Morphometrical Study of the Lumbar Segment of the Internal Vertebral Venous Plexus in Dogs: a Contrast CT-Based Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Development of the Epidural Space in Human Embryos
Folia Morphol. Vol. 63, No. 3, pp. 273–279 Copyright © 2004 Via Medica O R I G I N A L A R T I C L E ISSN 0015–5659 www.fm.viamedica.pl The development of the epidural space in human embryos Magdalena Patelska-Banaszewska, Witold Woźniak Department of Anatomy, University School of Medical Sciences, Poznań, Poland [Received 25 April 2004; Accepted 25 June 2004] The epidural space is seen in embryos at stage 17 (41 days) on the periphery of the primary meninx. During stage 18 (44 days) the dura mater proper appears and the epidural space is located between this meninx and the perichondrium and contains blood vessels. During the last week of the embryonic period (stages 20–23) the epidural space is evident around the circumference of the spinal cord. On the posterior surface it is found between the dura mater and the me- soderm of the dorsal body wall. Key words: human neuroembryology, primary meninx, epidural space INTRODUCTION horizontal, frontal, and sagittal planes and stained The epidural space lies between the spinal dura according to various methods (chiefly Mallory, hae- mater and the periosteum of the vertebral canal. This matoxylin and eosin and with silver salts). In some periosteum is formed by the outer endosteal layer embryos graphic reconstructions were prepared at of the dura mater. The epidural space contains loose each of the stages investigated. connective tissue, venous plexuses and adipose tis- sue, which is particularly evident in the lumbar re- RESULTS gion [8]. There is some evidence that it is only a po- The primordium of the epidural space appears in tential space [2]. -

CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit
228 CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit MUSCLES OF FACIAL EXPRESSION Dural Venous Sinuses Not in the Subendocranial Occipitofrontalis Space More About the Epicranial Aponeurosis and the Cerebral Veins Subcutaneous Layer of the Scalp Emissary Veins Orbicularis Oculi CLINICAL SIGNIFICANCE OF EMISSARY VEINS Zygomaticus Major CAVERNOUS SINUS THROMBOSIS Orbicularis Oris Cranial Arachnoid and Pia Mentalis Vertebral Artery Within the Cranial Cavity Buccinator Internal Carotid Artery Within the Cranial Cavity Platysma Circle of Willis The Absence of Veins Accompanying the PAROTID GLAND Intracranial Parts of the Vertebral and Internal Carotid Arteries FACIAL ARTERY THE INTRACRANIAL PORTION OF THE TRANSVERSE FACIAL ARTERY TRIGEMINAL NERVE ( C.N. V) AND FACIAL VEIN MECKEL’S CAVE (CAVUM TRIGEMINALE) FACIAL NERVE ORBITAL CAVITY AND EYE EYELIDS Bony Orbit Conjunctival Sac Extraocular Fat and Fascia Eyelashes Anulus Tendineus and Compartmentalization of The Fibrous "Skeleton" of an Eyelid -- Composed the Superior Orbital Fissure of a Tarsus and an Orbital Septum Periorbita THE SKULL Muscles of the Oculomotor, Trochlear, and Development of the Neurocranium Abducens Somitomeres Cartilaginous Portion of the Neurocranium--the The Lateral, Superior, Inferior, and Medial Recti Cranial Base of the Eye Membranous Portion of the Neurocranium--Sides Superior Oblique and Top of the Braincase Levator Palpebrae Superioris SUTURAL FUSION, BOTH NORMAL AND OTHERWISE Inferior Oblique Development of the Face Actions and Functions of Extraocular Muscles Growth of Two Special Skull Structures--the Levator Palpebrae Superioris Mastoid Process and the Tympanic Bone Movements of the Eyeball Functions of the Recti and Obliques TEETH Ophthalmic Artery Ophthalmic Veins CRANIAL CAVITY Oculomotor Nerve – C.N. III Posterior Cranial Fossa CLINICAL CONSIDERATIONS Middle Cranial Fossa Trochlear Nerve – C.N. -

Spinal Meninges Neuroscience Fundamentals > Regional Neuroscience > Regional Neuroscience
Spinal Meninges Neuroscience Fundamentals > Regional Neuroscience > Regional Neuroscience SPINAL MENINGES GENERAL ANATOMY Meningeal Layers From outside to inside • Dura mater • Arachnoid mater • Pia mater Meningeal spaces From outside to inside • Epidural (above the dura) - See: epidural hematoma and spinal cord compression from epidural abscess • Subdural (below the dura) - See: subdural hematoma • Subarachnoid (below the arachnoid mater) - See: subarachnoid hemorrhage Spinal canal Key Anatomy • Vertebral body (anteriorly) • Vertebral arch (posteriorly). • Vertebral foramen within the vertebral arch. MENINGEAL LAYERS 1 / 4 • Dura mater forms a thick ring within the spinal canal. • The dural root sheath (aka dural root sleeve) is the dural investment that follows nerve roots into the intervertebral foramen. • The arachnoid mater runs underneath the dura (we lose sight of it under the dural root sheath). • The pia mater directly adheres to the spinal cord and nerve roots, and so it takes the shape of those structures. MENINGEAL SPACES • The epidural space forms external to the dura mater, internal to the vertebral foramen. • The subdural space lies between the dura and arachnoid mater layers. • The subarachnoid space lies between the arachnoid and pia mater layers. CRANIAL VS SPINAL MENINGES  Cranial Meninges • Epidural is a potential space, so it's not a typical disease site unless in the setting of high pressure middle meningeal artery rupture or from traumatic defect. • Subdural is a potential space but bridging veins (those that pass from the subarachnoid space into the dural venous sinuses) can tear, so it is a common site of hematoma. • Subarachnoid space is an actual space and is a site of hemorrhage and infection, for example. -

The Meninges and Common Pathology Understanding the Anatomy Can Lead to Prompt Identification of Serious Pathology
education The meninges and common pathology Understanding the anatomy can lead to prompt identification of serious pathology The meninges are three membranous of the skull and extends into folds that arterial blood has sufficient pressure to layers that surround the structures of the compartmentalise the skull.1 2 The large separate the dura from the bare bone of central nervous system. They include the midline fold separates the two hemispheres the skull.4 The classic example of this is dura mater, the arachnoid mater, and and is called the falx.1 A smaller fold a severe blow to the temple that ruptures the pia mater. Together they cushion the separates the cerebral hemispheres from the middle meningeal artery, which brain and spinal cord with cerebrospinal the cerebellum and is known as the has part of its course between the skull fluid and support the associated vascular tentorium cerebelli usually abbreviated as and the dura at a weak point called the structures.1 2 Although they are usually “tentorium” (fig 1).1‑3 pterion.1 2 4 This creates an extradural mentioned as a trio, there are subtle but Where the edges of the falx and tentorium haematoma,2 a potentially lifethreatening important differences to the arrangement of meet the skull, the dura encloses large injury that classically presents with the meninges in the spine and cranium. The venous sinuses that are responsible for decreased consciousness and vomiting aim of this introduction to the meninges is draining venous blood from the brain.1 4 after a lucid interval (an initial period of to clarify the anatomy and link these details These are not to be confused with the air apparently normal consciousness). -

Anatomical Aspects of Epidural and Spinal Analgesia
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Via Medica Journals Review paper Grzegorz Jagla1, 2, Jerzy Walocha2, K. Rajda3, Jan Dobrogowski4, Jerzy Wordliczek1 1Department of Pain Treatment and Palliative Care Medical College, Jagiellonian University, Krakow, Poland 2Department of Anatomy Medical College, Jagiellonian University, Krakow, Poland 31st Department of Internal Medicine, J. Dietl Hospital, Krakow, Poland 4Department of Pain Research and Treatment, Medical College, Jagiellonian University, Krakow, Poland Anatomical aspects of epidural and spinal analgesia Abstract Regional anaesthesia seems to be the future of the anaesthesia in this century. The knowledge of the anatomy of the epidural and other spinal spaces seems to play the crucial role in success of regional anaesthesia. It's important in perioperative medicine and cancer pain treatment. Up to date there is not too many datas considering anatomy of these compartments. Many of the results obtained by research- ers in the past are still not mentioned in the clinical textbooks. This article is an attempt to resolve this problem. Key words: epidural anesthesia, spinal anesthesia, human anatomy, epidural space Adv. Pall. Med. 2009; 8, 4: 135–146 Introduction nal lamina of the dura mater, and the dural sac which consists of the internal lamina of dura mater Successful a hinges on successfully reaching neu- and arachnoid. Many fragments of this space are ral tissue. The sensation of pain traveling from noci- empty (they contain only air). It can be found in all ceptor to sensory cortex follows an elaborate and places where the dural sac reaches the vertebral complex path before being registered by our brains: pedicles, vertebral lamina or ligamentum flava. -

Anatomy and Physiology of Cerebrospinal Fluid
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/51814628 Anatomy and physiology of cerebrospinal fluid Article in European Annals of Otorhinolaryngology, Head and Neck Diseases · November 2011 DOI: 10.1016/j.anorl.2011.03.002 · Source: PubMed CITATIONS READS 202 10,152 3 authors, including: Laurent Sakka Centre Hospitalier Universitaire de Clermont-Ferrand 67 PUBLICATIONS 478 CITATIONS SEE PROFILE All content following this page was uploaded by Laurent Sakka on 14 November 2018. The user has requested enhancement of the downloaded file. European Annals of Otorhinolaryngology, Head and Neck diseases (2011) 128, 309—316 Available online at www.sciencedirect.com REVIEW OF THE LITERATURE Anatomy and physiology of cerebrospinal fluid L. Sakka a,b,∗, G. Coll b, J. Chazal a,b a Laboratoire d’anatomie, faculté de médecine, université d’Auvergne, 28, place Henri-Dunant, 63001 Clermont-Ferrand cedex 1, France b Image-Guided Clinical Neuroscience and Connectomics, université d’Auvergne, UFR Médecine, CHU de Clermont-Ferrand, Hôpital Gabriel Montpied, 58 rue Montalembert, 63003 Clermont-Ferrand, France Available online 18 November 2011 KEYWORDS Summary The cerebrospinal fluid (CSF) is contained in the brain ventricles and the cranial Cerebrospinal fluid; and spinal subarachnoid spaces. The mean CSF volume is 150 ml, with 25 ml in the ventricles CSF; and 125 ml in subarachnoid spaces. CSF secretion; CSF is predominantly, but not exclusively, secreted by the choroid plexuses. Brain interstitial CSF circulation; fluid, ependyma and capillaries may also play a poorly defined role in CSF secretion. CSF space CSF circulation from sites of secretion to sites of absorption largely depends on the arterial comparative anatomy pulse wave. -

Meninges, Ventricles, and CSF
Meninges, Ventricles, and CSF Lecture (19) ▪ Important ▪ Doctors Notes Please check our Editing File ▪ Notes/Extra explanation ه هذا العمل مب ين بشكل أسا يس عىل عمل دفعة 436 مع المراجعة { َوَم نْ يَ َت َو َ ّكْ عَ َلْ ا َّْلل فَهُ َوْ َحْ سْ ُ ُُْ} والتدقيق وإضافة المﻻحظات وﻻ يغ ين عن المصدر اﻷسا يس للمذاكرة ▪ Objectives At the end of the lecture, students should be able to: ✓ Explain the cerebral meninges & compare between the main dural folds. ✓ Identify the spinal meninges & locate the level of the termination of each of them. ✓ Describe the importance of the subarachnoid space. ✓ Explain the ventricular system of the CNS and locate the site of each of them. ✓ Analyze the formation, circulation, drainage, and functions of the CSF. ✓ Justify the clinical point related to the CSF. Meninges 02:02 The brain and spinal cord (CNS) are invested by three concentric membranes/ layers: 1-The outermost layer is the dura matter.(fibrous) Dura Outside 2-The middle layer is the arachnoid matter.(translucent) Pia Inside 3-The innermost layer is the pia matter.(translucent) 1- (The dura surround 2- (from which it is 3- (Pia mater is a the brain and the separated by thin fibrous tissue that spinal cord and is the subarachnoid space . is impermeable to fluid. responsible for The delicate arachnoid layer This allows the pia keeping in the CSF) is attached to the inside of mater to enclose csf) the dur and surrounds the brain and spinal cord.) Meninges 1- Dura Matter o The cranial dura is a two layered tough, fibrous, thick membrane that surrounds the brain. -

Anatomy and Clinical Importance of the Epidural Space
1 Anatomy and Clinical Importance of the Epidural Space Sotonye Fyneface-Ogan Department of Anaesthesiology, Faculty of Clinical Sciences, College of Health Sciences, University of Port Harcourt, Nigeria 1. Introduction The epidural space is one of the most explored spaces of the human body. This exploration demands a good knowledge of the relevant anatomy and contents of the space. First described in 1901 (Corning JL, 1901), the epidural space is an anatomic compartment between the dural sheath and the spinal canal. In some areas it is a real space and in others only a potential space. Various methods have been used to study the anatomy of the epidural space by investigators. Methods such as epiduroscopy in cadavers and patients, anatomical dissection, Magnetic Resonance Imaging (MRI), Computerized Tomographic epidurography (Yan et al., 2010), epidural injections of resins and the use of cryomicrotome sectioning in cadavers frozen soon after death (Hogan QH, 1991), have been used to demonstrate the inner layout of the space. The use of the term ‘space’ has been controversial amongst anatomists. It is argued that the term would be more appropriate for the subarachnoid space than the epidural. It is claimed that the epidural space is not an open anatomical space whether in life or death. The only time a space is present is when the dura mater is artificially separated from the overlying vertebral canal by injection of contrast media or solutions of local anesthetics (Parkin & Harrison, 1985). 2. Embryology of the epidural space Histological transverse sections of human lumbar spines of adults and fetuses aged 13, 15, 21, 32 and 39 weeks (menstrual age) were studied (Hamid et al., 2002). -

FUNCTIONAL HUMAN ANATOMY LAB #3 Brain, Spinal Cord and Cranial Nerves
Lab 3 FUNCTIONAL HUMAN ANATOMY LAB #3 Brain, Spinal Cord and Cranial Nerves BRAIN: Frontal lobes Temporal lobes Correspond to the flat bones of the skull that cover the parts of the Parietal lobes cerebrum Occipital lobes Cerebellum Pons Medulla Oblongata (typically where the brain is severed during dissection) Corpus Callosum (where the cerebral hemispheres join; can be seen within the longitudinal cerebral fissure) Meninges and spaces: (superficial to deep - can be seen in both the brain and spinal cord) Epidural space (potential space in the cranium; actual space in the vertebral canal) Dura matter (very thick, easily palpable, opaque) Sub-dural space Arachnoid matter (very thin, transparent, easier to probe in the brain) Sub-arachnoid space (contains CSF fluid and much vasculature) Pia matter (non-dissectable) 12 CRANIAL NERVES: (know general innervations/functions) (CN I) Olfactory Sensory only - smell; courses on the inferior side of the frontal lobes and parallel to the cribriform plate; nerves go through the perforations in the plate to access the nasal cavity (CN II) Optic Sensory only - vision; processes light information and turns it into a picture that your brain can recognize (CN III) Oculomotor Motor and sensory function for the eyes; motor to all muscles except superior oblique m. and lateral rectus m.; controls ciliary muscle (lens) and sphincter muscle (iris); sensory - proprioception (CN IV) Trochlear Motor and sensory function for the eyes; motor to superior oblique muscle; sensory - proprioception (CN VI) Abducens -
Unit 11 Cranial Nerves, Spinal Cord, and Reflexes
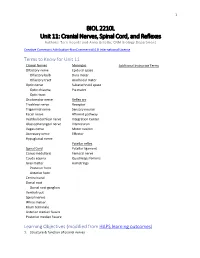
1 BIOL 2210L Unit 11: Cranial Nerves, Spinal Cord, and Reflexes Authors: Terri Koontz and Anna Gilletly, CNM Biology Department Creative Commons Attribution-NonCommercial 4.0 International License Terms to Know for Unit 11 Cranial Nerves Meninges Additional Instructor Terms Olfactory nerve Epidural space Olfactory bulb Dura mater Olfactory tract Arachnoid mater Optic nerve Subarachnoid space Optic chiasma Pia mater Optic tract Oculomotor nerve Reflex arc Trochlear nerve Receptor Trigeminal nerve Sensory neuron Facial nerve Afferent pathway Vestibulocochlear nerve Integration Center Glossopharyngeal nerve Interneuron Vagus nerve Motor neuron Accessory nerve Effector Hypoglossal nerve Patellar reflex Spinal Cord Patellar ligament Conus medullaris Femoral nerve Cauda equina Quadriceps femoris Gray matter Hamstrings Posterior horn Anterior horn Central canal Dorsal root Dorsal root ganglion Ventral root Spinal nerves White matter Filum terminale Anterior median fissure Posterior median fissure Learning Objectives (modified from HAPS learning outcomes) 1. Structure & function of cranial nerves 2 a. List and identify the cranial nerves by name and number. b. Describe the specific functions of each of the cranial nerves and classify each as sensory, motor or mixed. c. Identify the foramina that the cranial nerves pass through within the skull. 2. Anatomy of the spinal cord a. Describe the gross anatomy of the spinal cord. b. Identify the anatomical features seen in a cross sectional view of the spinal cord c. Identify the dorsal root ganglia, dorsal and ventral roots, and spinal nerves. 3. Reflexes & their roles in nervous system function a. Define the term reflex. b. Describe reflex responses in terms of the major structural and functional components of a reflex arc. -

Powerpoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck
PowerPoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck Slide Title Slide Number Slide Title Slide Number Arterial Blood Supply to the Head: Aortic Arch Branches Slide 2 Innervation of Dura Slide 14 Arterial Blood Supply to the Head: Carotid Arteries Slide 3 Emissary Veins & Diploic Veins Slide 15 Arterial Blood Supply to the Head: Internal Carotid Artery Slide4 Cerebral & Cerebellar Veins Slide 16 Blood Supply Review from MSI: Subclavian Artery & Named Dural Folds Slide 5 Slide 17 Thyrocervical Trunk Dural Venous Sinuses Slide 18 Vertebral Artery Slide 6 Dural Venous Sinuses (Continued) Slide 19 Subclavian Steal Syndrome Slide 7 Osseous Grooves formed by Dural Sinuses Slide 20 Thyrocervical Trunk Slide 8 Venous Drainage of Head: Cavernous Sinuses Slide 21 Review: Suprascapular Artery Slide 9 Head & Neck Venous Drainage Slide 22 Review: Transverse Cervical Artery Slide 10 Intracranial Versus EXtracranial Venous Drainage Slide 23 Middle Meningeal Artery Slide 11 Meningeal Layers & Spaces Slide 12 Cranial Dura, Dural Folds, & Dural Venous Sinuses Slide 13 Arterial Blood Supply to the Head: Aortic Arch Branches The head and neck receive their blood supply from https://3d4medic.al/PXGmbxEt branches of the right and left common carotid and right and left subclavian arteries. • On the right side, the subclavian and common carotid arteries arise from the brachiocephalic trunk. • On the left side, these two arteries originate from the arch of the aorta. Arterial Blood Supply to the Head: Carotid Arteries On each side of the neck, the common carotid arteries ascend in the neck to the upper border of the thyroid cartilage (vertebral level C3/C4) where they divide into eXternal and internal carotid arteries at the carotid bifurcation. -

Lab Exercise 9
Lab Exercise 9 Nervous Tissue Brain Cranial Nerves Spinal Cord Spinal Nerves Textbook Reference: See Chapter 11 for histology of nerve tissue and spinal cord See Chapter 12 for brain and spinal cord anatomy See Chapter 13 for cranial nerves and spinal nerves What you need to be able to do on the exam after completing this lab exercise: Be able to identify nerve tissue and identifying features, such as nerve cell body, nuclelus, nucleolus, processes, supporting cell nuclei, etc. Be able to identify the listed parts of the brain on the brain models. Be able to identify the listed parts of the brain on the sheep brains. Be able to identify the cranial nerves by name, Roman numeral, and function on the brain and brainstem models. Be able to identify the listed parts of the spinal cord on the spinal cord models. Be able to identify the listed parts of the spinal cord on the spinal cord microscope slides. Be able to identify the listed plexuses and major spinal nerves on the nerve man model. For a handy supplemental study guide, please print the “Nervous System Handout” under “Virtual Lab Nine” on the Virtual Lab website. 9-1 Nervous Tissue Nervous tissue is composed of two major cell types: supporting cells and neurons. Supporting cells are non-conducting cells that far outnumber the neurons and function to protect, support, and insulate the neurons. Neurons are the large conducting cells of nervous tissue. They all have a nucleus-containing cell body, and their cytoplasm is drawn out into long extensions (processes).