Treatment of Lipoedema Using Liposuction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WEIGHT HISTORY – WHQ Target Group: Sps 16+
NHANES 2017 6/3/16 Questionnaire: SP WEIGHT HISTORY – WHQ Target Group: SPs 16+ WHQ.010 These next questions ask about {your/SP's} height and weight at different times in {your/his/her} life. G/F/I/M/C How tall {are you/is SP} without shoes? |___| ENTER HEIGHT IN FEET AND INCHES ...... 1 ENTER HEIGHT IN METERS AND CENTIMETERS ........................... 2 REFUSED ..................................................... 7 (WHQ.025) DON’T KNOW ............................................... 9 (WHQ.025) |___|___| ENTER NUMBER OF FEET REFUSED ................................................. 7777 (WHQ.025) DON’T KNOW ........................................... 9999 (WHQ.025) AND |___|___| ENTER NUMBER OF INCHES DON’T KNOW ........................................... 9999 (WHQ.025) OR |___|___| ENTER NUMBER OF METERS REFUSED ................................................. 7777 (WHQ.025) DON’T KNOW ........................................... 9999 (WHQ.025) AND |___|___|___| ENTER NUMBER OF CENTIMETERS DON’T KNOW ........................................... 9999 (WHQ.025) Page 1 of 268 WHQ.025/ How much {do you/does SP} weigh without clothes or shoes? [If {you are/she is} currently pregnant, how much L/K did {you/she} weigh before your pregnancy?] RECORD CURRENT WEIGHT. ENTER WEIGHT IN POUNDS OR KILOGRAMS. CAPI INSTRUCTION: DISPLAY OPTIONAL SENTENCE [If {you are/she is} currently pregnant . .] ONLY IF SP IS FEMALE AND AGE IS 16 THROUGH 59. IF ITEM CHANGED, CHECK MEC COMPONENT. |___| ENTER WEIGHT IN POUNDS ...................... 1 ENTER WEIGHT IN KILOGRAMS ................ 2 REFUSED ..................................................... 7 (WHQ.030) DON’T KNOW ............................................... 9 (WHQ.030) |___|___|___| ENTER NUMBER OF POUNDS CAPI INSTRUCTION: SOFT EDIT 75-500, HARD EDIT 50-750 OR |___|___|___| ENTER NUMBER OF KILOGRAMS CAPI INSTRUCTION: SOFT EDIT 34-225, HARD EDIT 23-338 OR REFUSED ................................................ -

Adipose Tissue As Pain Generator in the Lower Back and Lower Extremity
Lee et al. HCA Healthcare Journal of Medicine (2020) 1:5 https://doi.org/10.36518/2689-0216.1102 Clinical Review Adipose Tissue as Pain Generator in the Lower Back and Lower Extremity: Application in Author affiliations are listed Musculoskeletal Medicine at the end of this article. Se Won Lee, MD ,1 Craig Van Dien, MD ,2 Sun Jae Won, MD, PhD3 Correspondence to: Se Won Lee, MD Abstract Department of Physical Medicine and Rehabilitation Description MoutainView Medical Adipose tissue (AT) has diverse and important functions in body insulation, mechanical protection, energy metabolism and the endocrine system. Despite its relative abundance in Center the human body, the clinical significance of AT in musculoskeletal (MSK) medicine, partic- 2880 N Tenaya Way, 2nd Fl, ularly its role in painful MSK conditions, is under-recognized. Pain associated with AT can Las Vegas, NV 89128 be divided into intrinsic (AT as a primary pain generator), extrinsic (AT as a secondary pain ([email protected]) generator) or mixed origin. Understanding AT as an MSK pain generator, both by mechanism and its specific role in pain generation by body region, enhances the clinical decision-making process and guides therapeutic strategies in patients with AT-related MSK disorders. This article reviews the existing literature of AT in the context of pain generation in the lower back and lower extremity to increase clinician awareness and stimulate further investigation into AT in MSK medicine. Keywords adipose tissue; fat pad; musculoskeletal pain; connective tissue; lipodystrophy; lipoma; obe- sity; lipedema; pain generator Introduction lower extremity, focusing on its pathogenic role Mounting evidence supports the various func- as a pain generator as well as practical diagno- tions of adipose tissue (AT), most notably its sis and management. -

Using Surgery to Remove Fat Has Long Been a Quest Of
I have these deposits offat where I really hate them, especially on my thighs. Dieting hasn't helped. -Ginny, 34, secretary sing surgery to remove fat has long been a quest of Ucosmetic surgeons, but the journey toward that dream has been slow until recently. About twenty years ago, physicians in Italy scraped out fat through a relatively small incision using a sharp, circular-ended knife called a curette. Because severe complications often resulted, this technique did not gain widespread acceptance. Seizing on that idea, doctors in France began using a blunt-ended canula, a metal tube with openings along the sides that looks a bit like an oversized straw, to remove fat more gently while preserving the important connections between the skin and muscle. This fat-removal method minimized the chances of damage to surrounding tissue. In a variation on the technique, doctors began infusing into the fat small amounts of saline (salt water), which was identical in composition to the water in our body. This helped break up the fat globules, making them easier to remove. © Copyright 2000, David J. Leffell. MD. All rights reserved. 172 Look Your Best After the technique was introduced to the United States in 1982, lipo suction rapidly gained popularity, though the potential for complications, many related mostly to the use of general anesthesia, remained. Three years later, American dermatologist Jeffrey Klein introduced tumescent anesthesia. The tumescent technique involves injecting low-concentration anesthetic solution (lidocaine) into the fat combined with epinephrine (to reduce bleeding and prolong the anesthetic effect) and saline. Large vol umes of this solution are injected into the fat before surgery, thus swelling the area to approximately two to three times its normal size. -

Childhood Obesity During the 1960S Are Available for Certain Age Groups
NATIONAL CENTER FOR HEALTH STATISTICS SEPTEMBER Health E-Stats 2018 Prevalence of Overweight, Obesity, and Severe Obesity Among Children and Adolescents Aged 2–19 Years: United States, 1963–1965 Through 2015–2016 by Cheryl D. Fryar, M.S.P.H., Margaret D. Carroll, M.S.P.H., and Cynthia L. Ogden, Ph.D., Division of Health and Nutrition Examination Surveys Results from the 2015–2016 National Health and Nutrition Examination Survey (NHANES), using measured heights and weights, indicate that an estimated 18.5% of U.S. children and adolescents aged 2–19 years have obesity, including 5.6% with severe obesity, and another 16.6% are overweight. Body mass index (BMI), expressed as weight in kilograms divided by height in meters squared (kg/m2), is commonly used to classify obesity among adults and is also recommended for use with children and adolescents. Cutoff criteria are based on the sex-specific BMI-for-age 2000 CDC Growth Charts for the United States (available from: https://www.cdc.gov/growthcharts/cdc_charts.htm). Based on current recommendations from expert committees, children and adolescents with BMI values at or above the 95th percentile of the growth charts are categorized as having obesity. This differs from previous years in which children and adolescents above this cutoff were categorized as overweight. This change in terminology reflects the category labels used by organizations such as the National Academy of Medicine and the American Academy of Pediatrics. For more information, see “Changes in Terminology for Childhood Overweight and Obesity,” available from: https://www.cdc.gov/nchs/data/nhsr/nhsr025.pdf. -
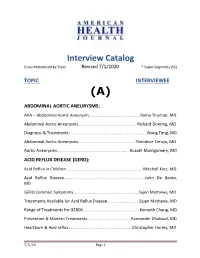
AHJ Interview Catalog 7-1-13(9)
Interview Catalog Cross Referenced by Topic Revised 7/1/2020 * Super Segments (SS) TOPIC INTERVIEWEE (A) ABDOMINAL AORTIC ANEURYSMS: AAA – Abdominal Aortic Aneurysm………………………………………….Rama Thumati, MD Abdominal Aortic Aneurysms………………………………………………..Richard Doering, MD Diagnosis & Treatments…………………………………………………………..…...Wang Teng, MD Abdominal Aortic Aneurysms……………………………………………...Theodore Teruya, MD Aortic Aneurysms...............................................................Russell Montgomery, MD ACID REFLUX DISEASE (GERD): Acid Reflux in Children...................................................................Mitchell Katz, MD Acid Reflux Disease……………………………………………………………….….John De Banto, MD GERD Common Symptoms……………………………………………………..Sajen Mathews, MD Treatments Available for Acid Reflux Disease............................Sajen Mathews, MD Range of Treatments for GERDS.................................................Kenneth Chang, MD Prevention & Modern Treatments......................................Parminder Dhaliwal, MD Heartburn & Acid reflux………...............................................Christopher Hurley, MD 7/1/20 Page 1 ACL TEAR (ANTERIOR CRUCIATE LIGAMENT TEAR) ACL Tear/Injuries‐Female Atheletes Prevention....................John A. Schlechter, DO ACNE: Acne……………………………………………………………………………….Sharon Christopher, PA‐C Best Methods of Treating Acne.……………………………………………Gene Rubinstein, MD Flaxel Repair Laser (Part 1)………………………………………………………Michael Persky, MD Flaxel Laser/Recovery & Results (Part 2)………………………………….Michael Persky, MD ACUPUNCTURE: -
Underweight Vs. Overweight/Obese: Which Weight Category Do We Prefer? Dissociation of Weight#Related Preferences at the Explicit and Implicit Level
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Harvard University - DASH Underweight vs. overweight/obese: which weight category do we prefer? Dissociation of weight#related preferences at the explicit and implicit level The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Marini, M. 2017. “Underweight vs. overweight/obese: which weight category do we prefer? Dissociation of weight#related preferences at the explicit and implicit level.” Obesity Science & Practice 3 (4): 390-398. doi:10.1002/osp4.136. http://dx.doi.org/10.1002/osp4.136. Published Version doi:10.1002/osp4.136 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:34651998 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA Obesity Science & Practice doi: 10.1002/osp4.136 ORIGINAL ARTICLE Underweight vs. overweight/obese: which weight category do we prefer? Dissociation of weight-related preferences at the explicit and implicit level M. Marini1,2,3, 1Center for Translational Neurophysiology, Summary Istituto Italiano di Tecnologia, Ferrara, Italy; Objective 2Department of Neurobiology, Harvard Medical School, Boston, MA, USA; 3Department of Psychology, Harvard Although stigma towards obesity and anorexia is a well-recognized problem, no research University, Cambridge, MA, USA has investigated and compared the explicit (i.e. conscious) and implicit (i.e. unconscious) preferences between these two conditions. -

I UNIVERSITY of CALIFORNIA SAN DIEGO the Weight of Medical
UNIVERSITY OF CALIFORNIA SAN DIEGO The Weight of Medical Authority: The Making and Unmaking of Knowledge in the Obesity Epidemic A dissertation submitted in partial satisfaction of the requirements for the degree Doctor of Philosophy in Sociology (Science Studies) by Julia Rogers Committee in charge: Professor Martha Lampland, Chair Professor Cathy Gere Professor Isaac Martin Professor David Serlin Professor Charles Thorpe 2018 i Copyright Julia Ellen Rogers, 2018 All Rights Reserved ii The Dissertation of Julia Ellen Rogers is approved, and it is acceptable in quality and form for publication on microfilm and electronically: _____________________________________________________________ _____________________________________________________________ _____________________________________________________________ _____________________________________________________________ _____________________________________________________________ Chair University of California San Diego 2018 iii DEDICATION For Eric and Anderson iv TABLE OF CONTENTS Signature Page………………………………………………………………………………iii Dedication ............................................................................................................................... iv Table of Contents ..................................................................................................................... v List of Figures and Tables ....................................................................................................... xi Vita ....................................................................................................................................... -

July 14, 2019 the Honorable Jan
July 14, 2019 The Honorable Jan Schakowsky 2367 Rayburn HOB Washington, DC 20515 Dear Representative Schakowsky: On behalf of University of Pennsylvania Department of Physical Medicine and Rehabilitation, I’m writing to inform you that we would like to offer our formal endorsement of the Lymphedema Treatment Act (S.518/H.R.1948). I am a practicing cancer physiatrist at Penn Medicine and frequently evaluate, diagnose, and manage lymphedema. Many of my patients have lymphedema as a result of cancer treatment, while others have lymphedema as a result of congenital lymphedema, Milroy’s disease, Klippel-Trenaunay Syndrome, lipedema, organ transplantation, chronic venous insufficiency, or trauma. Despite the cause of lymphedema, the international standard of care for treatment includes lymphedema therapy and long term use of compression garments that at a minimum needs to be replaced every 6 months. Lymphedema is a life-long condition that requires ongoing medical management along with continuous compression. The current international standard of care for lymphedema requires use of appropriate compression on a 24-hour basis. Failure to provide adequate compression can lead to significant medical, psychological and functional morbidity. Specifically, patients are left vulnerable to worsening lymphedema, potentially life- threatening cellulitis infections, chronic pain and non-healing wounds. Unfortunately, Medicare currently does not cover these medically necessary compression garments, despite the evidence for the increase in morbidity and mortality associated with untreated lymphedema and the international standard of care to treat with 24-hour compression garments. Furthermore, many patients are unable to financially afford the costs of compression garments that can be several hundred dollars a year. -

Surgical Treatments for Lymphedema and Lipedema BACKGROUND
Name of Blue Advantage Policy: Surgical Treatments for Lymphedema and Lipedema Policy #:719 Latest Review Date: September 2020 Category: Medical/Surgical Policy Grade: B BACKGROUND: Blue Advantage medical policy does not conflict with Local Coverage Determinations (LCDs), Local Medical Review Policies (LMRPs) or National Coverage Determinations (NCDs) or with coverage provisions in Medicare manuals, instructions or operational policy letters. In order to be covered by Blue Advantage the service shall be reasonable and necessary under Title XVIII of the Social Security Act, Section 1862(a)(1)(A). The service is considered reasonable and necessary if it is determined that the service is: 1. Safe and effective; 2. Not experimental or investigational*; 3. Appropriate, including duration and frequency that is considered appropriate for the service, in terms of whether it is: • Furnished in accordance with accepted standards of medical practice for the diagnosis or treatment of the patient’s condition or to improve the function of a malformed body member; • Furnished in a setting appropriate to the patient’s medical needs and condition; • Ordered and furnished by qualified personnel; • One that meets, but does not exceed, the patient’s medical need; and • At least as beneficial as an existing and available medically appropriate alternative. *Routine costs of qualifying clinical trial services with dates of service on or after September 19, 2000 which meet the requirements of the Clinical Trials NCD are considered reasonable and necessary by Medicare. Providers should bill Original Medicare for covered services that are related to clinical trials that meet Medicare requirements (Refer to Medicare National Coverage Determinations Manual, Chapter 1, Section 310 and Medicare Claims Processing Manual Chapter 32, Sections 69.0-69.11). -
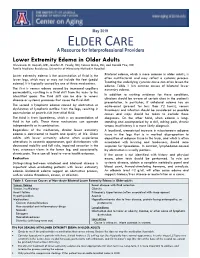
Lower Extremity Edema.Pdf
May 2019 ELDER CARE A Resource for Interprofessional Providers Lower Extremity Edema in Older Adults Oluwaseun O. Acquah, MD, Jennifer M. Vesely, MD, Teresa Quinn, MD, and Donald Pine, MD Family Medicine Residency, University of Minnesota Methodist Hospital Lower extremity edema is the accumulation of fluid in the Bilateral edema, which is more common in older adults, is lower legs, which may or may not include the feet (pedal often multifactorial and may reflect a systemic process. edema). It is typically caused by one of three mechanisms. Treating the underlying systemic cause can often lessen the edema. Table 1 lists common causes of bilateral lower The first is venous edema caused by increased capillary extremity edema. permeability, resulting in a fluid shift from the veins to the interstitial space. The fluid shift can be due to venous In addition to seeking evidence for these conditions, disease or systemic processes that cause the fluid shift. clinicians should be aware of certain clues in the patient’s presentation. In particular, if unilateral edema has an The second is lymphatic edema caused by obstruction or acute-onset (present for less than 72 hours), venous dysfunction of lymphatic outflow from the legs, resulting in thrombosis and infection should be considered as possible accumulation of protein-rich interstitial fluid. causes and steps should be taken to exclude those The third is from lipoedema, which is an accumulation of diagnoses. On the other hand, when edema is long- fluid in fat cells. These three mechanisms can operate standing and accompanied by a dull, aching pain, chronic independently or in combination. -
Sakakawea Dispatch
Winter 2018-2019 Sakakawea Medical Center Sakakawea Dispatch Inside this issue: This institution is an equal opportunity provider. CCCHC Providers 2 Construction 3 Update for CCCHC Darrold Bertsch, SMC CEO Receives Grassroots Champion Award Emergency 4 Department Each year, the American Hospital Association (AHA), in conjunction with the state hospital associations, recognizes the achievements of grassroots Triage 4 leaders with the prestigious Grassroots Champion Award. One hospital Charity Care 4 leader from each state is honored for his or her work over the previous year in effectively delivering the hospital message to elected officials; Lymphedema helping to broaden the base of community support for hospitals; and 5 Program advocating tirelessly on behalf of patients, hospitals and communities. Patient Satisfaction 5 The American Hospital Association in conjunction with the North Dakota Surveys State Hospital Association named Sakakawea Medical Center, CEO, Stop the Bleed 6 Darrold Bertsch as the 2018 Grassroots Champion. Bertsch earned this special recognition through his dedication to the hospital mission, on both Welcome the local and the national level. 7 Dr. Fogarty Mr. Bertsch was recognized during the during the AHA annual meeting and Tobacco Cessation 7 was presented with the award during the North Dakota Hospital Association annual conference that was held in Fargo, North Dakota. Visiting Specialists 8 Darrold Bertsch, CEO of Sakakawea Medical Center SMC and Jen Porter, American Hospital Association’s Regional Executive for Region 6 How to contact us: Sakakawea Medical Center 510 8th Ave NE Hazen, ND 58545 Phone: 701.748.2225 Fax: 701.748.5757 Visit www.aha.org for more information. -

Refining the Abdominoplasty for Better Patient Outcomes
Refining the Abdominoplasty for Better Patient Outcomes Karol A Gutowski, MD, FACS Private Practice University of Illinois & University of Chicago Refinements • 360o assessment & treatment • Expanded BMI inclusion • Lipo-abdominoplasty • Low scar • Long scar • Monsplasty • No “dog ears” • No drains • Repurpose the fat • Rapid recovery protocols (ERAS) What I Do and Don’t Do • “Standard” Abdominoplasty is (almost) dead – Does not treat the entire trunk – Fat not properly addressed – Problems with lateral trunk contouring – Do it 1% of cases • Solution: 360o Lipo-Abdominoplasty – Addresses entire trunk and flanks – No Drains & Rapid Recovery Techniques Patient Happy, I’m Not The Problem: Too Many Dog Ears! Thanks RealSelf! Take the Dog (Ear) Out! Patients Are Telling Us What To Do Not enough fat removed Not enough skin removed Patient Concerns • “Ideal candidate” by BMI • Pain • Downtime • Scar – Too high – Too visible – Too long • Unnatural result – Dog ears – Mons aesthetics Solutions • “Ideal candidate” by BMI Extend BMI range • Pain ERAS protocols + NDTT • Downtime ERAS protocols + NDTT • Scar Scar planning – Too high Incision markings – Too visible Scar care – Too long Explain the need • Unnatural result Technique modifications – Dog ears Lipo-abdominoplasty – Mons aesthetics Mons lift Frequent Cause for Reoperation • Lateral trunk fullness – Skin (dog ear), fat, or both • Not addressed with anterior flank liposuction alone – need posterior approach • Need a 360o approach with extended skin excision (Extended Abdominoplasty) • Patient