Lower Extremity Edema.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Adipose Tissue As Pain Generator in the Lower Back and Lower Extremity
Lee et al. HCA Healthcare Journal of Medicine (2020) 1:5 https://doi.org/10.36518/2689-0216.1102 Clinical Review Adipose Tissue as Pain Generator in the Lower Back and Lower Extremity: Application in Author affiliations are listed Musculoskeletal Medicine at the end of this article. Se Won Lee, MD ,1 Craig Van Dien, MD ,2 Sun Jae Won, MD, PhD3 Correspondence to: Se Won Lee, MD Abstract Department of Physical Medicine and Rehabilitation Description MoutainView Medical Adipose tissue (AT) has diverse and important functions in body insulation, mechanical protection, energy metabolism and the endocrine system. Despite its relative abundance in Center the human body, the clinical significance of AT in musculoskeletal (MSK) medicine, partic- 2880 N Tenaya Way, 2nd Fl, ularly its role in painful MSK conditions, is under-recognized. Pain associated with AT can Las Vegas, NV 89128 be divided into intrinsic (AT as a primary pain generator), extrinsic (AT as a secondary pain ([email protected]) generator) or mixed origin. Understanding AT as an MSK pain generator, both by mechanism and its specific role in pain generation by body region, enhances the clinical decision-making process and guides therapeutic strategies in patients with AT-related MSK disorders. This article reviews the existing literature of AT in the context of pain generation in the lower back and lower extremity to increase clinician awareness and stimulate further investigation into AT in MSK medicine. Keywords adipose tissue; fat pad; musculoskeletal pain; connective tissue; lipodystrophy; lipoma; obe- sity; lipedema; pain generator Introduction lower extremity, focusing on its pathogenic role Mounting evidence supports the various func- as a pain generator as well as practical diagno- tions of adipose tissue (AT), most notably its sis and management. -
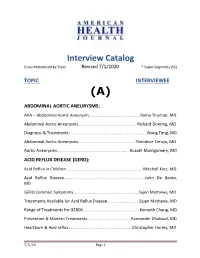
AHJ Interview Catalog 7-1-13(9)
Interview Catalog Cross Referenced by Topic Revised 7/1/2020 * Super Segments (SS) TOPIC INTERVIEWEE (A) ABDOMINAL AORTIC ANEURYSMS: AAA – Abdominal Aortic Aneurysm………………………………………….Rama Thumati, MD Abdominal Aortic Aneurysms………………………………………………..Richard Doering, MD Diagnosis & Treatments…………………………………………………………..…...Wang Teng, MD Abdominal Aortic Aneurysms……………………………………………...Theodore Teruya, MD Aortic Aneurysms...............................................................Russell Montgomery, MD ACID REFLUX DISEASE (GERD): Acid Reflux in Children...................................................................Mitchell Katz, MD Acid Reflux Disease……………………………………………………………….….John De Banto, MD GERD Common Symptoms……………………………………………………..Sajen Mathews, MD Treatments Available for Acid Reflux Disease............................Sajen Mathews, MD Range of Treatments for GERDS.................................................Kenneth Chang, MD Prevention & Modern Treatments......................................Parminder Dhaliwal, MD Heartburn & Acid reflux………...............................................Christopher Hurley, MD 7/1/20 Page 1 ACL TEAR (ANTERIOR CRUCIATE LIGAMENT TEAR) ACL Tear/Injuries‐Female Atheletes Prevention....................John A. Schlechter, DO ACNE: Acne……………………………………………………………………………….Sharon Christopher, PA‐C Best Methods of Treating Acne.……………………………………………Gene Rubinstein, MD Flaxel Repair Laser (Part 1)………………………………………………………Michael Persky, MD Flaxel Laser/Recovery & Results (Part 2)………………………………….Michael Persky, MD ACUPUNCTURE: -

July 14, 2019 the Honorable Jan
July 14, 2019 The Honorable Jan Schakowsky 2367 Rayburn HOB Washington, DC 20515 Dear Representative Schakowsky: On behalf of University of Pennsylvania Department of Physical Medicine and Rehabilitation, I’m writing to inform you that we would like to offer our formal endorsement of the Lymphedema Treatment Act (S.518/H.R.1948). I am a practicing cancer physiatrist at Penn Medicine and frequently evaluate, diagnose, and manage lymphedema. Many of my patients have lymphedema as a result of cancer treatment, while others have lymphedema as a result of congenital lymphedema, Milroy’s disease, Klippel-Trenaunay Syndrome, lipedema, organ transplantation, chronic venous insufficiency, or trauma. Despite the cause of lymphedema, the international standard of care for treatment includes lymphedema therapy and long term use of compression garments that at a minimum needs to be replaced every 6 months. Lymphedema is a life-long condition that requires ongoing medical management along with continuous compression. The current international standard of care for lymphedema requires use of appropriate compression on a 24-hour basis. Failure to provide adequate compression can lead to significant medical, psychological and functional morbidity. Specifically, patients are left vulnerable to worsening lymphedema, potentially life- threatening cellulitis infections, chronic pain and non-healing wounds. Unfortunately, Medicare currently does not cover these medically necessary compression garments, despite the evidence for the increase in morbidity and mortality associated with untreated lymphedema and the international standard of care to treat with 24-hour compression garments. Furthermore, many patients are unable to financially afford the costs of compression garments that can be several hundred dollars a year. -

Surgical Treatments for Lymphedema and Lipedema BACKGROUND
Name of Blue Advantage Policy: Surgical Treatments for Lymphedema and Lipedema Policy #:719 Latest Review Date: September 2020 Category: Medical/Surgical Policy Grade: B BACKGROUND: Blue Advantage medical policy does not conflict with Local Coverage Determinations (LCDs), Local Medical Review Policies (LMRPs) or National Coverage Determinations (NCDs) or with coverage provisions in Medicare manuals, instructions or operational policy letters. In order to be covered by Blue Advantage the service shall be reasonable and necessary under Title XVIII of the Social Security Act, Section 1862(a)(1)(A). The service is considered reasonable and necessary if it is determined that the service is: 1. Safe and effective; 2. Not experimental or investigational*; 3. Appropriate, including duration and frequency that is considered appropriate for the service, in terms of whether it is: • Furnished in accordance with accepted standards of medical practice for the diagnosis or treatment of the patient’s condition or to improve the function of a malformed body member; • Furnished in a setting appropriate to the patient’s medical needs and condition; • Ordered and furnished by qualified personnel; • One that meets, but does not exceed, the patient’s medical need; and • At least as beneficial as an existing and available medically appropriate alternative. *Routine costs of qualifying clinical trial services with dates of service on or after September 19, 2000 which meet the requirements of the Clinical Trials NCD are considered reasonable and necessary by Medicare. Providers should bill Original Medicare for covered services that are related to clinical trials that meet Medicare requirements (Refer to Medicare National Coverage Determinations Manual, Chapter 1, Section 310 and Medicare Claims Processing Manual Chapter 32, Sections 69.0-69.11). -
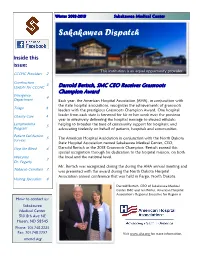
Sakakawea Dispatch
Winter 2018-2019 Sakakawea Medical Center Sakakawea Dispatch Inside this issue: This institution is an equal opportunity provider. CCCHC Providers 2 Construction 3 Update for CCCHC Darrold Bertsch, SMC CEO Receives Grassroots Champion Award Emergency 4 Department Each year, the American Hospital Association (AHA), in conjunction with the state hospital associations, recognizes the achievements of grassroots Triage 4 leaders with the prestigious Grassroots Champion Award. One hospital Charity Care 4 leader from each state is honored for his or her work over the previous year in effectively delivering the hospital message to elected officials; Lymphedema helping to broaden the base of community support for hospitals; and 5 Program advocating tirelessly on behalf of patients, hospitals and communities. Patient Satisfaction 5 The American Hospital Association in conjunction with the North Dakota Surveys State Hospital Association named Sakakawea Medical Center, CEO, Stop the Bleed 6 Darrold Bertsch as the 2018 Grassroots Champion. Bertsch earned this special recognition through his dedication to the hospital mission, on both Welcome the local and the national level. 7 Dr. Fogarty Mr. Bertsch was recognized during the during the AHA annual meeting and Tobacco Cessation 7 was presented with the award during the North Dakota Hospital Association annual conference that was held in Fargo, North Dakota. Visiting Specialists 8 Darrold Bertsch, CEO of Sakakawea Medical Center SMC and Jen Porter, American Hospital Association’s Regional Executive for Region 6 How to contact us: Sakakawea Medical Center 510 8th Ave NE Hazen, ND 58545 Phone: 701.748.2225 Fax: 701.748.5757 Visit www.aha.org for more information. -

Lipedema Intake Form
Lipedema Intake Form (Please complete in addition to a complete health history) Personal Information Name Do you sit for long periods at a work, home or DOB while driving? Yes No Have you been formally diagnosed with lipedema? If yes, please tell me more: Yes No Does someone else in your family have Lipedema? Do you experience stress? Yes No Yes No If yes, please tell me more: Have you been evaluated by an expert? Endocrinologist Yes No Does your stress result in any of these symptoms? Vascular Specialist Yes No (circle all that apply) Nutritionist Yes No muscle tension / anxiety / insomnia / irritability / other Physical Therapy for functional improvement - Is there a particular area of the body where you are (balance and movement) Yes No experiencing tension, stiffness, pain or other discomfort? Psychotherapist Yes No Yes No Other Yes No If yes, please tell me more: Tell me more: Are you experiencing discomfort in your body? Yes No What treatments have you tried in the past? How well did they work? If yes, please tell me more: Tell me more: Do you suffer from chronic pain? Yes No Are you currently under medical supervision for If yes, please tell me more: lipedema, lymphedema or any other condition? Yes No Do you have areas of swelling and/or inflammation? Yes No If yes, please tell me more: If yes, please tell me more: Do you exercise regularly? Yes No Have you had a recent injury or surgery? Yes No If yes, please tell me more: If yes, please tell me more: Do you perform any repetitive movement in your work or at home? Yes No Do you -

MR Imaging of the Lymphatic System in Patients with Lipedema and Lipo-Lymphedema
Microvascular Research 77 (2009) 335–339 Contents lists available at ScienceDirect Microvascular Research journal homepage: www.elsevier.com/locate/ymvre Regular Article MR imaging of the lymphatic system in patients with lipedema and lipo-lymphedema Christian Lohrmann a,⁎, Etelka Foeldi b, Mathias Langer a a Department of Radiology, University Hospital of Freiburg, Hugstetter Strasse 55, D-79106, Freiburg i. Br., Germany b Foeldi Clinic for Lymphology, Hinterzarten, Röβlehofweg 2-6, D-79856, Hinterzarten, Germany article info abstract Article history: Objective: To assess for the first time the morphology of the lymphatic system in patients with lipedema and Received 30 October 2008 lipo-lymphedema of the lower extremities by MR lymphangiography. Revised 15 January 2009 Materials and methods: 26 lower extremities in 13 consecutive patients (5 lipedema, 8 lipo-lymphedema) Accepted 15 January 2009 were examined by MR lymphangiography. 18 mL of gadoteridol and 1 mL of mepivacainhydrochloride 1% Available online 27 January 2009 were subdivided into 10 portions and injected intracutaneously in the forefoot. MR imaging was performed with a 1.5-T system equipped with high-performance gradients. For MR lymphangiography, a 3D-spoiled Keywords: Lipedema gradient-echo sequence was used. For evaluation of the lymphedema a heavily T2-weighted 3D-TSE Lipo-lymphedema sequence was performed. MRI Results: In all 16 lower extremities (100%) with lipo-lymphedema, high signal intensity areas in the epifascial Lymphangiography region could be detected on the 3D-TSE sequence. In the 16 examined lower extremities with lipo- Microcirculation lymphedema, 8 lower legs and 3 upper legs demonstrated enlarged lymphatic vessels up to a diameter of 3 mm. -

Best Practice Guidelines
WUK BPG Best Practice Guidelines Te management of lipoedema 2017 Diagnosis and assessment Lipoedema management Life style support and self care Compression therapy Non-surgical and surgical interventions BEST PRACTICE GUIDELINES: EXPERT WORKING GROUP: THE MANAGEMENT OF Tanya Coppel, Specialist Lymphoedema Physiotherapist, LIPOEDEMA Belfast Health & Social Care Trust, Belfast PUBLISHED BY: Julie Cunneen, Macmillan Clinical Lead for Wounds UK Lymphoedema Service/Nurse Consultant, Moseley Hall Hospital, Birmingham A division of Omniamed, 1.01 Cargo Works Sharie Fetzer, Chair, Lipoedema UK, London 1–2 Hatfields, London SE1 9PG, UK Tel: +44 (0)203735 8244 Kristiana Gordon, Consultant in Dermatology and Web: www.wounds-uk.com Lymphovascular Medicine, St George’s Hospital, London Denise Hardy, Lymphoedema/Lipoedema Nurse Consultant, Kendal Lymphology Centre, Kendal, Cumbria; Nurse Adviser, Lipoedema UK/ Lymphoedema Support Network (LSN), Cumbria; Co- Chair of the Expert Working Group © Wounds UK, March 2017 Tis document has been developed Kris Jones, Patient; Joint Managing Director & Nurse by Wounds UK and is supported byActiva Healthcare, BSN Consultant, LymphCare UK; Nurse Consultant, Medical, Haddenham Healthcare, Lipoedema UK Lipoedema UK, medi UK, Sigvaris and Talk Lipoedema. Angela McCarroll, Trustee, Talk Lipoedema; Patient, Northern Ireland Caitriona O’Neill, Lymphoedema Care Lead Nurse, Accelerate CIC, London Sara Smith, Senior Lecturer in Dietetics and Nutrition, Queen Margaret University, Edinburgh Cheryl White, Lymphoedema Specialist -

Lymph/Lipoedema Treatment in Its Different Approaches
Lymph/lipoedema treatment in its different approaches Prelims.indd 1 6/4/09 18:26:08 The views expressed in this book reflect the experience of the authors and are not necessarily those of Wounds UK or BSN-Jobst GmbH. The authors have made every effort to ensure the accuracy of drug dosage and other information contained in this book. However, this does not diminish the requirement to exercise clinical judgement, and the authors and publisher cannot accept responsibility for the use of the information in clinical practice. Any products referred to by the authors should only be used as recommended in the manufacturers’ data sheets. Prelims.indd 2 6/4/09 18:26:08 Lymph/lipoedema treatment in its different approaches 1st Jobst® Scientific Symposium, 2008 Prelims.indd 3 6/4/09 18:26:09 Sound Recording: AP Technik, Andreas Peeck Beschallung und Veranstaltungsmanagement Hoher Weg 30 D-46446 Emmerich am Rhein www.soundlight-events.com Wounds UK, a subsidiary of HealthComm UK Limited, Suite 3.1, 36 Upperkirkgate, Aberdeen AB10 1BA British Library Cataloguing-in-Publication Data A catalogue record is available for this book © BSN-Jobst GmbH, 2009 ISBN-10 0-95555758-6-9 ISBN-13 978-0-9555758-6-0 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without prior permission from the publishers Printed in the UK by WACE Corporate Print Limited, Swindon, Wiltshire SN3 4FH Prelims.indd 4 6/4/09 18:26:09 Contents Contributors ...................................................................................................................................................................................... -

Genetics of Lipedema: New Perspectives on Genetic Research and Molecular Diagnoses S
European Review for Medical and Pharmacological Sciences 2019; 23: 5581-5594 Genetics of lipedema: new perspectives on genetic research and molecular diagnoses S. PAOLACCI1, V. PRECONE2, F. ACQUAVIVA3, P. CHIURAZZI4,5, E. FULCHERI6,7, M. PINELLI3,8, F. BUFFELLI9,10, S. MICHELINI11, K.L. HERBST12, V. UNFER13, M. BERTELLI2; GENEOB PROJECT 1MAGI’S LAB, Rovereto (TN), Italy 2MAGI EUREGIO, Bolzano, Italy 3Department of Translational Medicine, Section of Pediatrics, Federico II University, Naples, Italy 4Istituto di Medicina Genomica, Fondazione A. Gemelli, Università Cattolica del Sacro Cuore, Rome, Italy 5UOC Genetica Medica, Fondazione Policlinico Universitario “A. Gemelli” IRCCS, Rome, Italy 6Fetal and Perinatal Pathology Unit, IRCCS Istituto Giannina Gaslini, Genoa, Italy 7Department of Integrated Surgical and Diagnostic Sciences, University of Genoa, Genoa, Italy 8Telethon Institute of Genetics and Medicine (TIGEM), Pozzuoli, Italy 9Fetal and Perinatal Pathology Unit, IRCCS Istituto Giannina Gaslini, Genoa, Italy 10Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics and Maternal-Infantile Sciences, University of Genoa, Genoa, Italy 11Department of Vascular Rehabilitation, San Giovanni Battista Hospital, Rome, Italy 12Department of Medicine, University of Arizona, Tucson, AZ, USA 13Department of Developmental and Social Psychology, Faculty of Medicine and Psychology, Sapienza University of Rome, Rome, Italy Abstract. – OBJECTIVE: The aim of this quali- Introduction tative review is to provide an update on the cur- rent understanding of the genetic determinants of lipedema and to develop a genetic test to dif- Lipedema is an underdiagnosed chronic debil- ferentiate lipedema from other diagnoses. itating disease characterized by bruising and pain MATERIALS AND METHODS: An electronic and excess of subcutaneous adipose tissue of the search was conducted in MEDLINE, PubMed, and legs and/or arms in women during or after times Scopus for articles published in English up to of hormone change, especially in puberty1. -

81B High-Volume-Liposuction-...Pdf
doi:10.36849/JDD.2021.5828 March 2021 Volume 20 • Issue 3 Copyright © 2021 ORIGINAL ARTICLE Journal of Drugs in Dermatology SPECIAL TOPIC High Volume Liposuction in Tumescence Anesthesia in Lipedema Patients: A Retrospective Analysis Matthias Sandhofer MD,a Victoria Hofer, a,b Martina Sandhofer,a Mindt Sonani,c Werner Moosbauer,a,d Martin Barscha aDermatologie Zentrum für Haut, Ästhetik, Laser, Venen, Praxis Dr. Matthias Sandhofer/Dr. Martin Barsch; Austrian Center for Lipedema, Wien/Linz, Austria bDanube Private University, Faculty of Medicine/Dental Medicine, Krems-Stein, Austria cInstitute for Clinical Chemistry, University Hospital Mannheim, Mannheim, Germany dKepler Universitätsklinikum GmbH, Anästhesiologie und Operative Intensivmedizin, Linz, Austria ABSTRACT Background: Lipedema is a chronic, progressive disease that occurs almost exclusively in women and leads to pathological, painful fat growths at the extremities. Only symptomatic therapy can be offered since the etiology of the disease has not yet been clarified. Liposuction in tumescent anesthesia has established itself as a surgical treatment method of choice. The complication rate associated with the procedure and the pharmacological course and safety of treatment in patients with lipedema has not yet been sufficiently studied. The aim of the study was to broaden the evidence on the safety of ambulatory high-volume liposuction in tumescent anesthesia in lipedema patients. Influencing factors of patients (weight, fat content, comorbidities) or the process technique (drug administration, volume of aspirates) should be investigated on the safety and risks of tumescent anesthesia. This was a retrospective data analysis in which data from 27 patients (40 liposuction procedures) treated at the Sandhofer and Barsch lipedema center between 2016 and 2018 were evaluated. -

Lymphedema, Lipedema and Nutrition
LYMPHEDEMA, LIPEDEMA AND NUTRITION THE ILF CONFERENCE, CHICAGO, IL PAULA JB STEWART MS, MD, CLT-LANA JUNE 15TH, 2019 NO FINANCIAL IMPLICATIONS OR DISCLOSURES FOR THIS PRESENTATION Primary lymphedema: occurs as a result of abnormal development of the lymphatic system LYMPHEDEMA Secondary lymphedema: results from damage, disruption or trauma to a previously normal lymphatic system Stage 0 sub-clinical lymphedema with impaired lymph drainage and subjective symptoms of heaviness. STAGES OF Stage I reversible pitting edema high in protein content LYMPHEDEMA fatty fibrosis irreversible pitting edema which in later stages Stage iii also called elephantiasis andexhibits characterized by fibrotic skin changes andearly thickening due to fatty deposition with pappilomatosis. STAGES OF LYMPHEDEMA • 0 STAGE: SUBCLINICAL IMPAIRED LYMPH DRAINAGE WITH SUBJECTIVE SYMPTOMS OF HEAVINESS THAT CAN EXIST MONTHS BEFORE OVERT EDEMA • STAGE I: REVERSIBLE ACCUMULATION OF HIGH PROTEIN FLUID WITH PITTING • STAGE II: IRREVERSIBLE EDEMA WITH PITTING AND IN LATER STAGES SOME FIBROUS OCCURS • STAGE III: ALSO CALLED ELEPHANTIASIS, PITTING IS ABSENT DUE TO FIBROTIC SKIN CHANGES AND FATTY DEPOSITION WITH PAPILLOMATOSIS DIAGNOSIS OF LYMPHEDEMA • CLINICAL: SUBJECTIVE SYMPTOMS OF SWELLING, HEAVINESS AND STIFFNESS PAIRED WITH FINDING OF EDEMA AND STEMMER’S SIGN AND AT LEAST A 2 CM DIFFERENCE IN LIMB CIRCUMFERENCE. • PROCEDURAL DIAGNOSTICS: A. LYMPHOSCINTIGRAPHY B. MRI LYMPHOGRAPHY (NOT APPROVED IN US) C. NEAR INFRARED FLUORESCENCE IMAGING (NIRF) WITH INDOCYANINE GREEN (ICG)