Altered Expression of TSPAN32 During B Cell Activation and Systemic Lupus Erythematosus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Machine-Learning and Chemicogenomics Approach Defi Nes and Predicts Cross-Talk of Hippo and MAPK Pathways
Published OnlineFirst November 18, 2020; DOI: 10.1158/2159-8290.CD-20-0706 RESEARCH ARTICLE Machine -Learning and Chemicogenomics Approach Defi nes and Predicts Cross-Talk of Hippo and MAPK Pathways Trang H. Pham 1 , Thijs J. Hagenbeek 1 , Ho-June Lee 1 , Jason Li 2 , Christopher M. Rose 3 , Eva Lin 1 , Mamie Yu 1 , Scott E. Martin1 , Robert Piskol 2 , Jennifer A. Lacap 4 , Deepak Sampath 4 , Victoria C. Pham 3 , Zora Modrusan 5 , Jennie R. Lill3 , Christiaan Klijn 2 , Shiva Malek 1 , Matthew T. Chang 2 , and Anwesha Dey 1 ABSTRACT Hippo pathway dysregulation occurs in multiple cancers through genetic and non- genetic alterations, resulting in translocation of YAP to the nucleus and activation of the TEAD family of transcription factors. Unlike other oncogenic pathways such as RAS, defi ning tumors that are Hippo pathway–dependent is far more complex due to the lack of hotspot genetic alterations. Here, we developed a machine-learning framework to identify a robust, cancer type–agnostic gene expression signature to quantitate Hippo pathway activity and cross-talk as well as predict YAP/TEAD dependency across cancers. Further, through chemical genetic interaction screens and multiomics analyses, we discover a direct interaction between MAPK signaling and TEAD stability such that knockdown of YAP combined with MEK inhibition results in robust inhibition of tumor cell growth in Hippo dysregulated tumors. This multifaceted approach underscores how computational models combined with experimental studies can inform precision medicine approaches including predictive diagnostics and combination strategies. SIGNIFICANCE: An integrated chemicogenomics strategy was developed to identify a lineage- independent signature for the Hippo pathway in cancers. -

An Extracellular Site on Tetraspanin CD151 Determines Α3 and Α6
JCBArticle An extracellular site on tetraspanin CD151 determines ␣3 and ␣6 integrin–dependent cellular morphology Alexander R. Kazarov, Xiuwei Yang, Christopher S. Stipp, Bantoo Sehgal, and Martin E. Hemler Dana-Farber Cancer Institute and Department of Pathology, Harvard Medical School, Boston, MA 02115 he ␣31 integrin shows strong, stoichiometric, direct Brij 96–resistant) were independent of the QRD/TS151r lateral association with the tetraspanin CD151. As site, occurred late in biosynthesis, and involved mature T shown here, an extracellular CD151 site (QRD194–196) integrin subunits. Presence of the CD151–QRD194–196→INF is required for strong (i.e., Triton X-100–resistant) ␣31 mutant disrupted ␣3 and ␣6 integrin–dependent formation association and for maintenance of a key CD151 epitope of a network of cellular cables by Cos7 or NIH3T3 cells on (defined by monoclonal antibody TS151r) that is blocked basement membrane Matrigel and markedly altered cell upon ␣3 integrin association. Strong CD151 association spreading. These results provide definitive evidence that with integrin ␣61 also required the QRD194–196 site and strong lateral CD151–integrin association is functionally masked the TS151r epitope. For both ␣3 and ␣6 integrins, important, identify CD151 as a key player during ␣3 and strong QRD/TS151r-dependent CD151 association occurred ␣6 integrin–dependent matrix remodeling and cell spreading, early in biosynthesis and involved ␣ subunit precursor and support a model of CD151 as a transmembrane linker forms. In contrast, weaker associations of CD151 with itself, between extracellular integrin domains and intracellular integrins, or other tetraspanins (Triton X-100–sensitive but cytoskeleton/signaling molecules. -

Genome-Wide DNA Methylation Profiling Identifies Differential Methylation in Uninvolved Psoriatic Epidermis
Genome-Wide DNA Methylation Profiling Identifies Differential Methylation in Uninvolved Psoriatic Epidermis Deepti Verma, Anna-Karin Ekman, Cecilia Bivik Eding and Charlotta Enerbäck The self-archived postprint version of this journal article is available at Linköping University Institutional Repository (DiVA): http://urn.kb.se/resolve?urn=urn:nbn:se:liu:diva-147791 N.B.: When citing this work, cite the original publication. Verma, D., Ekman, A., Bivik Eding, C., Enerbäck, C., (2018), Genome-Wide DNA Methylation Profiling Identifies Differential Methylation in Uninvolved Psoriatic Epidermis, Journal of Investigative Dermatology, 138(5), 1088-1093. https://doi.org/10.1016/j.jid.2017.11.036 Original publication available at: https://doi.org/10.1016/j.jid.2017.11.036 Copyright: Elsevier http://www.elsevier.com/ Genome-Wide DNA Methylation Profiling Identifies Differential Methylation in Uninvolved Psoriatic Epidermis Deepti Verma*a, Anna-Karin Ekman*a, Cecilia Bivik Edinga and Charlotta Enerbäcka *Authors contributed equally aIngrid Asp Psoriasis Research Center, Department of Clinical and Experimental Medicine, Division of Dermatology, Linköping University, Linköping, Sweden Corresponding author: Charlotta Enerbäck Ingrid Asp Psoriasis Research Center, Department of Clinical and Experimental Medicine, Linköping University SE-581 85 Linköping, Sweden Phone: +46 10 103 7429 E-mail: [email protected] Short title Differential methylation in psoriasis Abbreviations CGI, CpG island; DMS, differentially methylated site; RRBS, reduced representation bisulphite sequencing Keywords (max 6) psoriasis, epidermis, methylation, Wnt, susceptibility, expression 1 ABSTRACT Psoriasis is a chronic inflammatory skin disease with both local and systemic components. Genome-wide approaches have identified more than 60 psoriasis-susceptibility loci, but genes are estimated to explain only one third of the heritability in psoriasis, suggesting additional, yet unidentified, sources of heritability. -
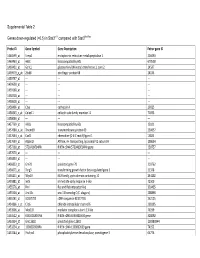
0.5) in Stat3∆/∆ Compared with Stat3flox/Flox
Supplemental Table 2 Genes down-regulated (<0.5) in Stat3∆/∆ compared with Stat3flox/flox Probe ID Gene Symbol Gene Description Entrez gene ID 1460599_at Ermp1 endoplasmic reticulum metallopeptidase 1 226090 1460463_at H60c histocompatibility 60c 670558 1460431_at Gcnt1 glucosaminyl (N-acetyl) transferase 1, core 2 14537 1459979_x_at Zfp68 zinc finger protein 68 24135 1459747_at --- --- --- 1459608_at --- --- --- 1459168_at --- --- --- 1458718_at --- --- --- 1458618_at --- --- --- 1458466_at Ctsa cathepsin A 19025 1458345_s_at Colec11 collectin sub-family member 11 71693 1458046_at --- --- --- 1457769_at H60a histocompatibility 60a 15101 1457680_a_at Tmem69 transmembrane protein 69 230657 1457644_s_at Cxcl1 chemokine (C-X-C motif) ligand 1 14825 1457639_at Atp6v1h ATPase, H+ transporting, lysosomal V1 subunit H 108664 1457260_at 5730409E04Rik RIKEN cDNA 5730409E04Rik gene 230757 1457070_at --- --- --- 1456893_at --- --- --- 1456823_at Gm70 predicted gene 70 210762 1456671_at Tbrg3 transforming growth factor beta regulated gene 3 21378 1456211_at Nlrp10 NLR family, pyrin domain containing 10 244202 1455881_at Ier5l immediate early response 5-like 72500 1455576_at Rinl Ras and Rab interactor-like 320435 1455304_at Unc13c unc-13 homolog C (C. elegans) 208898 1455241_at BC037703 cDNA sequence BC037703 242125 1454866_s_at Clic6 chloride intracellular channel 6 209195 1453906_at Med13l mediator complex subunit 13-like 76199 1453522_at 6530401N04Rik RIKEN cDNA 6530401N04 gene 328092 1453354_at Gm11602 predicted gene 11602 100380944 1453234_at -

4-6 Weeks Old Female C57BL/6 Mice Obtained from Jackson Labs Were Used for Cell Isolation
Methods Mice: 4-6 weeks old female C57BL/6 mice obtained from Jackson labs were used for cell isolation. Female Foxp3-IRES-GFP reporter mice (1), backcrossed to B6/C57 background for 10 generations, were used for the isolation of naïve CD4 and naïve CD8 cells for the RNAseq experiments. The mice were housed in pathogen-free animal facility in the La Jolla Institute for Allergy and Immunology and were used according to protocols approved by the Institutional Animal Care and use Committee. Preparation of cells: Subsets of thymocytes were isolated by cell sorting as previously described (2), after cell surface staining using CD4 (GK1.5), CD8 (53-6.7), CD3ε (145- 2C11), CD24 (M1/69) (all from Biolegend). DP cells: CD4+CD8 int/hi; CD4 SP cells: CD4CD3 hi, CD24 int/lo; CD8 SP cells: CD8 int/hi CD4 CD3 hi, CD24 int/lo (Fig S2). Peripheral subsets were isolated after pooling spleen and lymph nodes. T cells were enriched by negative isolation using Dynabeads (Dynabeads untouched mouse T cells, 11413D, Invitrogen). After surface staining for CD4 (GK1.5), CD8 (53-6.7), CD62L (MEL-14), CD25 (PC61) and CD44 (IM7), naïve CD4+CD62L hiCD25-CD44lo and naïve CD8+CD62L hiCD25-CD44lo were obtained by sorting (BD FACS Aria). Additionally, for the RNAseq experiments, CD4 and CD8 naïve cells were isolated by sorting T cells from the Foxp3- IRES-GFP mice: CD4+CD62LhiCD25–CD44lo GFP(FOXP3)– and CD8+CD62LhiCD25– CD44lo GFP(FOXP3)– (antibodies were from Biolegend). In some cases, naïve CD4 cells were cultured in vitro under Th1 or Th2 polarizing conditions (3, 4). -

Page 1 Supplemental Table I Upin WTVG Upin Humlowfb FAR1
Supplemental Table I UPinWTvG UPinHuMlowFB overlap FAR1 CD209 PLEKHO2 B2M IL27 GCLC CALR HMGN2P46 ME1 XPO1 CLEC1A NEK6 PDIA3 HSD17B14 TMEM106A SERPINH1 NSUN7 KCNJ15 PLEKHO2 SEMA6B SH3PXD2B HSPD1 BAALC RHOU SYVN1 CEACAM4 TGFBI DNAJB9 KATNAL2 CTSZ SLC25A19 CCDC175 SULF2 MHCII CARD14 P2RY6 MDN1 TDO2 CD74 GCLC FCAR HLA-DQB1 PTPN2 GLDN CD14 CHORDC1 MMP7 CSF2RB LOX CLEC5A MRC1 STIP1 ZMYND15 ITGAX BPIFB1 ITLN1 SLAMF7 ME1 DKK2 CD84 PDIA6 FAM124A FCGR2A HYOU1 F3 CLEC10A NLRC5 DZIP1L IFI30 NEK6 CECR6 CLEC4A SLC39A14 NDP CLEC7A TMEM106AFCGR1A TFEC KCNJ15 CCL7 C1QC SH3PXD2B CRABP2 C1QA RHOU PIPOX FOLR2 LRP2 CCL2 CH25H MVD VSIG4 C1QB TGFBI LINC01010 SIGLEC1 NFKB2 DPRXP4 CTSS C5 FAM20A CCR1 HSP90B1 ANKRD29 SLAMF8 ALDH18A1 OCSTAMP MS4A7 EDEM1 TGM2 HK3 CTSZ TM4SF19 CXCL10 C6 TRPV4 CTSK AACS CCL8 MSR1 PPA1 CCL1 STEAP4 PIK3R5 KCNE1 CXCL9 RASAL3 SLC9A7P1 MS4A6A DOCK11 CHI3L1 TIMP1 BHLHE40 LOC731424 CD209 HCLS1 DCSTAMP CCL7 FASN MSR1 PDCD1LG2 PDIA4 IL31RA CCL2 ITK CXCL3 CXCL2 CRELD2 TREM2 C15orf48 SFTPD MGST1 GPR84 BCL3 METTL7B CXCL5 SULF2 TMEM86A OCSTAMP CYP51A1 A2M SERPINA1 CREB3L1 AQP9 MMP12 DUSP2 NUPR1 CCL8 ADAM8 FHAD1 CCL24 P2RY6 YPEL4 FBP1 KCNAB2 FBP1 NA NFKBIE LOC100506585 NA FSCN1 CXCL16 NA MANF RAB13 NA SLC5A3 LOC391322 NA CTSC IL8 NA COTL1 MS4A4A NA HSPA5 SERPING1 NA MUC5B PLA2G4C NA CD74 CA12 NA HLA-DQB1 GBP1P1 NA SLC7A2 C11orf45 NA FABP5 ACVRL1 NA CIITA SPP1 NA RAB3IL1 TLN2 NA HSPE1 NDRG2 NA SCD C15orf48 NA ITIH4 KCNJ15 NA SERPINA3 MEIS3P1 NA LAG3 IL1RN NA FOXM1 HNMT NA CD14 CYP27B1 NA RRM2 CDCP1 NA ABCD2 FOLR2 NA FCRL2 ECM1 NA PDE3B ADAMDEC1 -

PRODUCT SPECIFICATION Anti-TSPAN3
Anti-TSPAN3 Product Datasheet Polyclonal Antibody PRODUCT SPECIFICATION Product Name Anti-TSPAN3 Product Number HPA015996 Gene Description tetraspanin 3 Clonality Polyclonal Isotype IgG Host Rabbit Antigen Sequence Recombinant Protein Epitope Signature Tag (PrEST) antigen sequence: NGTNPDAASRAIDYVQRQLHCCGIHNYSDWENTDWFKETKNQSVPLSCCR ETASNCNGSLAHPSDLYAEGCEALVVKKLQEI Purification Method Affinity purified using the PrEST antigen as affinity ligand Verified Species Human Reactivity Recommended IHC (Immunohistochemistry) Applications - Antibody dilution: 1:20 - 1:50 - Retrieval method: HIER pH6 ICC-IF (Immunofluorescence) - Fixation/Permeabilization: PFA/Triton X-100 - Working concentration: 0.25-2 µg/ml Characterization Data Available at atlasantibodies.com/products/HPA015996 Buffer 40% glycerol and PBS (pH 7.2). 0.02% sodium azide is added as preservative. Concentration Lot dependent Storage Store at +4°C for short term storage. Long time storage is recommended at -20°C. Notes Gently mix before use. Optimal concentrations and conditions for each application should be determined by the user. For protocols, additional product information, such as images and references, see atlasantibodies.com. Product of Sweden. For research use only. Not intended for pharmaceutical development, diagnostic, therapeutic or any in vivo use. No products from Atlas Antibodies may be resold, modified for resale or used to manufacture commercial products without prior written approval from Atlas Antibodies AB. Warranty: The products supplied by Atlas Antibodies are warranted to meet stated product specifications and to conform to label descriptions when used and stored properly. Unless otherwise stated, this warranty is limited to one year from date of sales for products used, handled and stored according to Atlas Antibodies AB's instructions. Atlas Antibodies AB's sole liability is limited to replacement of the product or refund of the purchase price. -

Complexes of Tetraspanins with Integrins: More Than Meets the Eye
COMMENTARY 4143 Complexes of tetraspanins with integrins: more than meets the eye Fedor Berditchevski CRC Institute for Cancer Studies, The University of Birmingham, Edgbaston, Birmingham, B15 2TA, UK Author for correspondence (e-mail: [email protected]) Journal of Cell Science 114, 4143-4151 (2001) © The Company of Biologists Ltd Summary The transmembrane proteins of the tetraspanin membrane, integrin-tetraspanin signalling complexes superfamily are implicated in a diverse range of biological are partitioned into specific microdomains proximal to phenomena, including cell motility, metastasis, cell cholesterol-rich lipid rafts. A substantial fraction of proliferation and differentiation. The tetraspanins are tetraspanins colocalise with integrins in various associated with adhesion receptors of the integrin family intracellular vesicular compartments. It is proposed that and regulate integrin-dependent cell migration. In cells tetraspanins can influence cell migration by one of the attached to the extracellular matrix, the integrin- following mechanisms: (1) modulation of integrin tetraspanin adhesion complexes are clustered into a distinct signalling; (2) compartmentalisation of integrins on the cell type of adhesion structure at the cell periphery. Various surface; or (3) direction of intracellular trafficking and tetraspanins are associated with phosphatidylinositol 4- recycling of integrins. kinase and protein kinase C isoforms, and they may facilitate assembly of signalling complexes by tethering these enzymes to integrin heterodimers. At the plasma Key words: Tetraspanin, Integrin, Migration, Signalling Introduction relatively well conserved among tetraspanins (Fig. 1). A Tetraspanins (also referred to as tetraspans or TM4SF proteins) combination of all the above features distinguishes tetraspanins are a family of widely expressed four-transmembrane-domain from a diverse group of proteins that have four transmembrane proteins. -

Downloaded 18 July 2014 with a 1% False Discovery Rate (FDR)
UC Berkeley UC Berkeley Electronic Theses and Dissertations Title Chemical glycoproteomics for identification and discovery of glycoprotein alterations in human cancer Permalink https://escholarship.org/uc/item/0t47b9ws Author Spiciarich, David Publication Date 2017 Peer reviewed|Thesis/dissertation eScholarship.org Powered by the California Digital Library University of California Chemical glycoproteomics for identification and discovery of glycoprotein alterations in human cancer by David Spiciarich A dissertation submitted in partial satisfaction of the requirements for the degree Doctor of Philosophy in Chemistry in the Graduate Division of the University of California, Berkeley Committee in charge: Professor Carolyn R. Bertozzi, Co-Chair Professor David E. Wemmer, Co-Chair Professor Matthew B. Francis Professor Amy E. Herr Fall 2017 Chemical glycoproteomics for identification and discovery of glycoprotein alterations in human cancer © 2017 by David Spiciarich Abstract Chemical glycoproteomics for identification and discovery of glycoprotein alterations in human cancer by David Spiciarich Doctor of Philosophy in Chemistry University of California, Berkeley Professor Carolyn R. Bertozzi, Co-Chair Professor David E. Wemmer, Co-Chair Changes in glycosylation have long been appreciated to be part of the cancer phenotype; sialylated glycans are found at elevated levels on many types of cancer and have been implicated in disease progression. However, the specific glycoproteins that contribute to cell surface sialylation are not well characterized, specifically in bona fide human cancer. Metabolic and bioorthogonal labeling methods have previously enabled enrichment and identification of sialoglycoproteins from cultured cells and model organisms. The goal of this work was to develop technologies that can be used for detecting changes in glycoproteins in clinical models of human cancer. -

Supp Table 6.Pdf
Supplementary Table 6. Processes associated to the 2037 SCL candidate target genes ID Symbol Entrez Gene Name Process NM_178114 AMIGO2 adhesion molecule with Ig-like domain 2 adhesion NM_033474 ARVCF armadillo repeat gene deletes in velocardiofacial syndrome adhesion NM_027060 BTBD9 BTB (POZ) domain containing 9 adhesion NM_001039149 CD226 CD226 molecule adhesion NM_010581 CD47 CD47 molecule adhesion NM_023370 CDH23 cadherin-like 23 adhesion NM_207298 CERCAM cerebral endothelial cell adhesion molecule adhesion NM_021719 CLDN15 claudin 15 adhesion NM_009902 CLDN3 claudin 3 adhesion NM_008779 CNTN3 contactin 3 (plasmacytoma associated) adhesion NM_015734 COL5A1 collagen, type V, alpha 1 adhesion NM_007803 CTTN cortactin adhesion NM_009142 CX3CL1 chemokine (C-X3-C motif) ligand 1 adhesion NM_031174 DSCAM Down syndrome cell adhesion molecule adhesion NM_145158 EMILIN2 elastin microfibril interfacer 2 adhesion NM_001081286 FAT1 FAT tumor suppressor homolog 1 (Drosophila) adhesion NM_001080814 FAT3 FAT tumor suppressor homolog 3 (Drosophila) adhesion NM_153795 FERMT3 fermitin family homolog 3 (Drosophila) adhesion NM_010494 ICAM2 intercellular adhesion molecule 2 adhesion NM_023892 ICAM4 (includes EG:3386) intercellular adhesion molecule 4 (Landsteiner-Wiener blood group)adhesion NM_001001979 MEGF10 multiple EGF-like-domains 10 adhesion NM_172522 MEGF11 multiple EGF-like-domains 11 adhesion NM_010739 MUC13 mucin 13, cell surface associated adhesion NM_013610 NINJ1 ninjurin 1 adhesion NM_016718 NINJ2 ninjurin 2 adhesion NM_172932 NLGN3 neuroligin -

Human Induced Pluripotent Stem Cell–Derived Podocytes Mature Into Vascularized Glomeruli Upon Experimental Transplantation
BASIC RESEARCH www.jasn.org Human Induced Pluripotent Stem Cell–Derived Podocytes Mature into Vascularized Glomeruli upon Experimental Transplantation † Sazia Sharmin,* Atsuhiro Taguchi,* Yusuke Kaku,* Yasuhiro Yoshimura,* Tomoko Ohmori,* ‡ † ‡ Tetsushi Sakuma, Masashi Mukoyama, Takashi Yamamoto, Hidetake Kurihara,§ and | Ryuichi Nishinakamura* *Department of Kidney Development, Institute of Molecular Embryology and Genetics, and †Department of Nephrology, Faculty of Life Sciences, Kumamoto University, Kumamoto, Japan; ‡Department of Mathematical and Life Sciences, Graduate School of Science, Hiroshima University, Hiroshima, Japan; §Division of Anatomy, Juntendo University School of Medicine, Tokyo, Japan; and |Japan Science and Technology Agency, CREST, Kumamoto, Japan ABSTRACT Glomerular podocytes express proteins, such as nephrin, that constitute the slit diaphragm, thereby contributing to the filtration process in the kidney. Glomerular development has been analyzed mainly in mice, whereas analysis of human kidney development has been minimal because of limited access to embryonic kidneys. We previously reported the induction of three-dimensional primordial glomeruli from human induced pluripotent stem (iPS) cells. Here, using transcription activator–like effector nuclease-mediated homologous recombination, we generated human iPS cell lines that express green fluorescent protein (GFP) in the NPHS1 locus, which encodes nephrin, and we show that GFP expression facilitated accurate visualization of nephrin-positive podocyte formation in -

Single-Cell Transcriptomics of Allo-Reactive CD4 T Cells Over Time
Single-cell transcriptomics of allo-reactive CD4+ T cells over time reveals divergent fates during gut GVHD Jessica A. Engel, … , Motoko Koyama, Ashraful Haque JCI Insight. 2020. https://doi.org/10.1172/jci.insight.137990. Research In-Press Preview Hematology Immunology Graphical abstract Find the latest version: https://jci.me/137990/pdf 1 Single-cell transcriptomics of allo-reactive CD4+ T cells over time reveals 2 divergent fates during gut GVHD. 3 4 Jessica A. Engel*1, Hyun Jae Lee*1, Cameron G. Williams*1, Rachel Kuns1, Stuart Olver1, 5 Lianne I. M. Lansink1, Megan S. F. Soon1, Stacey B. Andersen2, Joseph E. Powell3,4, Valentine 6 Svensson5, Sarah A. Teichmann6, Geoffrey R Hill1,7,8, Antiopi Varelias1, 9, Motoko Koyama7 7 and Ashraful Haque1,10. 8 9 Affiliations: 10 1QIMR Berghofer Medical Research Institute, Herston, Brisbane, Queensland 4006, Australia 11 2Institute for Molecular Bioscience, University of Queensland, St Lucia, Australia 12 3Garvan-Weizmann Centre for Cellular Genomics, Sydney, Australia. 13 4UNSW Cellular Genomics Futures Institute, University of New South Wales, Sydney, 14 Australia 15 5Flagship Labs 60 Inc, Cambridge, Mass, USA. 16 6Wellcome Sanger Institute, Wellcome Genome Campus, Hinxton, Cambridgeshire, UK 17 7Clinical Research Division, Fred Hutchinson Cancer Research Center, Seattle, WA 98109, 18 USA 19 8Division of Medical Oncology, University of Washington, Seattle, WA 98109, USA 20 9Faculty of Medicine, University of Queensland, St Lucia, Queensland, Australia 21 10Department of Microbiology and Immunology, University of Melbourne, located at The Peter 22 Doherty Institute for Infection and Immunity, 792 Elizabeth Street, Parkville, Victoria 3000, 23 Australia 24 25 *These authors contributed equally.