Objectives Body Fluid Compartments
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

BIPN100 F15 Human Physiology 1 (Kristan) Lecture 15. Body Fluids, Tonicity P
BIPN100 F15 Human Physiology 1 (Kristan) Lecture 15. Body fluids, tonicity p. 1 Terms you should understand: intracellular compartment, plasma compartment, interstitial compartment, extracellular compartment, dilution technique, concentration, quantity, volume, Evans blue, plasma volume, interstitial fluid, inulin, total body water, intracellular volume, diffusion, osmosis, colligative property, osmotic pressure, iso-osmotic, hypo-osmotic, hyperosmotic, tonicity, isotonic, hypotonic, hypertonic, active transport, symporter, antiporter, facilitated diffusion. I. Body fluids are distributed in a variety of compartments. A. The three major compartments are: 1. Intracellular compartment = total volume inside all body cells. 2. Plasma compartment = fluid volume inside the circulatory system. 3. Interstitial compartment = volume between the plasma and intracellular compartments. 4. Extracellular compartment = plasma + interstitial fluid B. Slowly-exchanging compartments include bones and dense connective tissues, fluids within the eyes and in the joint capsules; in total, they comprise a small volume. C. Cells exchange materials with the environment almost entirely through the plasma. Fig. 15.1. The major fluid compartments of the body and how water, ions, and metabolites pass among them. D. Under normal conditions, the three compartments are in osmotic equilibrium with one another, but they contain different distributions of solutes. 1. There is a lot of organic anion (mostly proteins) inside cells, essentially none in interstitial fluid, and small quantities in the plasma. 2. Na+ and K+ have inverse concentration profiles across the cell membranes. 3. The total millimolar concentration of solutes is equal in each of the three compartments. 4. Materials that exchange between compartments must cross barriers: a. Cell membranes separate the intracellular and interstitial compartments. b. -

Body Fluid Compartments Dr Sunita Mittal
Body fluid compartments Dr Sunita Mittal Learning Objectives To learn: ▪ Composition of body fluid compartments. ▪ Differences of various body fluid compartments. ▪Molarity, Equivalence,Osmolarity-Osmolality, Osmotic pressure and Tonicity of substances ▪ Effect of dehydration and overhydration on body fluids Why is this knowledge important? ▪To understand various changes in body fluid compartments, we should understand normal configuration of body fluids. Total Body Water (TBW) Water is 60% by body weight (42 L in an adult of 70 kg - a major part of body). Water content varies in different body organs & tissues, Distribution of TBW in various fluid compartments Total Body Water (TBW) Volume (60% bw) ________________________________________________________________ Intracellular Fluid Compartment Extracellular Fluid Compartment (40%) (20%) _______________________________________ Extra Vascular Comp Intra Vascular Comp (15%) (Plasma ) (05%) Electrolytes distribution in body fluid compartments Intracellular fluid comp.mEq/L Extracellular fluid comp.mEq/L Major Anions Major Cation Major Anions + HPO4- - Major Cation K Cl- Proteins - Na+ HCO3- A set ‘Terminology’ is required to understand change of volume &/or ionic conc of various body fluid compartments. Molarity Definition Example Equivalence Osmolarity Osmolarity is total no. of osmotically active solute particles (the particles which attract water to it) per 1 L of solvent - Osm/L. Example- Osmolarity and Osmolality? Osmolarity is total no. of osmotically active solute particles per 1 L of solvent - Osm/L Osmolality is total no. of osmotically active solute particles per 1 Kg of solvent - Osm/Kg Osmosis Tendency of water to move passively, across a semi-permeable membrane, separating two fluids of different osmolarity is referred to as ‘Osmosis’. Osmotic Pressure Osmotic pressure is the pressure, applied to stop the flow of solvent molecules from low osmolarity to a compartment of high osmolarity, separated through a semi-permeable membrane. -

Kidney: Body Fluids & Renal Function
Kidney: Body Fluids & Renal Function Adapted From: Textbook Of Medical Physiology, 11th Ed. Arthur C. Guyton, John E. Hall Chapters 25, 26, & 27 John P. Fisher © Copyright 2012, John P. Fisher, All Rights Reserved Overview of The Kidney and Body Fluids Introduction • The maintenance of volume and a stable composition of body fluids is essential for homeostasis • The kidneys are key players that control many functions • Overall regulation of body fluid volume • Regulation of the constituents of extracellular fluid • Regulation of acid-base balance • Control of fluid exchange between extracellular and intracellular compartments © Copyright 2012, John P. Fisher, All Rights Reserved 1 Balance of Fluid Intake and Fluid Output Introduction • Water intake comes from two sources • Ingested in the form of liquids or within food Normal Exercise • Synthesized as a result of the Intake oxidation of carbohydrates Ingested 2100 ? Metabolism 200 200 • Water loss occurs in many forms Total Intake 2300 ? • Insensible water loss • Evaporation through skin Output • Humidification of inspired air Insensible - Skin 350 350 • Sweat Insensible - Lungs 350 650 • Feces Sweat 100 5000 • Urine Feces 100 100 • The kidneys are a critical Urine 1400 500 mechanism of controlling water Total Output 2300 6600 loss © Copyright 2012, John P. Fisher, All Rights Reserved Balance of Fluid Intake and Fluid Output Body Fluid Compartments • Total body fluid is divided between extracellular fluid, transcellular fluid, and intracellular fluid • Extracellular fluid is again divided between blood plasma and interstitial fluid • Transcellular fluid includes fluid in the synovial, peritoneal, pericardial, and intraocular space • A 70 kg person contains approximately 42 liters of water (60%) and varies with significant physical parameters • Age • Sex • Obesity Guyton & Hall. -

Renal Physiology Question
Med Phys 2011 4/18/2011 Lisa M Harrison-Bernard, PhD Associate Professor Department of Physiology Renal Physiologist MEB Room 7213; 568-6175 [email protected] Please Use the Subject Line – Renal Physiology Question Posted on Medical Physiology Schedule of Classes: Learning Objectives, Reading AiAssignmen tHdtPblStts, Handouts, Problems Sets, Tutorials, Review Article Renal Lecture 1 – Harrison-Bernard 1 Med Phys 2011 4/18/2011 Renal Physiology - Lectures 1. Physiology of Body Fluids – Problem Set Posted – 4/19/11 2. Structure & Function of the Kidneys 3. Renal Clearance & Glomerular Filtration – Problem Set Posted 4. Regulation of Renal Blood Flow – Review Article Posted 5. Transport of Sodium & Chloride – Posting of Tutorials A & B Renal Physiology - Lectures 6. Transport of Urea, Glucose, Phosphate, Calcium & Organic Solutes 7. Regulation of Potassium Balance 8. Regulation of Water Balance 9. Transport of Acids & Bases 10. Integration of Salt & Water Balance Renal Lecture 1 – Harrison-Bernard 2 Med Phys 2011 4/18/2011 Renal Physiology - Lectures 11. Clinical Correlation - 5/4/11 12. Problem Set Rev iew – 5/9/11 13. Exam Review – 5/9/11 14. Exam IV – 5/12/11 15. Final Exam – 5/18/11 THE END OF PHYSIOLOGY!! Renal Physiology Lecture 1 Physiology of Body Fluids Chapter 1 - Koeppen & Stanton Renal Physiology 1. Terminology 2. Body Fluid Compartments 3. IditDiltiPiilIndicator Dilution Principle 4. Clinical Examples Renal Lecture 1 – Harrison-Bernard 3 Med Phys 2011 4/18/2011 Three Emergency Room Patients • 80 yo - over medicated - no drinking -

Third-Spacing: When Body Fluid Shifts by Susan Simmons Holcomb, ARNP-BC, Phd
Topics in Progressive Care Third-spacing: When body fluid shifts By Susan Simmons Holcomb, ARNP-BC, PhD In a healthy adult, nearly all fluid is contained in Water, water the intracellular, intravascular, or interstitial everywhere spaces, with the intracellular space holding about two-thirds of total body water. Normally, fluid moves freely between these three spaces to main- Intracellular fluid tain fluid balance (see Water, water everywhere). Third-spacing occurs when too much fluid moves Ifrom the intravascular space (blood vessels) into the interstitial or “third” space—the nonfunctional Intravascular fluid area between cells. This can cause potentially seri- ous problems such as edema, reduced cardiac output, and hypotension. Interstitial fluid In this article, I’ll describe why third-spacing occurs and how to intervene to restore balance. Let’s start with a brief physiology review. Body fluids are distributed between the intracellular What’s behind third-spacing? and extracellular fluid compartments. The intracellular Fluid volume, pressure, and levels of sodium compartment consists of fluid contained within all the and albumin are the keys to maintaining fluid body cells. The extracellular compartment contains all balance between the intracellular and extracellu- the fluids outside the cells, including fluid in the inter- lar (intravascular and interstitial) spaces. Capillary stitial (tissue) spaces, and that in the intravascular permeability and the lymphatic system also play space (blood vessels). a role. A problem with any of these components can cause fluid to shift from the intravascular space losses during diarrhea or fluid losses caused by to the interstitial space. Let’s look more closely at medications such as diuretics. -

Fluid & Electrolyte Balance
Fluid & Electrolyte Balance body is ~2/3rds water (males=63%; women=52%) this water occupies three “compartments”: intracellular 63% (or 40% of body wt) 25L facilitates chemical reactions, solvent extracellular 37% (or 20% of body wt) [15L] provides internal environment for cells and transport, protection, etc transcellular (CSF, eye, synovial joints, bursae) 30% 12L interstitial lymph plasma (=intravascular) 7% 3L Total: 40L* *based on 70kg(154lb) person Total amount of water & solutes in each compartment remain relatively constant water content and movement is tied to electrolytes and solute concentrations and movement eg. if solutes leave a compartment by diffusion; water also leaves by osmosis water follows salt can’t talk about fluid balance without talking about electrolyte balance balance means: input = output Inputs 1. digestive tract: food and drink 2. metabolism: each cell produces water in catabolism of glucose Outputs 1. urine (kidneys) 2. lungs: water vapor expired with air 3. sweat (skin) 4. feces (intestines) output is crucial element in control of fluids and electrolytes Human Anatomy & Physiology: Fluid & Electrolyte Balance; Ziser, 2004 1 most important output organ is kidney urine volume is controlled by: glomerular filtration rate reabsorption by tubules glomerular filtration rate remains fairly constant not a strong controlling influence on urine volume major control of urine volume is reabsorption of water reabsorption can be controlled to make output match input controlled by two major hormones: ADH decrease in ECF volume stimulates release of ADH ?osmoreceptors in hypothalamus? makes distal & collecting tubes permeable to water increases water reabsorption decreases urine volume Aldosterone increases tubular reabsorption of sodium and other ions increases water reabsorption by osmosis decreases urine volume additional factors that can affect fluid loss 1. -

Renal General Functions - László Rosivall, Shahrokh Mirzahosseini
PHYSIOLOGY AND MAINTENANCE – Vol. III - Renal General Functions - László Rosivall, Shahrokh MirzaHosseini RENAL GENERAL FUNCTIONS László Rosivall Department of Pathophysiology, Faculty of Medicine, Semmelweis University, Hungary, and Hungarian Academy of Sciences and Semmelweis University Nephrology Research Group. Shahrokh MirzaHosseini Avicenna International College, Budapest, Hungary. Keywords: ADH, aldosterone, ANH, creatinine, edema, erythropoietin, glucosuria, hypertension, polyuria, proteinuria, renin, urea, uremia, vitamin D3. Contents 1. Introduction 2. Renal General Functions 3. Body Fluid Compartments 4. Juxtaglomerular Apparatus (JGA) Releases Renin 5. Glomerular Ultrafiltration (GFR) and Its Determination 6. Composition of the Glomerular Filtrate 7. Tubular Filtrate Processing 7.1. Reabsorption 7.2. Tubular Excretion Glossary Bibliography Biographical Sketches Summary The human organism is constantly in exchange with its environment as an open system. The organism receives and disposes e.g. fluid and electrolytes from/to its environment. The organism is very sensitive to the deprivation of fluid and electrolyte as compared to its tolerance to calorie (food) deprivation. The role of kidneys is to tightly regulate the balanced optimum conditions required by the cells for their normal activities. This balanced, optimum internal environment condition is referred to as “homeostasis”. Kidneys UNESCOexcrete the waste products of –me tabolism,EOLSS produce, secrete and metabolize hormones, and regulate the pH and electrolytes balance. The kidneys are also involved in the oxygen SAMPLEcarrying capacity of the blood CHAPTERS by producing erythropoietin hormone which contributes to the regulation of the erythrocyte number in the circulation. Several systems integrate the renal functions with the activity of the endocrine system. Nutritional status can affect the renal tasks in many ways. -

The Body Fluid Compartments: Extracellular and Intracellular Fluids; Edema
C H A P T E R 2 5 U N I T V The Body Fluid Compartments: Extracellular and Intracellular Fluids; Edema The maintenance of a relatively constant volume and a conditions. This loss is termed insensible water loss stable composition of the body fluids is essential for because we are not consciously aware of it, even though homeostasis. Some of the most common and important it occurs continually in all living humans. problems in clinical medicine arise because of abnor Insensible water loss through the skin occurs indepen malities in the control systems that maintain this relative dently of sweating and is present even in people who are constancy of the body fluids. In this chapter and in born without sweat glands; the average water loss by dif the following chapters on the kidneys, we discuss the fusion through the skin is about 300 to 400 ml/day. This overall regulation of body fluid volume, constituents of loss is minimized by the cholesterolfilled cornified layer the extracellular fluid, acidbase balance, and control of of the skin, which provides a barrier against excessive loss fluid exchange between extracellular and intracellular by diffusion. When the cornified layer becomes denuded, compartments. as occurs with extensive burns, the rate of evaporation can increase as much as 10fold, to 3 to 5 L/day. For this FLUID INTAKE AND OUTPUT reason, persons with burns must be given large amounts ARE BALANCED DURING of fluid, usually intravenously, to balance fluid loss. STEADY-STATE CONDITIONS Insensible water loss through the respiratory tract averages about 300 to 400 ml/day. -
Renal Physiology.Kp
Harvard-MIT Division of Health Sciences and Technology HST.542J: Quantitative Physiology: Organ Transport Systems Instructor: Roger Mark ©Prof. Roger G. Mark, 2004 MASSACHUSETTS INSTITUTE OF TECHNOLOGY Departments of Electrical Engineering, Mechanical Engineering, and the Harvard-MIT Division of Health Sciences and Technology 6.022J/2.792J/HST542J: Quantitative Physiology: Organ Transport Systems RENAL PHYSIOLOGY Text Reference: Chapters 6 and 7 RENAL PHYSIOLOGY These notes will present supplementary material, but are not meant to replace standard texts. Students are encouraged to read chapters 6 and 7 in the textbook by Costanzo. I. INTRODUCTION The kidneys are critical in regulating the internal environment of the body. In particular, they regulate the total body water, as well as a number of substances which are essential to life. We will focus on the following major topics: - Body Fluid Compartments - The Functional Anatomy of the Kidney - Basic Renal Mechanisms Glomerular Filtration Tubular Absorption Tubular Secretion Overall Mass Balance for the Kidneys - Renal Regulation of: Sodium Extracellular Volume and Osmolarity pH Renal Physiology 3 II. Body Fluid Compartments Total body water (TBW) is approximately 60% of body weight. It is distributed as intracellular water (ICW) and extracellular water (ECW). Intracellular water is the largest compartment, comprising approximately 40% of body weight. Extracellular water is about 20% of body weight. (Note the 20, 40, 60 rule for ECW, ICW, and TBW respectively.) Figure 1 shows the approximate sizes of the body fluid compartments. Note that ECW is divided into interstitial fluid (16% of body weight), and blood plasma (4% of body weight). Composition of the body fluid compartments differs markedly as shown in Figure 2. -
Body Fluids Bruce M
Faculty version with model answers Body Fluids Bruce M. Koeppen, M.D., Ph.D. University of Connecticut Health Center Introduction By weight, water comprises approximately 60% of the adult human body (this percentage varies with the amount of adipose tissue (as the amount of adipose tissue increases the percentage of body weight attributed to water decreases). This total body water (TBW) is contained within two major compartments; the intracellular fluid (ICF – 40% of body weight) and the extracellular fluid (ECF – 20% of body weight). Fluid within the ECF is further subdivided into plasma and the fluid surrounding cells (interstitial fluid). Water readily moves between these various fluid compartments. Water movement between the ICF and ECF is driven by differences in osmotic pressure, whereas movement between the vascular compartment (i.e., plasma) and the interstitial fluid compartment is driven by Starling forces across the wall of the capillaries. In this conference we will examine the volumes and composition of the various body fluid compartments, and how fluid shifts occur under a number of conditions. Recommended Reading: Pg. 1 - 15: Renal Physiology, 3rd ed., Koeppen & Stanton, C.V. Mosby, 2001. ___________________________ Capillary Fluid Movement Fluid movement across the wall of a capillary is driven by the sum of the Starling forces; two of which favor (Pc and Πis) and two of which oppose (Pis and Πc) fluid movement out of the capillaries. • Pc: hydrostatic pressure in the capillary • Pis: hydrostatic pressure in the interstitium -

Fluid and Electrolytes Body Fluids Body Fluids Fluid Compartments
5/2/2016 Body Fluids • Body water and dissolved substances – Cells need a stable environment to function Fluid and Electrolytes Body Fluids Fluid Compartments • Body water content • Total body water ≈ 40 L – Infants • Where is it all?? • 73% or more water – 1. Intracellular fluid (ICF) compartment Adult males • 2/3 (25 L) • ~60% water 2. Extracellular fluid (ECF) compartment – Adult females • 1/3 (15 L) • ~50% water a. Plasma: 3 L – Higher fat content & less skeletal muscle mass b. Interstitial fluid (IF): 12 L – Water content declines with old age c. Other ECF • ~45% • Lymph, CSF, humors of the eye, synovial fluid, serous fluid, gastrointestinal secretions Fluid Compartments Total body water Volume = 40 L 60% body weight Extracellular fluid (ECF) • Intracellular fluid Volume = 15 L 20% body weight – Metabolic reactions – Homeostasis essential to health Intracellular fluid (ICF) Interstitial fluid (IF) Volume = 25 L Volume = 12 L 40% body weight 80% of ECF Figure 26.1 1 5/2/2016 Lungs Gastrointestinal Kidneys Fluid Compartments tract • Extracellular fluid Examples? H O, Functions Blood O2 CO 2 Nutrients 2 H2O, Nitrogenous plasma Ions Ions wastes • Route in and out of cell Osmosis is the primary force for movement O CO H O Nitrogenous Interstitial 2 2 Nutrients 2 Ions • Lubricant wastes fluid • Solvent • Acid-base balance Intracellular fluid in tissue cells Figure 26.3 Composition of Body Fluids Blood plasma Interstitial fluid • Intracellular fluid ECF and ICF composition varies Na + Sodium ECF K+ Potassium • All similar, except higher -
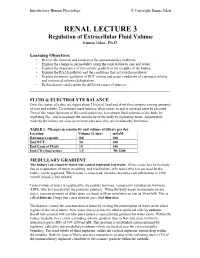
RENAL LECTURE 3 Regulation of Extracellular Fluid Volume Emma Jakoi, Ph.D
Introductory Human Physiology © Copyright Emma Jakoi RENAL LECTURE 3 Regulation of Extracellular Fluid Volume Emma Jakoi, Ph.D. Learning Objectives • Review the function and location of the juxtamedullary nephrons. • Explain the change in permeability along the renal tubule to ions and water. • Explain the importance of the osmotic gradient in the medulla of the kidney. • Explain the RAAS pathway and the conditions that activate this pathway. • Explain hormonal regulation of ECF volume and under conditions of expanded volume and contracted volume (dehydration • Define diuresis and explain the different causes of diuresis. _____________________________________________________________ FLUID & ELECTROLYTE BALANCE Over the course of a day, we ingest about 2 liters of food and drink that contains varying amounts of ions and solutes. To maintain mass balance, what comes in and is not used must be excreted. Two of the major functions of the renal system are to maintain fluid volumes of the body by regulating Na+ and to maintain the osmolarity of the body by regulating water. Adjustments made by the kidney are slow (over hours) because they are mediated by hormones. TABLE 1. Changes in osmolarity and volume of filtrate per day Location Volume (L/day) mOsM Bowman's capsule 180 300 End PCT 54 300 End Loop of Henle 18 100 End CD (final urine) 1.5 50-1200 MEDULLARY GRADIENT The kidney can conserve water but cannot replenish lost water. Of the water lost by the body due to evaporation of sweat, breathing, and metabolism, only water which is excreted by the kidney can be regulated. When water is conserved, the urine becomes concentrated up to 1200 mOsM (blood is 300 mOsM).