Total Testosterone
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cable Channels
HD Channel Lineup for: Tampa Bay Area: Manatee County Displaying 459 channels. Ch. Network Ch. Network Ch. Network 3 WEDU - PBS 154 BET Jams 221 Cinemax - E 1003 WEDU - PBS 96 BET Soul 226 Cinemáx - E 605 WEDU - PBS Encore 809 BTN 61 Comedy Central 8 WFLA - NBC 820 BTN - Extra1 95 Community Programming 1008 WFLA - NBC 821 BTN - Extra2 142 Cooking Channel 11 WFTS - ABC 197 BYUtv 170 Crime & Investigation 1011 WFTS - ABC 174 Baby First TV 949 Cubaplay 10 WTSP - CBS 974 BabyFirstTV (SAP) 136 DIY Network 1010 WTSP - CBS 975 BabyTV (SAP) 524 DWLS Filipino Audio 13 WTVT - FOX 961 Bandamax 525 DZBB Filipino Audio 1013 WTVT - FOX 9 Bay News 9 171 Daystar 16 WUSF - PBS 831 BeIN SPORTS 979 De Película 1016 WUSF - PBS 913 BeIN SPORTS Español 980 De Película Clásico 617 WUSF - PBS Kids 127 Bloomberg Television 108 Destination America 7 WWSB - ABC 124 Boomerang 34 Discovery Channel 1007 WWSB - ABC 51 Bravo 922 Discovery Familia 227 5 StarMAX - E 14 C-SPAN 102 Discovery Family 48 A&E 176 C-SPAN2 114 Discovery Life Channel 567 ABP News 177 C-SPAN3 925 Discovery en Español 64 AMC 529 C1R (Russia) 40 Disney Channel 501 ART Cable 139 CBS Sports Network 179 Disney Junior 180 ASPiRE TV 590 CCTV-4 122 Disney XD 1303 AXS TV 45 CMT 923 Disney XD 223 ActionMAX - E 42 CNBC 70 E! 103 American Heroes Channel 141 CNBC World 364 EPIX 35 Animal Planet 29 CNN 365 EPIX 2 - E 557 Ant1 Greek 904 CNN en Español 367 EPIX Drive-In 960 Antena 3 Internacional 532 CTC Russian Network 1366 EPIX HITS 972 Atres Series 906 Canal Sur 27 ESPN 986 AyM Sports 936 Caracol 810 ESPN Classic 75 BBC America 58 Cartoon Network 1791 ESPN College Extra 1278 BBC America 970 Cartoon Network (SAP) 153 ESPN Deportes 123 BBC World News 907 CentroamericaTV 1196 ESPN Goal Line/Bases Loaded 71 BET 912 Cine Mexicano 28 ESPN2 107 BET HER 928 Cinelatino 150 ESPNEWS Ch. -

Apo-Nid63005.Pdf
AUSTRALIAN BROADCASTING TRIBUNAL ANNUAL REPORT 1991-92 Australian Broadcasting Tribunal Sydney 1992 ©Commonwealth of Australia ISSN 0728-8883 Design by Media and Public Relations Branch, Australian Broadcasting Tribunal. Printed in Australia by Pirie Printers Sales Pty Ltd, Fyshwick, A.CT. 11 Contents 1. MEMBERSIDP OF THE TRIBUNAL 1 2. THE YEAR IN REVIEW 7 3. POWERS AND FUNCTIONS OF THE TRIBUNAL 13 Responsible Minister 16 4. LICENSING 17 Number and Type of Licences on Issue 19 Grant of Limited Licences 20 Commercial Radio Licence Grant Inquiries 21 Supplementary Radio Grant Inquiries 23 Joined Supplementary /Independent Radio Grant Inquiries 24 Remote Licences 26 Public Radio Licence Grants 26 Renewal of Licences with Conditions or Licensee Undertaking 30 Revocation/Suspension/Conditions Inquiries 32 Allocation of Call Signs 37 5. OWNERSHIP AND CONTROL 39 Applications and Notices Received 41 Most Significant Inquiries 41 Unfinished Inquiries 47 Contraventions Amounting To Offences 49 Licence Transfers 49 Uncompleted Inquiries 50 Operation of Service by Other than Licensee 50 Registered Lender and Loan Interest Inquiries 50 6. PROGRAM AND ADVERTISING STANDARDS 51 Program and Advertising Standards 53 Australian Content 54 Compliance with Australian Content Television Standard 55 Children's Television Standards 55 Compliance with Children's Standards 58 Comments and Complaints 59 Broadcasting of Political Matter 60 Research 61 iii 7. PROGRAMS - PUBLIC INQUIRIES 63 Public Inquiries 65 Classification of Television Programs 65 Foreign Content In Television Advertisements 67 Advertising Time On Television 68 Film And Television Co-productions 70 Australian Documentary Programs 71 Cigarette Advertising During The 1990 Grand Prix 72 Test Market Provisions For Foreign Television Advertisements 72 Public Radio Sponsorship Announcements 73 Teenage Mutant Ninja Turtles 74 John Laws - Comments About Aborigines 75 Anti-Discrimination Standards 75 Accuracy & Fairness in Current Affairs 76 Religious Broadcasts 77 Review of Classification Children's Television Programs 78 8. -

COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone During SARS-Cov-2 Infection
pharmaceuticals Review COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone during SARS-CoV-2 Infection Katarzyna Kotfis 1,* , Kacper Lechowicz 1 , Sylwester Drozd˙ zal˙ 2 , Paulina Nied´zwiedzka-Rystwej 3 , Tomasz K. Wojdacz 4, Ewelina Grywalska 5 , Jowita Biernawska 6, Magda Wi´sniewska 7 and Miłosz Parczewski 8 1 Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, 70-111 Szczecin, Poland; [email protected] 2 Department of Pharmacokinetics and Monitored Therapy, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 3 Institute of Biology, University of Szczecin, 71-412 Szczecin, Poland; [email protected] 4 Independent Clinical Epigenetics Laboratory, Pomeranian Medical University, 71-252 Szczecin, Poland; [email protected] 5 Department of Clinical Immunology and Immunotherapy, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 6 Department of Anesthesiology and Intensive Therapy, Pomeranian Medical University in Szczecin, 71-252 Szczecin, Poland; [email protected] 7 Clinical Department of Nephrology, Transplantology and Internal Medicine, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 8 Department of Infectious, Tropical Diseases and Immune Deficiency, Pomeranian Medical University in Szczecin, 71-455 Szczecin, Poland; [email protected] * Correspondence: katarzyna.kotfi[email protected]; Tel.: +48-91-466-11-44 Abstract: In March 2020, coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 was declared Citation: Kotfis, K.; Lechowicz, K.; a global pandemic by the World Health Organization (WHO). The clinical course of the disease is Drozd˙ zal,˙ S.; Nied´zwiedzka-Rystwej, unpredictable but may lead to severe acute respiratory infection (SARI) and pneumonia leading to P.; Wojdacz, T.K.; Grywalska, E.; acute respiratory distress syndrome (ARDS). -

Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals
Journal of Clinical Medicine Review Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals Carlotta Cocchetti 1, Jiska Ristori 1, Alessia Romani 1, Mario Maggi 2 and Alessandra Daphne Fisher 1,* 1 Andrology, Women’s Endocrinology and Gender Incongruence Unit, Florence University Hospital, 50139 Florence, Italy; [email protected] (C.C); jiska.ristori@unifi.it (J.R.); [email protected] (A.R.) 2 Department of Experimental, Clinical and Biomedical Sciences, Careggi University Hospital, 50139 Florence, Italy; [email protected]fi.it * Correspondence: fi[email protected] Received: 16 April 2020; Accepted: 18 May 2020; Published: 26 May 2020 Abstract: Introduction: To date no standardized hormonal treatment protocols for non-binary transgender individuals have been described in the literature and there is a lack of data regarding their efficacy and safety. Objectives: To suggest possible treatment strategies for non-binary transgender individuals with non-standardized requests and to emphasize the importance of a personalized clinical approach. Methods: A narrative review of pertinent literature on gender-affirming hormonal treatment in transgender persons was performed using PubMed. Results: New hormonal treatment regimens outside those reported in current guidelines should be considered for non-binary transgender individuals, in order to improve psychological well-being and quality of life. In the present review we suggested the use of hormonal and non-hormonal compounds, which—based on their mechanism of action—could be used in these cases depending on clients’ requests. Conclusion: Requests for an individualized hormonal treatment in non-binary transgender individuals represent a future challenge for professionals managing transgender health care. For each case, clinicians should balance the benefits and risks of a personalized non-standardized treatment, actively involving the person in decisions regarding hormonal treatment. -

Effect of Dehydroepiandrosterone and Testosterone Supplementation on Systemic Lipolysis
ORIGINAL ARTICLE Effect of Dehydroepiandrosterone and Testosterone Supplementation on Systemic Lipolysis Ana E. Espinosa De Ycaza, Robert A. Rizza, K. Sreekumaran Nair, and Michael D. Jensen Division of Endocrinology, Endocrine Research Unit, Mayo Clinic, Rochester, Minnesota 55905 Downloaded from https://academic.oup.com/jcem/article/101/4/1719/2804555 by guest on 24 September 2021 Context: Dehydroepiandrosterone (DHEA) and T hormones are advertised as antiaging, antiobe- sity products. However, the evidence that these hormones have beneficial effects on adipose tissue metabolism is limited. Objective: The objective of the study was to determine the effect of DHEA and T supplementation on systemic lipolysis during a mixed-meal tolerance test (MMTT) and an iv glucose tolerance test (IVGTT). Design: This was a 2-year randomized, double-blind, placebo-controlled trial. Setting: The study was conducted at a general clinical research center. Participants: Sixty elderly women with low DHEA concentrations and 92 elderly men with low DHEA and bioavailable T concentrations participated in the study. Interventions: Elderly women received 50 mg DHEA (n ϭ 30) or placebo (n ϭ 30). Elderly men received 75 mg DHEA (n ϭ 30),5mgT(nϭ 30), or placebo (n ϭ 32). Main Outcome Measures: In vivo measures of systemic lipolysis (palmitate rate of appearance) during a MMTT or IVGTT. Results: At baseline there was no difference in insulin suppression of lipolysis measured during MMTT and IVGTT between the treatment groups and placebo. For both sexes, a univariate analysis showed no difference in changes in systemic lipolysis during the MMTT or IVGTT in the DHEA group and T group when compared with placebo. -

Reproductive DHEA-S
Reproductive DHEA-S Analyte Information - 1 - DHEA-S Introduction DHEA-S, DHEA sulfate or dehydroepiandrosterone sulfate, it is a metabolite of dehydroepiandrosterone (DHEA) resulting from the addition of a sulfate group. It is the sulfate form of aromatic C19 steroid with 10,13-dimethyl, 3-hydroxy group and 17-ketone. Its chemical name is 3β-hydroxy-5-androsten-17-one sulfate, its summary formula is C19H28O5S and its molecular weight (Mr) is 368.5 Da. The structural formula of DHEA-S is shown in (Fig.1). Fig.1: Structural formula of DHEA-S Other names used for DHEA-S include: Dehydroisoandrosterone sulfate, (3beta)-3- (sulfooxy), androst-5-en-17-one, 3beta-hydroxy-androst-5-en-17-one hydrogen sulfate, Prasterone sulfate and so on. As DHEA-S is very closely connected with DHEA, both hormones are mentioned together in the following text. Biosynthesis DHEA-S is the major C19 steroid and is a precursor in testosterone and estrogen biosynthesis. DHEA-S originates almost exclusively in the zona reticularis of the adrenal cortex (Fig.2). Some may be produced by the testes, none is produced by the ovaries. The adrenal gland is the sole source of this steroid in women, whereas in men the testes secrete 5% of DHEA-S and 10 – 20% of DHEA. The production of DHEA-S and DHEA is regulated by adrenocorticotropin (ACTH). Corticotropin-releasing hormone (CRH) and, to a lesser extent, arginine vasopressin (AVP) stimulate the release of adrenocorticotropin (ACTH) from the anterior pituitary gland (Fig.3). In turn, ACTH stimulates the adrenal cortex to secrete DHEA and DHEA-S, in addition to cortisol. -

Safety Data Sheet
SAFETY DATA SHEET SECTION 1: PRODUCT IDENTIFICATION PRODUCT NAME DHEA (Prasterone) (Micronized) PRODUCT CODE 0733 SUPPLIER MEDISCA Inc. Tel.: 1.800.932.1039 | Fax.: 1.855.850.5855 661 Route 3, Unit C, Plattsburgh, NY, 12901 3955 W. Mesa Vista Ave., Unit A-10, Las Vegas, NV, 89118 6641 N. Belt Line Road, Suite 130, Irving, TX, 75063 MEDISCA Pharmaceutique Inc. Tel.: 1.800.665.6334 | Fax.: 514.338.1693 4509 Rue Dobrin, St. Laurent, QC, H4R 2L8 21300 Gordon Way, Unit 153/158, Richmond, BC V6W 1M2 MEDISCA Australia PTY LTD Tel.: 1.300.786.392 | Fax.: 61.2.9700.9047 Unit 7, Heritage Business Park 5-9 Ricketty Street, Mascot, NSW 2020 EMERGENCY PHONE CHEMTREC Day or Night Within USA and Canada: 1-800-424-9300 NSW Poisons Information Centre: 131 126 USES Adjuvant; Androgen SECTION 2: HAZARDS IDENTIFICATION GHS CLASSIFICATION Toxic to Reproduction (Category 2) PICTOGRAM SIGNAL WORD Warning HAZARD STATEMENT(S) Reproductive effector, prohormone. Suspected of damaging fertility or the unborn child. May cause harm to breast-fed children. Causes serious eye irritation. Causes skin and respiratory irritation. Very toxic to aquatic life with long lasting effects. AUSTRALIA-ONLY HAZARDS Not Applicable. PRECAUTIONARY STATEMENT(S) Prevention Wash thoroughly after handling. Obtain special instructions before use. Do not handle until all safety precautions have been read and understood. Do not breathe dusts or mists. Do not eat, drink or smoke when using this product. Avoid contact during pregnancy/while nursing. Wear protective gloves, protective clothing, eye protection, face protection. Avoid release to the environment. Response IF ON SKIN (HAIR): Wash with plenty of water. -

Alpha ELT Listing
Lienholder Name Lienholder Address City State Zip ELT ID 1ST ADVANTAGE FCU PO BX 2116 NEWPORT NEWS VA 23609 CFW 1ST COMMAND BK PO BX 901041 FORT WORTH TX 76101 FXQ 1ST FNCL BK USA 47 SHERMAN HILL RD WOODBURY CT 06798 GVY 1ST LIBERTY FCU PO BX 5002 GREAT FALLS MT 59403 ESY 1ST NORTHERN CA CU 1111 PINE ST MARTINEZ CA 94553 EUZ 1ST NORTHERN CR U 230 W MONROE ST STE 2850 CHICAGO IL 60606 GVK 1ST RESOURCE CU 47 W OXMOOR RD BIRMINGHAM AL 35209 DYW 1ST SECURITY BK WA PO BX 97000 LYNNWOOD WA 98046 FTK 1ST UNITED SVCS CU 5901 GIBRALTAR DR PLEASANTON CA 94588 W95 1ST VALLEY CU 401 W SECOND ST SN BERNRDNO CA 92401 K31 360 EQUIP FIN LLC 300 BEARDSLEY LN STE D201 AUSTIN TX 78746 DJH 360 FCU PO BX 273 WINDSOR LOCKS CT 06096 DBG 4FRONT CU PO BX 795 TRAVERSE CITY MI 49685 FBU 777 EQUIPMENT FIN LLC 600 BRICKELL AVE FL 19 MIAMI FL 33131 FYD A C AUTOPAY PO BX 40409 DENVER CO 80204 CWX A L FNCL CORP PO BX 11907 SANTA ANA CA 92711 J68 A L FNCL CORP PO BX 51466 ONTARIO CA 91761 J90 A L FNCL CORP PO BX 255128 SACRAMENTO CA 95865 J93 A L FNCL CORP PO BX 28248 FRESNO CA 93729 J95 A PLUS FCU PO BX 14867 AUSTIN TX 78761 AYV A PLUS LOANS 500 3RD ST W SACRAMENTO CA 95605 GCC A/M FNCL PO BX 1474 CLOVIS CA 93613 A94 AAA FCU PO BX 3788 SOUTH BEND IN 46619 CSM AAC CU 177 WILSON AVE NW GRAND RAPIDS MI 49534 GET AAFCU PO BX 619001 MD2100 DFW AIRPORT TX 75261 A90 ABLE INC 503 COLORADO ST AUSTIN TX 78701 CVD ABNB FCU 830 GREENBRIER CIR CHESAPEAKE VA 23320 CXE ABOUND FCU PO BX 900 RADCLIFF KY 40159 GKB ACADEMY BANK NA PO BX 26458 KANSAS CITY MO 64196 ATF ACCENTRA CU 400 4TH -

A10 Anabolic Steroids Hardcore Info
CONTENTS GENERAL INFORMATION 3 Anabolic steroids – What are they? 4 How do they Work? – Aromatisation 5 More molecules – More problems 6 The side effects of anabolic steroids 7 Women and anabolic steroids 8 Injecting steroids 9 Abscesses – Needle Exchanges 10 Intramuscular injection 11 Injection sites 12 Oral steroids – Cycles – Stacking 13 Diet 14 Where do steroids come from? Spotting a counterfeit 15 Drug Information – Drug dosage STEROIDS 16 Anadrol – Andriol 17 Anavar – Deca-Durabolin 18 Dynabolon – Durabolin – Dianabol 19 Esiclene – Equipoise 20 Primobolan Depot – Proviron – Primobolan orals – Pronobol 21 Sustanon – Stromba, Strombaject – Testosterone Cypionate Testosterone Enanthate 22 Testosterone Propionate – Testosterone Suspension 23 Trenbolone Acetate – Winstrol OTHER DRUGS 24 Aldactone – Arimidex 25 Clenbuterol – Cytomel 26 Ephedrine Hydrochloride – GHB 27 Growth Hormone 28 Insulin 30 Insulin-Like Growth Factor-1 – Human Chorionic Gonadotrophin 31 Tamoxifen – Nubain – Recreational Drugs 32 Steroids and the Law 34 Glossary ANABOLIC STEROIDS People use anabolic steroids for various reasons, some use them to build muscle for their job, others just want to look good and some use them to help them in sport or body building. Whatever the reason, care needs to be taken so that as little harm is done to the body as possible because despite having muscle building effects they also have serious side effects especially when used incorrectly. WHAT ARE THEY? Anabolic steroids are man made versions of the hormone testosterone. Testosterone is the chemical in men responsible for facial hair, deepening of the voice and sex organ development, basically the masculine things Steroids are in a man. used in medicine to treat anaemia, muscle weakness after These masculine effects surgery etc, vascular are called the androgenic disorders and effects of testosterone. -

Gender-Affirming Hormone Therapy
GENDER-AFFIRMING HORMONE THERAPY Julie Thompson, PA-C Medical Director of Trans Health, Fenway Health March 2020 fenwayhealth.org GOALS AND OBJECTIVES 1. Review process of initiating hormone therapy through the informed consent model 2. Provide an overview of masculinizing and feminizing hormone therapy 3. Review realistic expectations and benefits of hormone therapy vs their associated risks 4. Discuss recommendations for monitoring fenwayhealth.org PROTOCOLS AND STANDARDS OF CARE fenwayhealth.org WPATH STANDARDS OF CARE, 2011 The criteria for hormone therapy are as follows: 1. Well-documented, persistent (at least 6mo) gender dysphoria 2. Capacity to make a fully informed decision and to consent for treatment 3. Age of majority in a given country 4. If significant medical or mental health concerns are present, they must be reasonably well controlled fenwayhealth.org INFORMED CONSENT MODEL ▪ Requires healthcare provider to ▪ Effectively communicate benefits, risks and alternatives of treatment to patient ▪ Assess that the patient is able to understand and consent to the treatment ▪ Informed consent model does not preclude mental health care! ▪ Recognizes that prescribing decision ultimately rests with clinical judgment of provider working together with the patient ▪ Recognizes patient autonomy and empowers self-agency ▪ Decreases barriers to medically necessary care fenwayhealth.org INITIAL VISITS ▪ Review history of gender experience and patient’s goals ▪ Document prior hormone use ▪ Assess appropriateness for gender affirming medical -

Project ASPIRE: Empowering Families of Children Wi H H I L with Hearing Loss
Project ASPIRE: Empowering Families of Children Wit h Hear ing Loss Sophie Shay, MSII Lyra Repplinger, M.S. Dana L. Suskind, M.D. AdAgenda { Pro jec t ASPIRE { Exploring Health Disparities { Developing A Best Practices Curriculum { The Modules { Module Components { The Dream { Research Protocol/Pilot Testing { Q & A What i s P roj ec t ASPIRE? { Pro ject ASPIRE: Achiev ing Superior Parental Involvement for Rehabilitative Excellence z A comprehensive interactive multimedia intervention z Imparts knowledge and skills for parents of economically disadvantaged children to aid in their children’s listening, language and spppeech development after im plantation z Empowers parents Impetus for the Program: IltOtImplant Outcome Di Diitisparities { Econom ica lly disa dvan tage d imp lan t recip ien ts have less favorable outcomes than their more affluent peers (Witkin, 2005;Easterbrooks, O’Rourke & Todd, 2000) { Factors in Outcome Disparities z Access and Availability of Habilitation z Inadequate Parental Skills to support their child’s language development (Geers, 2006; Moog & Geers, 2003, Easterbrooks, O’Rourke & Todd, 2000) What A re H ealth Dispar ities ? { Unequa l bur den in disease morbidity and morta lity rates experienced by ethnic/racial groups as compared to the dominant group { Widening disparity in the United States affecting all aspects of healthcare { Socioeconomic status (SES): the most frequently cited, and most consistent, contributor z SES=income, education, wealth or a combination { Healthy People 2010 has designated the elimination of health disparities as one of its essential goal z Improved hearing health of the nation through prevention, early detection, treatment and rehabilitation z Successful Implantation and Habilitation of Children Makes good economic sense! Children an d Pover ty BELOW 100% BELOW 150% RACE POVERTY** POVERTY** White 13. -
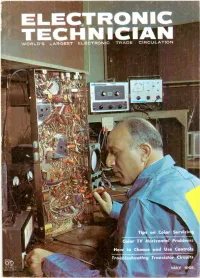
Electronics-Technici
WORLD'S LARGEST ELECTRONIC TRADE CIRCULATION Tips on Color Servicir Color TV Horizontal Problems How to Choose and Use Controls Troubleshooting Transistor Circuits MAY 1965 ENirr The quality goes in before the name goes on FOR THE FINEST COLOR AND UHF RECEPTION INSTALL ZENITH QUALITY ANTENNAS ... to assure finer performance in difficult reception areas! More color TV sets and new UHF stations mean new antenna installation jobs for you. Proper installation with antennas of Zenith quality is most important because of the sensi tivity of color and JHF signals. ZENITH ALL -CHANNEL VHF/UHF/FM AND FM -STEREO LOG -PERIODIC ANTENNAS The unusually broad bandwidth of the new Zenith VHF/UHF/FM and FM -Stereo log -periodic resonant V -dipole arrays pulls in all frequencies from 50 to 900 mc-television channels 2 to 83 /\' plus FM radio. The multi -mode operation pro- vides nigh gain and good rejection of ghosts. These frequency independent antennas, devel- , oped // by the research laboratories at the University of Illinois, are designed according to a geometrically derived logarithmic -periodic formula used in satellite telemetry. ZENITH QUALITY HEAVY-DUTY ZENITH QUALITY ANTENNA ROTORS WIRE AND CABLE Zenith quality antenna rotors are Zenith features a full line of quality heavy-duty throughout-with rugged packaged wire and cable. Also espe- motor and die-cast aluminum hous- cially designed UHF transmission ing. Turns a 150-Ib. antenna 360 de- wires, sold only by Zenith. Zenith grees in 45 seconds. The weather- wire and cable is engineered for proof bell casting protects the unit greater reception and longer life, from the elements.