affluent peers (Witkin, 2005;Easterbrooks, O’Rourke & Todd, 2000) { Factors in Outcome Disparities z Access and Availability of Habilitation z Inadequate Parental Skills to support their child’s language development (Geers, 2006; Moog & Geers, 2003, Easterbrooks, O’Rourke & Todd, 2000) What A re H ealth Dispar ities ? { Unequa l bur den in disease morbidity and morta lity rates experienced by ethnic/racial groups as compared to the dominant group { Widening disparity in the United States affecting all aspects of healthcare { Socioeconomic status (SES): the most frequently cited, and most consistent, contributor z SES=income, education, wealth or a combination { Healthy People 2010 has designated the elimination of health disparities as one of its essential goal z Improved hearing health of the nation through prevention, early detection, treatment and rehabilitation z Successful Implantation and Habilitation of Children Makes good economic sense! Children an d Pover ty BELOW 100% BELOW 150% RACE POVERTY** POVERTY** White 13. -
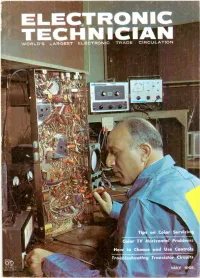
Electronics-Technici
WORLD'S LARGEST ELECTRONIC TRADE CIRCULATION Tips on Color Servicir Color TV Horizontal Problems How to Choose and Use Controls Troubleshooting Transistor Circuits MAY 1965 ENirr The quality goes in before the name goes on FOR THE FINEST COLOR AND UHF RECEPTION INSTALL ZENITH QUALITY ANTENNAS ... to assure finer performance in difficult reception areas! More color TV sets and new UHF stations mean new antenna installation jobs for you. Proper installation with antennas of Zenith quality is most important because of the sensi tivity of color and JHF signals. ZENITH ALL -CHANNEL VHF/UHF/FM AND FM -STEREO LOG -PERIODIC ANTENNAS The unusually broad bandwidth of the new Zenith VHF/UHF/FM and FM -Stereo log -periodic resonant V -dipole arrays pulls in all frequencies from 50 to 900 mc-television channels 2 to 83 /\' plus FM radio. The multi -mode operation pro- vides nigh gain and good rejection of ghosts. These frequency independent antennas, devel- , oped // by the research laboratories at the University of Illinois, are designed according to a geometrically derived logarithmic -periodic formula used in satellite telemetry. ZENITH QUALITY HEAVY-DUTY ZENITH QUALITY ANTENNA ROTORS WIRE AND CABLE Zenith quality antenna rotors are Zenith features a full line of quality heavy-duty throughout-with rugged packaged wire and cable. Also espe- motor and die-cast aluminum hous- cially designed UHF transmission ing. Turns a 150-Ib. antenna 360 de- wires, sold only by Zenith. Zenith grees in 45 seconds. The weather- wire and cable is engineered for proof bell casting protects the unit greater reception and longer life, from the elements. -

Channel Lineup
† 52 VH1 120 The Hub 186 VH1 Classics 372 MoreMAX Freehold/Lakewood/ † † 53 MTV 121 Disney XD 187 CMT 373 ThrillerMAX † Jackson/Millstone 54 BET 122 Nicktoons TV 188 MTV Hits 374 MovieMAX February 2014 55 MTV2 123 Nick Jr. 189 VH1 Soul 375 MAX Latino † 56 fuse 124 Teen Nick 190 FX Movie Channel 376 5 StarMAX 2 WCBS (2) New York (CBS) † 57 Animal Planet 125 Boomerang 191 Hallmark Channel 377 OuterMAX 3 WPXN (31) New York (ION) † † † 58 truTV 126 Disney Junior 192 SundanceTV 378 Cinemax West 4 WNBC (4) New York (NBC) † † † 59 CNN Headline News 127 Sprout 193 Hallmark Movie Channel 379 TMC On Demand 5 WNYW (5) New York (FOX) † 60 SportsNet New York 131 Kids Thirteen 195 MTV Tr3s 380 TMC Xtra 6 WPVI (6) Philadelphia (ABC) † 61 News 12 Traffic & Weather 132 WLIW World 196 FOX Deportes 381 TMC West 7 WABC (7) New York (ABC) 2† 62 The Weather Channel 133 WLIW Create 197 mun 382 TMC Xtra West 8 NJTV † 64 Esquire Network 134 Trinity Broadcasting Network 198 Galavisión 400-413 Optimum Sports & 9 My9 New York (MNT-WWOR) 66 C-SPAN 2 135 EWTN 199 Vme Entertainment Pak 10 WCAU (10) Philadelphia (NBC) † 67 Syfy 136 Daystar 300 HBO On Demand 414 Sports Overflow 11 WPIX (11) New York (CW) † † 69 FOX Sports 1 137 Telecare 301 HBO Signature 415-429 Seasonal Sports Packages 12 News 12 New Jersey 70 YES Network 138 Shalom TV 302 HBO Family 430 NBA TV 13 WNET (13) New York (PBS) † 71 MSG 140 ESPN Classic 303 HBO Comedy 432-450 Seasonal Sports Packages 14 Optimum Channel Channel Lineup Channel 72 MSG Plus 141 ESPNEWS† 304 HBO Zone 460 Sports Overflow 2 15 MiND -

Evidence-Based Prevention Programs and Proven Drug Use Outcomes
Evidence-based Prevention Programs and Proven Drug Use Outcomes Program Name Setting/Model Target Pop. Substance use outcomes Communities That Community-based / Data driven needs Any community Students were 32% less likely to have Care (CTC) assessment and program selection initiated alcohol use and 33% less strategy implemented by community likely to have initiated cigarette use coalitions. when compared with control group1 Big Brothers Big Community-based / Mentoring Youth aged Less likely to initiate drug use1 Sisters (BBBS) 6-18 Project Toward No School-based / Universal Prevention High school Lower prevalence of past 30-day hard Drug Abuse (TND) builds coping skills and ATOD youth drug use; effects maintained at 5 yr. knowledge and refusal skills. follow-up.1 LifeSkills Training School-based / Universal prevention- Middle school Lower use of alcohol, cigarettes, (LST) general self-mgmt skills, social skills youth marijuana; lower rates of poly- development, ATOD knowledge and substance use; effects maintained at refusal skills. 6.5 yr. follow-up.1 Positive Action School-based / Universal Prevention K-12 Lower self-reported substance use at promotes positive school climate grades 5 and 81 Strengthening Community-based / Family program to Parent/caregiver Lower use rate of methamphetamines Families Program strengthen parent-child relationship; and their youth (12th gr), slower rate of polydrug use 10-14 peer pressure refusal skills for youth aged 10-14. (6-12th) narcotic and barbituate misuse (young adult), Rx opiod (SFP 10-14) misuse, lifetime Rx drug misuse 1 Strong African Community-based / Family program to Families with Significantly lower new alcohol user American Families strengthen parent-child relationship; youth aged 10- proportions at post-test and 2.4 year improve peer pressure refusal skills for 14 with African follow-up.1 youth; communication skills; improve American Significantly slower rate of increase in future orientation; enhance family Heritage 1 cultural pride alcohol use at 5.4 year follow-up. -

Air Traffic Management Abbreviation Compendium
Air Traffic Management Abbreviation Compendium List of Aviation, Aerospace and Aeronautical Acronyms DLR-IB-FL-BS-2021-1 Institute of Air Traffic Management Abbreviation Compendium Flight Guidance Document properties Title Air Traffic Management Abbreviation Compendium Subject List of Aviation, Aerospace and Aeronautical Acronyms Institute Institute of Flight Guidance, Braunschweig, German Aerospace Center, Germany Authors Nikolai Rieck, Marco-Michael Temme IB-Number DLR-IB-FL-BS-2021-1 Date 2021-01-28 Version 1.0 Title: Air Traffic Management Abbreviation Compendium Date: 2021-01-28 Page: 2 Version: 1.0 Authors: N. Rieck & M.-M. Temme Institute of Air Traffic Management Abbreviation Compendium Flight Guidance Index of contents 2.1. Numbers and Punctuation Marks _______________________________________________________ 6 2.2. Letter - A ___________________________________________________________________________ 7 2.3. Letter - B ___________________________________________________________________________ 55 2.4. Letter - C __________________________________________________________________________ 64 2.5. Letter - D _________________________________________________________________________ 102 2.6. Letter - E __________________________________________________________________________ 128 2.7. Letter - F __________________________________________________________________________ 152 2.8. Letter - G _________________________________________________________________________ 170 2.9. Letter - H _________________________________________________________________________ -

SOUTH Sr. PAUL MUNICIPAL AIRPORT
South St. Paul MAYOR/COUNCIL WORKSESSION SSP City Hall 125 3rd Avenue North Monday, April 22, 2013 7:00 p.m. AGENDA: 1. Review of Downtown Redevelopment Project Area and Plan 2. HRA Update 3. Continued Park Referendum Discussion a. Wakota Arena warm viewing area re-design b. Kaposia Landing and McMorrow Field Master Plan updates c. Future education and planning 4. Design options for 3rd Street, east of 9th Avenue 5. Utility Mapping on GIS 6. Airport Business Plan Review City Council Worksession Report Date: April 22, 2013 HRASfP/ (_ Agenda Item: Review of Downtown Redevelopment Project Area and Plan Attached is the Redevelopment Plan for the establishment of a Downtown Redevelopment Project Area. The Redevelopment Plan was adopted by the HRA Board of Commissioners on April 9, 2013. The purpose of establishing a project area in this part of town is to initiate planning and obtain funding for redevelopment. The HRA acquired two properties on i 11 Avenue North in 2012 and plans to purchase the remaining properties as they become available and funding permits. Other commercial properties are in need of redevelopment. 1 The recommended boundaries of the project area are 14 h Avenue South on the West, 3rd Street South to the South, 3rd Avenue North to the east and 3rd Street North to the north excluding the high school campus (see attached map of Project Area). The project Plan does not reference specific properties but states the following findings: 1. The Project Plan proposes the Authority undertake certain redevelopment activities for the purpose of encouraging redevelopment of properties in the Redevelopment Project Area. -

T.V Channel Guide
Channel Lineup Effective December 11, 2020 1-800-xfinity | xfinity.com Summit Co. Blue River, Breckenridge, Dillon, Frisco, Keystone, Silverthorne, Summit County LIMITED BASIC 644,1053 KETD HD 507 Hallmark Movies & 48 USA Network 681,1484 Food Network HD 2 KWGN (CW) 646,1025 KDEN HD (TEL) Mysteries 49 Lifetime 688,1411 Syfy HD 3 KCDO (IND) 648,1059 KPXC HD (ION) 672,1223 Golf Channel HD 50 FX 689,1207 NBC Sports 4 KCNC (CBS) 652,1007 KMGH HD (ABC) 674,1473 National 51 Comedy Central Network HD 5 KTVD (MyTV) 653,1009 KUSA HD (NBC) Geographic HD 52 NBC Sports Network 691,1409 FX HD 6 KRMA (PBS) 654,1004 KCNC HD (CBS) 675,1402 A&E HD 54 Oxygen 692,1410 FXX HD 7 KMGH (ABC) 655,1031 KDVR HD (FOX) 688,1411 Syfy HD 55 TNT 699,1450 TLC HD 8,1028 K28HI (IND) 656,1033 KQCK HD 689,1207 NBC Sports 56 Food Network 723,1606 MTV HD 9 KUSA (NBC) 660,1012 KBDI HD (PBS) Network HD 57 AMC 724,1403 USA Network HD 10,22,165 Government 701,1006 KRMA HD (PBS) 692,1410 FXX HD 59 BET 728,1728 Nickelodeon HD Access 702,1002 KWGN HD (CW) 724,1403 USA Network HD 60 MTV 730,1471 Animal Planet HD 11 KPXC (ION) 703,1014 KTFD HD (UNV) 730,1471 Animal Planet HD 61 VH1 731,1734 Cartoon 12 KBDI-DT (PBS) 704,1020 KTVD HD (MyTV) 735,1477 Smithsonian 62,1426 TV Land Network HD 13 KDVR (FOX) 705,1003 KCDO HD (IND) Channel HD 63 TBS 736,1478 HISTORY HD 14 KTFD (UMAS) 706,1050 KCEC HD (UMAS) 736,1478 HISTORY HD 64 The Weather Channel 737,1112 HLN HD 16,1016 K26GY (IND) 716,1449 Discovery HD 738,1111 CNN HD 65 Travel Channel 738,1111 CNN HD 18 HSN 717,1010 QVC2 HD2 742,1110 FOX -

Total Testosterone
Laboratory Procedure Manual Analyte: Total Testosterone Matrix: Serum Method: Analysis of total testosterone in serum by ID/HPLC/MS/MS Method No: Revised: as performed by: Clinical Chemistry Branch Division of Laboratory Sciences National Center for Environmental Health contact: Dr. Hubert W. Vesper Phone: 770-488-4191 Fax: 404-638-5393 Email: [email protected] James Pirkle, M.D., Ph.D. Division of Laboratory Sciences Important Information for Users CDC periodically refines these laboratory methods. It is the responsibility of the user to contact the person listed on the title page of each write-up before using the analytical method to find out whether any changes have been made and what revisions, if any, have been incorporated. Total Testosterone in serum NHANES2011-2012 Page 5 of 44 Public Release Data Set Information This document details the Lab Protocol for testing the items listed in the following table: File Variable SAS Label Name Name TST_G LBXTST Testosterone, total (ng/dL) Total Testosterone in serum NHANES2011-2012 Page 4 of 44 1 SUMMARY OF TEST PRINCIPLE AND CLINICAL RELEVANCE 1.1 Clinical and Public Health Relevance Clinical guidelines and position statements recommend testing for testosterone to aid in diagnosing diseases and disorders or monitoring treatments [1-6]. Testosterone measurements are used in patient care for the diagnosis of hypogonadism in men [1] and androgen excess in women with polycystic ovary syndrome being one of the conditions causing androgen excess [7,8]. Research found that testosterone levels are associated with various diseases and conditions, such as metabolic syndrome [9], diabetes [10], cardiovascular disease [11,12], fractures [13,14], neurodegenerative disorder [15,16], and higher mortality in men with lower testosterone levels [17,18]. -
A History of Regional Commercial Television Ownership and Control
Station Break: A History of Regional Commercial Television Ownership and Control Michael Thurlow B. Journalism This thesis is presented for the degree of Master of Research Macquarie University Department of Media, Music, Communication and Cultural Studies 9 October 2015 This page has been left blank deliberately. Table of contents Abstract .................................................... i Statement of Candidate .................................... iii Acknowledgements ........................................... iv Abbreviations ............................................... v Figures ................................................... vii Tables ................................................... viii Introduction ................................................ 1 Chapter 1: New Toys for Old Friends ........................ 21 Chapter 2: Regulatory Foundations and Economic Imperatives . 35 Chapter 3: Corporate Ambitions and Political Directives .... 57 Chapter 4: Digital Protections and Technical Disruptions ... 85 Conclusion ................................................ 104 Appendix A: Stage Three Licence Grants .................... 111 Appendix B: Ownership Groups 1963 ......................... 113 Appendix C: Stage Four Licence Grants ..................... 114 Appendix D: Ownership Groups 1968 ......................... 116 Appendix E: Stage Six Licence Grants ...................... 117 Appendix F: Ownership Groups 1975 ......................... 118 Appendix G: Ownership Groups 1985 ......................... 119 Appendix H: