Health and Integrated Protection Needs in Ghazni Province
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Construction Sector Sector Overview
Construction Sector Sector Overview OFFICE OF THE SENIOR ECONOMIC ADVISOR FE BR UA RY 2017 This report has been made via interviewing with several organizations Organization Interview Date Discussion Summary MUDH October 06, 2015 Work on establishing Policy for sector is going on. Afghan Builder Association October 07, 2015 Introduction of ABA & List of Companies, and Challenges is asked. Kabul Municipality October 11, 2015 Procedures of housing in KM, NO. of Housing Dwellings Revenue Department of MoF October 13, 2015 Taxes and Revenues of Major Companies and Sector AISA October 13, 2015 List of Housing Companies registered & investments Private Construction Companies October, 2015 Current Project, Prices, Challenges of Company CSO October 27, 2015 No of buildings, Labor, Value of Construction Sector Housing Construction Enterprise November, 2016 Existing Capacity and predicted Capacity Banaee Construction Enterprise November, 2016 Existing Capacity and predicted Capacity Afghani Construction Enterprise November, 2016 Existing Capacity and predicted Capacity Construction Directorates of MoE, MoI and MoD November, 2016 Construction performance, capacity and budget for 2017 Central Bank of Afghanistan (DAB) December , 2016 Housing Finance Industry Data MUDH December, 2016 Housing Schemes, Challenges, shortage and recommendations 2 Table of Contents Sections Executive Summary 1 Housing Construction Overview 2 Demand Supply Regulatory Bodies MUDH Tasadees Overview 3 HCE Banaee Afghani Housing Financial Overview 4 Case Studies Schemes Recommendations 5 Annexes 6 Executive Summary This report on housing construction sector of Afghanistan has four main objectives. This includes (1) providing an overview of housing construction industry of Afghanistan, (2) providing an overview of the major players, (3) examining the possibility of providing low cost housing for militaries personnel and other civil servants, and (4) examining ways to help government to stimulate the private housing market. -
GOVERNMENT of KHYBER PAKHTUNKHWA ELEMENTARY & SECONDARY EDUCATION DEPARTMENT , Dated Peshawar the 17-03-2016
GOVERNMENT OF KHYBER PAKHTUNKHWA ELEMENTARY & SECONDARY EDUCATION DEPARTMENT , Dated Peshawar the 17-03-2016 NOTIFICATION No.SO(PE)/2-6/DPCMeeting/SST-SS (20/10/2015): On the recommendations of the Departmental Promotion Committee, the Competent Authority is pleased to promote the following Seven Hundred and Thirty Seven (737) Male SSTs (BS-16) to the post of Subject Specialist (BS-17) on regular basis with immediate effect:- S# in Name and S# SL# Present school Address Proposed Station Remarks Subject Qualification 1 1 746 Sikandar Khan GHS Pakha Ghulam SS B-17 (Biology) Against vacant post Peshawar GHSS Tehkal Bala Peshawar 2 2 1370 Zeenat Ullah SET GHS Mitha Khel Karak SS B-17 (Biology) Against vacant post MSc BEd GHSS Dabli Lawaghar Karak 3 3 1813 Mr Sultan Farooq, GHS Sarwar Jan Bala Services placed at the Against vacant post SET Khel FR Bannu disposal of Director Education FATA 4 4 1871 Mr Akhtar Nawaz GCMHS Turbela SS B-17 (Biology) Against vacant post Khan MSc:M.Ed Township Haripur GHSS Jatti Pind, Haripur 5 5 2751 Mr, Muhammad GHS Rashakai Nowshera SS B-17 (Biology) Against vacant post Fayaz Shah SET GHSS Rashakai, Nowshera 6 6 2768 Mr, Yousaf Zaman, GHS Jan Killa Bannu SS B-17 (Biology) Against vacant post SET GHSS Nari Panoos, Karak 7 7 2775 Mr, Bakht Baidar, GHSS Barikot Swat SS B-17 (Biology) Against vacant post SER GHSS Kishawra, Swat 8 8 2799 Mr, Janat Gul, SET GHSS Khanpur Dir SS B-17 (Biology) Against vacant post Lower GHSS Asbanr Dir Lower 9 9 2894 Mr,Bakht Ali GHSS Serai Naurang SS B-17 (Biology) Against vacant post -

Convention on the Prohibition of the Use, Stockpiling, Production and Transfer of Anti-Personnel Mines and on Their Destruction
CONVENTION ON THE PROHIBITION OF THE USE, STOCKPILING, PRODUCTION AND TRANSFER OF ANTI-PERSONNEL MINES AND ON THEIR DESTRUCTION Reporting Formats for Article 7 STATE [PARTY]: Afghanistan Mohammad Shafiq Yosufi, Director Directorate of Mine Action Coordination POINT OF CONTACT: (DMAC1), Afghanistan National Disaster Management Authority (ANDMA). Email: [email protected] Tel: +93 (0) 705 966 401 (Name, organization, telephone, fax, email) (ONLY FOR THE PURPOSES OF CLARIFICATION) 1 The government department working for mine action previously known as Department of Mine Clearance (DMC) was officially changed to DMAC in 2015. COVER PAGE OF THE ANNUAL ARTICLE 7 REPORT NAME OF STATE [PARTY]: Afghanistan REPORTING PERIOD: 1St January 2018 to 31st December 2018 (dd/mm/yyyy) (dd/mm/yyyy) Form A: National implementation measures: Form E: Status of conversion programs: Form I: Warning measures: ✓ changed changed ✓ changed unchanged (last reporting: yyyy) ✓ unchanged (last reporting: yyyy) un changed (last reporting: yyyy) non-applicable non-applicable Form B: Stockpiled anti-personnel mines: Form F: Program of APM destruction: Form J: Other Relevant Matters ✓ changed ✓ changed ✓ changed unchanged (last reporting: yyyy) unchanged (last reporting: yyyy) un changed (last reporting: yyyy) non-applicable non-applicable non -applicable Form C: Location of mined areas: Form G: APM destroyed: ✓ changed ✓ changed unchanged (last reporting: yyyy) unchanged (last reporting: yyyy) non-applicable non-applicable Form D: APMs retained or transferred: Form -
Afghanistan State Structure and Security Forces
European Asylum Support Office Afghanistan State Structure and Security Forces Country of Origin Information Report August 2020 SUPPORT IS OUR MISSION European Asylum Support Office Afghanistan State Structure and Security Forces Country of Origin Information Report August 2020 More information on the European Union is available on the Internet (http://europa.eu). ISBN: 978-92-9485-650-0 doi: 10.2847/115002 BZ-02-20-565-EN-N © European Asylum Support Office (EASO) 2020 Reproduction is authorised, provided the source is acknowledged, unless otherwise stated. For third-party materials reproduced in this publication, reference is made to the copyrights statements of the respective third parties. Cover photo: © Al Jazeera English, Helmand, Afghanistan 3 November 2012, url CC BY-SA 2.0 Taliban On the Doorstep: Afghan soldiers from 215 Corps take aim at Taliban insurgents. 4 — AFGHANISTAN: STATE STRUCTURE AND SECURITY FORCES - EASO COUNTRY OF ORIGIN INFORMATION REPORT Acknowledgements This report was drafted by the European Asylum Support Office COI Sector. The following national asylum and migration department contributed by reviewing this report: The Netherlands, Office for Country Information and Language Analysis, Ministry of Justice It must be noted that the review carried out by the mentioned departments, experts or organisations contributes to the overall quality of the report, it but does not necessarily imply their formal endorsement of the final report, which is the full responsibility of EASO. AFGHANISTAN: STATE STRUCTURE AND SECURITY -

Public Sector Development Programme 2019-20 (Original)
GOVERNMENT OF BALOCHISTAN PLANNING & DEVELOPMENT DEPARTMENT PUBLIC SECTOR DEVELOPMENT PROGRAMME 2019-20 (ORIGINAL) Table of Contents S.No. Sector Page No. 1. Agriculture……………………………………………………………………… 2 2. Livestock………………………………………………………………………… 8 3. Forestry………………………………………………………………………….. 11 4. Fisheries…………………………………………………………………………. 13 5. Food……………………………………………………………………………….. 15 6. Population welfare………………………………………………………….. 16 7. Industries………………………………………………………………………... 18 8. Minerals………………………………………………………………………….. 21 9. Manpower………………………………………………………………………. 23 10. Sports……………………………………………………………………………… 25 11. Culture……………………………………………………………………………. 30 12. Tourism…………………………………………………………………………... 33 13. PP&H………………………………………………………………………………. 36 14. Communication………………………………………………………………. 46 15. Water……………………………………………………………………………… 86 16. Information Technology…………………………………………………... 105 17. Education. ………………………………………………………………………. 107 18. Health……………………………………………………………………………... 133 19. Public Health Engineering……………………………………………….. 144 20. Social Welfare…………………………………………………………………. 183 21. Environment…………………………………………………………………… 188 22. Local Government ………………………………………………………….. 189 23. Women Development……………………………………………………… 198 24. Urban Planning and Development……………………………………. 200 25. Power…………………………………………………………………………….. 206 26. Other Schemes………………………………………………………………… 212 27. List of Schemes to be reassessed for Socio-Economic Viability 2-32 PREFACE Agro-pastoral economy of Balochistan, periodically affected by spells of droughts, has shrunk livelihood opportunities. -

AFGHANISTAN - Base Map KYRGYZSTAN
AFGHANISTAN - Base map KYRGYZSTAN CHINA ± UZBEKISTAN Darwaz !( !( Darwaz-e-balla Shaki !( Kof Ab !( Khwahan TAJIKISTAN !( Yangi Shighnan Khamyab Yawan!( !( !( Shor Khwaja Qala !( TURKMENISTAN Qarqin !( Chah Ab !( Kohestan !( Tepa Bahwddin!( !( !( Emam !( Shahr-e-buzorg Hayratan Darqad Yaftal-e-sufla!( !( !( !( Saheb Mingajik Mardyan Dawlat !( Dasht-e-archi!( Faiz Abad Andkhoy Kaldar !( !( Argo !( Qaram (1) (1) Abad Qala-e-zal Khwaja Ghar !( Rostaq !( Khash Aryan!( (1) (2)!( !( !( Fayz !( (1) !( !( !( Wakhan !( Khan-e-char Char !( Baharak (1) !( LEGEND Qol!( !( !( Jorm !( Bagh Khanaqa !( Abad Bulak Char Baharak Kishim!( !( Teer Qorghan !( Aqcha!( !( Taloqan !( Khwaja Balkh!( !( Mazar-e-sharif Darah !( BADAKHSHAN Garan Eshkashem )"" !( Kunduz!( !( Capital Do Koh Deh !(Dadi !( !( Baba Yadgar Khulm !( !( Kalafgan !( Shiberghan KUNDUZ Ali Khan Bangi Chal!( Zebak Marmol !( !( Farkhar Yamgan !( Admin 1 capital BALKH Hazrat-e-!( Abad (2) !( Abad (2) !( !( Shirin !( !( Dowlatabad !( Sholgareh!( Char Sultan !( !( TAKHAR Mir Kan Admin 2 capital Tagab !( Sar-e-pul Kent Samangan (aybak) Burka Khwaja!( Dahi Warsaj Tawakuli Keshendeh (1) Baghlan-e-jadid !( !( !( Koran Wa International boundary Sabzposh !( Sozma !( Yahya Mussa !( Sayad !( !( Nahrin !( Monjan !( !( Awlad Darah Khuram Wa Sarbagh !( !( Jammu Kashmir Almar Maymana Qala Zari !( Pul-e- Khumri !( Murad Shahr !( !( (darz !( Sang(san)charak!( !( !( Suf-e- (2) !( Dahana-e-ghory Khowst Wa Fereng !( !( Ab) Gosfandi Way Payin Deh Line of control Ghormach Bil Kohestanat BAGHLAN Bala !( Qaysar !( Balaq -

The Kingdom of Afghanistan: a Historical Sketch George Passman Tate
University of Nebraska Omaha DigitalCommons@UNO Books in English Digitized Books 1-1-1911 The kingdom of Afghanistan: a historical sketch George Passman Tate Follow this and additional works at: http://digitalcommons.unomaha.edu/afghanuno Part of the History Commons, and the International and Area Studies Commons Recommended Citation Tate, George Passman The kingdom of Afghanistan: a historical sketch, with an introductory note by Sir Henry Mortimer Durand. Bombay: "Times of India" Offices, 1911. 224 p., maps This Monograph is brought to you for free and open access by the Digitized Books at DigitalCommons@UNO. It has been accepted for inclusion in Books in English by an authorized administrator of DigitalCommons@UNO. For more information, please contact [email protected]. Tate, G,P. The kfn&ean sf Af&mistan, DATE DUE I Mil 7 (7'8 DEDICATED, BY PERMISSION, HIS EXCELLENCY BARON HARDINGE OF PENSHURST. VICEROY AND GOVERNOR-GENERAL OF INDIA, .a- . (/. BY m HIS OBEDIENT, SERVANT THE AUTHOR. il.IEmtev 01 the Asiniic Society, Be?zg-nl, S?~rueyof I~din. dafhor of 'I Seisinqz : A Menzoir on the FJisio~y,Topo~rcrphj~, A7zliquiiies, (112d Peo$Ie of the Cozi?zt~y''; The F/.o?zlic7,.~ of Baluchisia'nn : Travels on ihe Border.? of Pe~szk n?zd Akhnnistnn " ; " ICalnf : A lMe??zoir on t7ze Cozl7~try and Fnrrzily of the Ahntadsai Khn7zs of Iinlnt" ; 4 ec. \ViTkI AN INrPR<dl>kJCTOl2Y NO'FE PRINTED BY BENNETT COLEMAN & Co., Xc. PUBLISHED AT THE " TIMES OF INDIA" OFFTCES, BOMBAY & C.1LCUTT-4, LONDON AGENCY : gg, SI-IOE LANE, E.C. -
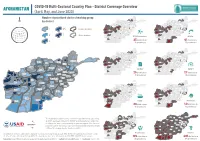
AFGHANISTAN COVID-19 Multi-Sectoral Country Plan - District Coverage Overview (April, May, and June 2020) Number of Prioritized Clusters/Working Group
AFGHANISTAN COVID-19 Multi-Sectoral Country Plan - District Coverage Overview (April, May, and June 2020) Number of prioritized clusters/working group Badakhshan Badakhshan Jawzjan Kunduz Jawzjan Kunduz Balkh Balkh N by district Takhar Takhar Faryab Faryab Samangan Samangan Sar-e-Pul Baghlan Sar-e-Pul Baghlan Panjsher Nuristan Panjsher Nuristan Badghis Parwan Badghis Parwan Bamyan Kapisa Kunar Bamyan Kapisa Kunar Laghman Laghman Kabul Kabul Maidan Wardak Maidan Wardak Ghor Nangarhar Ghor Nangarhar 1 4-5 province boundary Logar Logar Hirat Daykundi Hirat Daykundi Paktya Paktya Ghazni Khost Ghazni Khost Uruzgan Uruzgan Farah Farah Paktika Paktika 2 7 district boundary Zabul Zabul DTM Prioritized: WASH: Hilmand Hilmand Kandahar Kandahar Nimroz Nimroz 25 districts in 41 districts in 3 10 provinces 13 provinces Badakhshan Badakhshan Jawzjan Kunduz Jawzjan Kunduz Balkh Balkh Takhar Takhar Faryab Faryab Samangan Samangan Sar-e-Pul Baghlan Sar-e-Pul Baghlan Panjsher Nuristan Panjsher Nuristan Badghis Parwan Badghis Parwan Bamyan Kapisa Kunar Bamyan Kapisa Kunar Laghman Laghman Kabul Kabul Maidan Wardak Maidan Wardak Badakhshan Ghor Nangarhar Ghor Nangarhar Jawzjan Logar Logar Kunduz Hirat Daykundi Hirat Daykundi Balkh Paktya Paktya Takhar Ghazni Khost Ghazni Khost Uruzgan Uruzgan Farah Farah Paktika Paktika Faryab Zabul Zabul Samangan Baghlan Hilmand EiEWG: Hilmand ESNFI: Sar-e-Pul Kandahar Kandahar Nimroz Nimroz Panjsher Nuristan 25 districts in 27 districts in Badghis Parwan Bamyan Kapisa Kunar 10 provinces 12 provinces Laghman Kabul Maidan -

Education in Danger
Education in Danger Monthly News Brief September Attacks on education 2019 The section aligns with the definition of attacks on education used by the Global Coalition to Protect Education under Attack (GCPEA) in Education under Attack 2018. Africa This monthly digest comprises Kenya threats and incidents of Around 12 September 2019: In Mathemba, Wote town, Makueni violence as well as protests county, several students were reportedly beaten and injured by police and other events affecting officer who stormed the Mathemba Secondary School during a planned education. strike. Sources: Standard Media and Batatv It is prepared by Insecurity Somalia Insight from information 26 September 2019: In Mogadishu, an IED reportedly planted by al available in open sources. Shabaab detonated, striking a bulletproof vehicle carrying Turkish engineers of the education body Maarif Foundation near the KM-5 intersection. Source: AA Access data from the Education in Danger Monthly News Brief South Africa on HDX Insecurity Insight. 02 September 2019: In Port Elizabeth, Eastern Cape province, violent clashes ensued between student protestors and security officials at Nelson Mandela University. The students were demonstrating against Visit our website to download previous Education in Danger the lack of action taken by the university in response to concerns about Monthly News Briefs. safety on campus. Following the violence, seven students were reportedly arrested. Sources: News 24, Herald Live I and Herald Live II Join our mailing list to receive monthly reports on insecurity South Sudan affecting provision of education. 05 September 2019: In Yei River state, government and opposition forces continued to occupy schools, despite orders from their senior commanders to vacate the buildings. -

Contamination Status of Districts in Afghanistan
C O N T A M I N A T I O N S T A T U S O F D I S T R I C T S I N A F G H A N I S T A N ? ? ? ? ? ? ? As of 31st March 2019 ? ? ? ? ? T A J I K I S T A N ? ? ? ? ? ? ? U Z B E K I S T A N ? Shaki Darwazbala Darwaz ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? K? uf Ab N Khwahan A Raghistan Shighnan ? T Darqad Yawan ? Yangi Shahri Qala Kohistan ? S ? Buzurg ? Khwaja Chah Ab Bahawuddin Kham Shortepa Yaftal Sufla Wakhan I Qarqin ? Dashti ? ? Arghanj ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? Ab ? ? ? Qala ? ? ? ? ? Khani ? ? Fayzabad Khaw ? Imam Sahib ? ? ? N Mangajek Kaldar ? ? Chahar !. ? ? ? ? ? Shahada ? ? ? ? ? ? Khwaja Du Koh ? ? Dawlatabad Argo Faizabad ? Mardyan Dashte ? ? ? Bagh ? ? ? ? ? ? ? C H I N A Qurghan ? Takhar E ? Khwaja ? ? Baharak ? Rustaq ? Archi ? ? ? Hazar ? ? Badakhs han Nahri ? Aqcha Ghar ? Andkhoy ? Kunduz ? ? Sumu? ch Khash ? ? Shahi ? ? ? ? ? Balkh ? Baharak M ? Jawzjan Qalay-I- Zal ? ? Darayim Chahar Khulm Is hkashiem ? ? ? ? Kunduz ? Kalfagan Qaramqol Khaniqa ? ? ? ? ? ? Bolak ? Kishim ? Warduj ? Jurm ? ? ? !. ? Mazar-e Sharif ? !. ? ? ? ? ? ? K ? ? ? ? ? ? Taloqa? n ? ? Taluqan She be rg han ? !. ? ? ? ? ? ? Tashkan ? ? ? ? !. ? ? ? ? ? ? Dihdadi ? ? ? Marmul ? ? ? Chahar Dara ? ? ? Fayzabad ? ? Kunduz ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? R ? Bangi Khanabad ? ? Tagab Namak ? Aliabad ? Chimtal ? Dawlatabad ? ? (Kishmi Feroz ? Hazrati ? ? Chal Shibirghan ? ? Ab ? Farkhar Yamgan ? ? ? ? ? U Sari Pul Balkh Nakhchir Su? ltan Bala) Zebak ? ? Chahar ? (Girwan) ? Baghlani ? Ishkamish ? ? ? ? ? ? Kint ? ? ? ? ? ? Sholgara ? ? ? ? ? -

Balkh's Chamtal District Cleaned up from Rebels
www.outlookafghanistan.net www.thedailyafghanistan.com facebook.com/The.Daily.Outlook.Afghanistan facebook.com/The.Daily.Afghanistan Email: [email protected] Email: [email protected] Phone: 0093 (799) 005019/777-005019 Phone: 0093 (799) 005019/777-005019 Add: Sarai Ghazni, District 3, Kabul Add: Sarai Ghazni, District 3, Kabul Back Page August 22, 2017 Jalalabad Clear Ghazni Kandahar Clear Clear Mazar Clear Herat Clear Bamayan Clear Kabul Clear Daily Outlook 36°C 32°C 38°C 37°C 33°C 26°C 31°C Weather 28°C 16°C 24°C 25°C 16°C 12°C 18°C Forcast Balkh’s Chamtal District Cleaned up from Rebels MAZAR-I-SHARIF - Local officials on Monday said Chamtal district of Security Forces northern Balkh province has been cleaned of militants during an Af- Recapture Some Areas ghan forces operation. An operation launched by the Shahin of Mirzawlang Military Corps against militants was SAR-I-PUL CITY - Security forces have underway since Saturday night and taken control of Sheram and Kalta Taw ar- was ended late on Sunday. eas of Mirzawlang village in northern Sar- Amanullah Mobin, the commander i-Pul province, an official said on Monday. for the corps, told reporters that Governor Mohammad Zahir Wahdat told around 50 militants suffered casual- Pajhwok Afghan News the security forces ties and eight others were arrested carried out a predawn operation for retak- during the operation. Six security ing the valley. The security personnel suf- personnel were also killed. fered no casualties. He said that there were no rebels cur- Mirzawlang was overrun by militants on rently in Chamtal district after the August 4 when 50 civilians were reported- operation. -

Individuals and Organisations
Designated individuals and organisations Listed below are all individuals and organisations currently designated in New Zealand as terrorist entities under the provisions of the Terrorism Suppression Act 2002. It includes those listed with the United Nations (UN), pursuant to relevant Security Council Resolutions, at the time of the enactment of the Terrorism Suppression Act 2002 and which were automatically designated as terrorist entities within New Zealand by virtue of the Acts transitional provisions, and those subsequently added by virtue of Section 22 of the Act. The list currently comprises 7 parts: 1. A list of individuals belonging to or associated with the Taliban By family name: • A • B,C,D,E • F, G, H, I, J • K, L • M • N, O, P, Q • R, S • T, U, V • W, X, Y, Z 2. A list of organisations belonging to or associated with the Taliban 3. A list of individuals belonging to or associated with ISIL (Daesh) and Al-Qaida By family name: • A • B • C, D, E • F, G, H • I, J, K, L • M, N, O, P • Q, R, S, T • U, V, W, X, Y, Z 4. A list of organisations belonging to or associated with ISIL (Daesh) and Al-Qaida 5. A list of entities where the designations have been deleted or consolidated • Individuals • Entities 6. A list of entities where the designation is pursuant to UNSCR 1373 1 7. A list of entities where the designation was pursuant to UNSCR 1373 but has since expired or been revoked Several identifiers are used throughout to categorise the information provided.