Is the Madrid Sonographic Enthesitis Index Useful for Differentiating Psoriatic Arthritis from Psoriasis Alone and Healthy Controls?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OES Site Color Scheme 1
Nuisance Problems You will Grow to Love Thomas V Gocke, MS, ATC, PA-C, DFAAPA President & Founder Orthopaedic Educational Services, Inc. Boone, NC [email protected] www.orthoedu.com Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Faculty Disclosures • Orthopaedic Educational Services, Inc. Financial Intellectual Property No off label product discussions American Academy of Physician Assistants Financial PA Course Director, PA’s Guide to the MSK Galaxy Urgent Care Association of America Financial Intellectual Property Faculty, MSK Workshops Ferring Pharmaceuticals Consultant Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. 2 LEARNING GOALS At the end of this sessions you will be able to: • Recognize nuisance conditions in the Upper Extremity • Recognize nuisance conditions in the Lower Extremity • Recognize common Pediatric Musculoskeletal nuisance problems • Recognize Radiographic changes associates with common MSK nuisance problems • Initiate treatment plans for a variety of MSK nuisance conditions Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Inflammatory Response Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Inflammatory Response* When does the Inflammatory response occur: • occurs when injury/infection triggers a non-specific immune response • causes proliferation of leukocytes and increase in blood flow secondary to trauma • increased blood flow brings polymorph-nuclear leukocytes (which facilitate removal of the injured cells/tissues), macrophages, and plasma proteins to injured tissues *Knight KL, Pain and Pain relief during Cryotherapy: Cryotherapy: Theory, Technique and Physiology, 1st edition, Chattanooga Corporation, Chattanooga, TN 1985, p 127-137 Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. -

The Anatomy of the Deep Infrapatellar Bursa of the Knee Robert F
0363-5465/98/2626-0129$02.00/0 THE AMERICAN JOURNAL OF SPORTS MEDICINE, Vol. 26, No. 1 © 1998 American Orthopaedic Society for Sports Medicine The Anatomy of the Deep Infrapatellar Bursa of the Knee Robert F. LaPrade,* MD Department of Orthopaedic Surgery, University of Minnesota, Minneapolis, Minnesota ABSTRACT knee joint, and to define a consistent surgical approach to the deep infrapatellar bursa. Disorders of the deep infrapatellar bursa are important to include in the differential diagnosis of anterior knee pain. Knowledge regarding its anatomic location can MATERIALS AND METHODS aid the clinician in establishing a proper diagnosis. Fifty cadaveric knees were dissected, and the deep infrapa- Thorough dissections of the anterior aspect of the knee of tellar bursa had a consistent anatomic location in all 50 nonpaired cadaveric knees were performed. There were specimens. The deep infrapatellar bursa was located 27 male and 23 female cadaveric knees with 25 right and directly posterior to the distal 38% of the patellar ten- 25 left knees. The average age of the specimens was 71.8 don, just proximal to its insertion on the tibial tubercle. years (range, 42 to 93). After the skin and subcutaneous There was no communication to the knee joint. Its tissues of the anterior aspect of the knee were carefully average width at the most proximal margin of the tibial dissected away, an approach to the deep infrapatellar tubercle was slightly wider than the average distal bursa of the knee was made through medial and lateral width of the patellar tendon. It was found to be partially arthrotomy incisions along the patella, followed by compartmentalized, with a fat pad apron extending transection of the quadriceps tendon from the patella. -

Case Report Septic Infrapatellar Bursitis in an Immunocompromised Female
Hindawi Case Reports in Orthopedics Volume 2018, Article ID 9086201, 3 pages https://doi.org/10.1155/2018/9086201 Case Report Septic Infrapatellar Bursitis in an Immunocompromised Female Kenneth Herring , Seth Mathern, and Morteza Khodaee 1Department of Family Medicine, University of Colorado School of Medicine, 3055 Roslyn Street, Denver, CO 80238, USA Correspondence should be addressed to Kenneth Herring; [email protected] Received 8 April 2018; Revised 19 April 2018; Accepted 20 April 2018; Published 6 June 2018 Academic Editor: John Nyland Copyright © 2018 Kenneth Herring et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Bursitis is a relatively common occurrence that may be caused by traumatic, inflammatory, or infectious processes. Septic bursitis most commonly affects the olecranon and prepatellar bursae. Staphylococcus aureus accounts for 80% of all septic bursitis, and most cases affect men and are associated with preceding trauma. We present a case of an 86-year-old female with an atypical septic bursitis involving the infrapatellar bursa. Not only are there very few reported cases of septic infrapatellar bursitis, but also this patient’s case is particularly unusual in that she is a female with no preceding trauma who had Pseudomonas aeruginosa on aspirate. The case also highlights the diagnostic workup of septic bursitis through imaging modalities and aspiration. This patient had full resolution of her septic bursitis with appropriate IV antibiotics. 1. Introduction and relative superficial location, the olecranon and prepa- tellar bursae are the most common sites of septic bursitis The human body contains upwards of 150 bursae, many [3, 4]. -

Anterior Knee Pain
Page 1 of 4 Anterior Knee Pain Anterior knee pain is common with a variety of causes.[1] It is important to make a careful assessment of the underlying cause in order to ensure appropriate management and advice, Common causes [2] Patellofemoral pain syndrome (PFPS) PFPS is defined as pain behind or around the patella, caused by stress in the patellofemoral joint. PFPS is common. Symptoms are usually provoked by climbing stairs, squatting, and sitting with flexed knees for long periods of time.[3] PFPS seems to be multifactorial, resulting from a complex interaction between intrinsic anatomy and external training factors.[4] Pain and dysfunction often result from either abnormal forces or prolonged repetitive compressive or shearing forces between the patella and the femur. Patellofemoral pain syndrome (PFPS) is a common cause of knee pain in adolescents and young adults, especially among those who are physically active and regularly participate in sports. Although PFPS most often presents in adolescents and young adults, it can occur at any age. Over half of all cases are bilateral (but one side is often more affected than the other). The potential causes of PFPS remain controversial but include overuse, overloading and misuse of the patellofemoral joint. Underlying causes of PFPS include: Overuse of the knee - eg, in sporting activities. Minor problems in the alignment of the knee. Foot problems - eg, flat feet. Repeated minor injuries to the knee. Joint hypermobility affecting the knee. Reduced muscle strength in the leg. Physiotherapy and foot orthoses are often used in the management of PFPS.[5] Other common causes of anterior knee pain in adolescents These include: Osgood-Schlatter disease See the separate article on Osgood-Schlatter Disease. -

A Study on Effectiveness of Low Level Laser Therapy and Mcconnell Taping in Subjects with Infrapatellar Bursistis
Volume 4, Issue 10, October – 2019 International Journal of Innovative Science and Research Technology ISSN No:-2456-2165 A Study on Effectiveness of Low Level Laser Therapy and Mcconnell Taping in Subjects with Infrapatellar Bursistis T Hemalatha 1,R madhumathi 2 ,Dr. S. Senthil Kumar3 1,2IV Year, Saveetha College of Physiotherapy, Saveetha University, Thandalam, Chennai -102, Tamil Nadu 3Associate Professor, MPT (Ortho), PhD (REHAB), Saveetha College of Physiotherapy, Saveetha University, Thandalam, Chennai - 102, Tamil Nadu. Abstract:- Conclusion: The combination of low level laser therapy and Background : along with MCconnell taping was effective in pain Infrapaetallar bursa, is located just below the reduction in subjects with Infrapatellar bursistis. kneecap to essentially reduce the friction between structures such as muscle,tendon, and skin to slide over Keywords:- Knee Bursitis, NPRS, Low Level Laser bony surface without catching, during the weight bearing Therapy,MC Connell Taping. activity. Infrapatellar bursistis is one the common bursistis seen in the knee joint due to repitive strain and I. INTRODUCTION irritation to the patella tendon, often from jumping activities. This condition mainly interferes with daily Knee osteoarthritis is one of a common entity in every activites like walking, and long standing. occupational groups. Among that, knee bursitis is found to show some demanding quality of symptoms found only on Aim: the people who perform activities related to kneeling. A To find out the combined therapeutic effects of low bursa is a thin sack filled with synovial fluid , which reduces level laser therapy and MCconnell taping in improving the friction between the structures by lubrication. 1,2 pain reduction and range of motion (functional activity) in subjects with Infrapatellar bursistis. -

Infrapatellar Bursitis Presenting As a Lump Mantu Jain , Manmatha Nayak, Sajid Ansari, Bishnu Prasad Patro
Images in… BMJ Case Rep: first published as 10.1136/bcr-2021-243581 on 25 May 2021. Downloaded from Infrapatellar bursitis presenting as a lump Mantu Jain , Manmatha Nayak, Sajid Ansari, Bishnu Prasad Patro Orthopaedics, All India DESCRIPTION Institute of Medical Sciences, A bursa is a fluid-filled sac meant to reduce the Bhubaneswar, India friction between surfaces.1 A bursa can be superfi- cial when present between the skin and underlying Correspondence to tendon or bone such as the prepatellar, infrapa- Dr Mantu Jain; 2 montu_ jn@ yahoo. com tellar, olecranon bursa or superficial calcaneal. Deep bursae are located deep to the facia, typically 3 4 Accepted 12 May 2021 between muscles, tendon, and bones. Trauma, particularly repetitive, overuse, haemorrhage and, crystal disease, infection, are some of the common causes for inflammation of the bursa leading to bursitis.1 3 5 6 There could be systemic illness in some cases, and in a few, the cause remains unknown.7 Occupation and habitual or practices predispose certain types known by eponyms such as prepa- Figure 2 MRI findings axial and sagittal showing fluid tellar bursitis, also known as housemaid’s knee, and filled sac (A–C); excised mass (D) and histopathological superficial infrapatellar bursitis synonymous with study displaying chronic inflammatory tissue covered with 8 clergyman’s knee. The bursa with chronic inflam- fibrinous debris; 20×; H&E stain (E). mation may have calcification or become a solid lump losing its fluid content.7 9 This case depicts such a case wherein the patient presented with fat- suppressed images associated with surrounding painful swelling. -

Childhood and Adolescent Sports-Related Overuse Injuries KYLE J
Childhood and Adolescent Sports-Related Overuse Injuries KYLE J. CASSAS, M.D., and AMELIA CASSETTARI-WAYHS, M.D., Methodist Health System, Dallas, Texas Youth sports participation carries an inherent risk of injury, includ- ing overuse injuries. Little leaguer’s shoulder, a stress fracture of the proximal humerus that presents as lateral shoulder pain, usually is self- limited. Little leaguer’s elbow is a medial stress injury; treatment con- sists of complete rest from throwing for four to six weeks followed by rehabilitation and a gradual throwing program. Spondylolysis is a stress fracture of the pars interarticularis. Diagnostic modalities include plain film radiography, bone scan, computed tomography, single photon emission computed tomography, and magnetic resonance imaging. Treatment usually is conservative. Spondylolisthesis is the forward or anterior displacement of one vertebral body over another and may be related to a history of spondylolysis. Diagnosis is made with plain film radiography and graded according to the amount of displacement. Osgood-Schlatter disease presents as anterior knee pain localized to the tibial tubercle. Diagnosis is made clinically, and most patients respond to conservative measures. Calcaneal apophysitis (or Sever’s disease) is a common cause of heel pain in young athletes, presenting as pain in the posterior aspect of the calcaneus. (Am Fam Physician 2006;73:1014-22. Copyright © 2006 American Academy of Family Physicians.) SCOTT BY ILLUSTRATION BODELL S Patient information: ach year in the United States, develop in young athletes when this growth A handout on Osgood- approximately 30 million children center is unable to meet the demands placed Schlatter disease is available online at http:// and teenagers participate in orga- on it during activity. -

Common Superficial Bursitis MORTEZA KHODAEE, MD, MPH, University of Colorado School of Medicine, Aurora, Colorado
Common Superficial Bursitis MORTEZA KHODAEE, MD, MPH, University of Colorado School of Medicine, Aurora, Colorado Superficial bursitis most often occurs in the olecranon and prepatellar bursae. Less common locations are the superficial infrapatellar and subcutaneous (superficial) calcaneal bursae. Chronic microtrauma (e.g., kneeling on the prepatellar bursa) is the most common cause of superficial bursitis. Other causes include acute trauma/hem- orrhage, inflammatory disorders such as gout or rheumatoid arthritis, and infection (septic bursitis). Diagnosis is usually based on clinical presentation, with a particular focus on signs of septic bursitis. Ultrasonography can help distinguish bursitis from cellulitis. Blood testing (white blood cell count, inflammatory markers) and magnetic resonance imaging can help distinguish infectious from noninfectious causes. If infection is suspected, bursal aspi- ration should be performed and fluid examined using Gram stain, crystal analysis, glucose measurement, blood cell count, and culture. Management depends on the type of bursitis. Acute traumatic/hemorrhagic bursitis is treated conservatively with ice, elevation, rest, and analgesics; aspiration may shorten the duration of symptoms. Chronic microtraumatic bursitis should be treated conservatively, and the underlying cause addressed. Bursal aspiration of microtraumatic bursitis is generally not recommended because of the risk of iatrogenic septic bursitis. Although intrabursal corticosteroid injections are sometimes used to treat microtraumatic bursitis, high-quality evidence demonstrating any benefit is unavailable. Chronic inflammatory bursitis (e.g., gout, rheumatoid arthritis) is treated by addressing the underlying condition, and intrabursal corticosteroid injections are often used. For septic bursitis, antibiotics effective against Staphylococcus aureus are generally the initial treatment, with surgery reserved for bur- sitis not responsive to antibiotics or for recurrent cases. -

Management of Septic Bursitis
Joint Bone Spine 86 (2019) 583–588 Available online at ScienceDirect www.sciencedirect.com Review Management of septic bursitis a,∗ b c,d,e Christian Lormeau , Grégoire Cormier , Johanna Sigaux , f,g c,d,e Cédric Arvieux , Luca Semerano a Service de rhumatologie, centre hospitalier de Niort, 40, avenue Charles-de-Gaulle, 79021 Niort, France b Service de rhumatologie, centre hospitalier départemental Vendée, boulevard Stéphane-Moreau, 85928 La Roche-sur-Yon, France c Inserm, UMR 1125, 1, rue de Chablis, 93017 Bobigny, France d Sorbonne Paris Cité, université Paris 13, 1, rue de Chablis, 93017 Bobigny, France e − Service de rhumatologie, groupe hospitalier Avicenne Jean-Verdier–René-Muret, Assistance publique–Hôpitaux de Paris (AP−HP), 125, rue de Stalingrad, 93017 Bobigny, France f Clinique des maladies infectieuses, CHU de Rennes Pontchaillou, rue Henri-Le-Guilloux, 35043 Rennes, France g Centre de référence en infections ostéoarticulaires complexes du Grand Ouest (CRIOGO), CHU de Rennes, 35043 Rennes cedex, France a r t i c l e i n f o a b s t r a c t Article history: Superficial septic bursitis is common, although accurate incidence data are lacking. The olecranon and Accepted 10 September 2018 prepatellar bursae are the sites most often affected. Whereas the clinical diagnosis of superficial bursitis Available online 26 October 2018 is readily made, differentiating aseptic from septic bursitis usually requires examination of aspirated bursal fluid. Ultrasonography is useful both for assisting in the diagnosis and for guiding the aspiration. Keywords: Staphylococcus aureus is responsible for 80% of cases of superficial septic bursitis. Deep septic bursitis Bursitis is uncommon and often diagnosed late. -
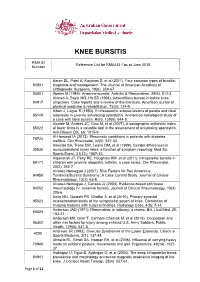
Reference List for RMA431-1As at June 2018 Number
KNEE BURSITIS RMA ID Reference List for RMA431-1as at June 2018 Number Aaron DL, Patel A, Kayiaros S, et al (2011). Four common types of bursitis: 84931 diagnosis and management. The Journal of American Academy of Orthopaedic Surgeons, 19(6): 359-67. 85001 Abeles M (1986). Anserine bursitis. Arthritis & Rheumatism, 29(6): 812-3. Ahmed A, Bayol MG, Ha SB (1994). Adventitious bursae in below knee 84917 amputees. Case reports and a review of the literature. American journal of physical medicine & rehabilitation, 73(2): 124-9. Albert J, Lagier R (1983). Enthesopathic erosive lesions of patella and tibial 85148 tuberosity in juvenile ankylosing spondylitis. Anatomico-radiological study of a case with tibial bursitis. Rofo, 139(5): 544-8. Alcalde M, Acebes JC, Cruz M, et al (2007). A sonographic enthesitic index 85022 of lower limbs is a valuable tool in the assessment of ankylosing spondylitis. Ann Rheum Dis, 66: 1015-9. Al-Homood IA (2013). Rheumatic conditions in patients with diabetes 78722 mellitus. Clin Rheumatol, 32(5): 527-33. Almeida SA, Trone DW, Leone DM, et al (1999). Gender differences in 39530 musculoskeletal injury rates: a function of symptom reporting. Med Sci Sports Exerc, 31(12): 1807-12. Alqanatish JT, Petty RE, Houghton KM, et al (2011). Infrapatellar bursitis in 85171 children with juvenile idiopathic arthritis: a case series. Clin Rheumatol, 30(2): 263-7. Alvarez-Nemegyei J (2007). Risk Factors for Pes Anserinus 84950 Tendinitis/Bursitis Syndrome: A Case Control Study. Journal of Clinical Rheumatology, 13(2): 63-5. Alvarez-Nemegyei J, Canoso JJ (2004). Evidence-based soft tissue 84552 rheumatology IV: anserine bursitis. -

ARTHRITIS FOUNDATION Painful Area for 15 - 20 Minutes 3 - 4 Times Daily May Also Help
6/29/11 10:38:13 AM The Bone and Joint Decade is a global campaign to improve conditions musculoskeletal with people for life of quality the and to advance understanding treatment of those conditions through research, prevention and education. part of our continuing education programme for all people with arthritis. ARTHRITIS FOUNDATION Registered Nonprofit Organisation - No. 002-847 NPO Helpline No: 0861 30 30 30 This information leaflet is published Arthritis by Foundation the as and RELATED and RELATED CONDITIONS BURSITIS, TENDINITIS THE CARPAL TUNNEL SYNDROME NATIONAL OFFICE Bloemfontein Branch 709 Tulbagh Centre PO Box 20269, Willows 9320 ARTHRITIS FOUNDATION Hans Strijdom Avenue Cell: 082 921 4234 Registered Non-profit organisation number 002 847 NPO Cape Town 8001 Fax: (051) 447-0451 MEMBERSHIP APPLICATION/ANNUAL RENEWAL FORM PO Box 6775 E-mail: [email protected] Roggebaai 8012 Eastern Cape Branch Please tick relevant boxes: Tel: (021) 425-2344 PO Box 7740 New application Renewal Fax: (021) 421-7330 Newton Park 6055 Website: http//www.arthritis.org.za Individual membership R 100 International membership R300 Tel: (041) 365-1419 E-mail: [email protected] Corporate membership R5 000 Other R Cell: 082 576 0382 National Helpline: 0861 30 30 30 Donation R Total R E-mail: [email protected] (For details of Associate membership (individuals joining through the community outreach programme. Johannesburg Branch Western Cape Branch Please contact your local branch). PO Box 87360, Houghton 2041 705 Tulbagh Centre My -

Imaging Ultrasound Imaging for the Rheumatologist XI. Ultrasound Imaging in Regional Pain Syndromes A
Imaging Ultrasound imaging for the rheumatologist XI. Ultrasound imaging in regional pain syndromes A. Iagnocco1, E. Filippucci2, G. Meenagh3, L. Riente4, A. Delle Sedie4, S. Bombardieri4, W. Grassi2, G. Valesini1 1Cattedra di Reumatologia, Sapienza - ABSTRACT In the present review, an update of the Università di Roma, Roma, Italy; Regional pain syndromes (RPS) are available data about US imaging in 2 Cattedra di Reumatologia, Università common complaints in clinical rheu- RPS is provided and the research agen- Politecnica delle Marche, Jesi, Italy; matological practice. Ultrasound (US) da relating to US imaging of local soft 3AntrimAntrim AreaArea Hospital,Hospital, Antrim,Antrim, NorthernNorthern Ireland, United Kingdom; allows a detailed assessment of soft tis- tissue rheumatism is discussed. 4Unità Operativa di Reumatologia, sue involvement and its use may have Università di Pisa, Pisa, Italy. considerable impact on the manage- Clinical applications Annamaria Iagnocco, MD; Emilio ment of RPS. The present review pro- A list of the most common RPS to- Filippucci, MD; Gary Meenagh, MD; vides an update of the available data gether with the corresponding patho- Lucrezia Riente, MD; Andrea Delle Sedie, about US imaging in RPS together with logical conditions that may be revealed MD; Stefano Bombardieri, MD, Professor research issues relating to periarticu- by US is presented in Table I. Differ- of Rheumatology; Walter Grassi, MD, lar soft tissue pathology. The research ent pathological conditions may mani- Professor of Rheumatology; Guido agenda covers: defi nition of standard fest with similar clinical features and Valesini, MD, Professor of Rheumatology. scanning protocols for US examination US assessment may be critical for the Please address correspondence to: of the most common RPS assessed by Dr.