Primary UREC Derived from Control Individuals
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Identification of Regulation in Central Carbon Metabolism Among Related
Identification of differential regulation in central carbon metabolism between related cell lines DISSERTATION zur Erlangung des akademischen Grades Doctor rerum naturalium (Dr. rer. nat.) im Fach Biophysik eingereicht an der Lebenswissenschaftlichen Fakultät der Humboldt-Universität zu Berlin von M.Sc. Roman Josef Rainer Präsidentin/Präsident der Humboldt-Universität zu Berlin: Prof. Dr.-Ing. Dr. Sabine Kunst Dekanin/Dekan der Lebenswissenschaftlichen Fakultät der Humboldt-Universität zu Berlin: Prof. Dr. Bernhard Grimm Gutachter/innen: 1. Prof. Dr. Dr. h.c. Edda Klipp 2. Prof. Dr. Birgit Sawitzki 3. Prof. Julio R. Banga Tag der mündlichen Prüfung: 29.10.2020 Abstract Colon cancer cells and T cells regulate central carbon metabolism to meet their anabolic needs. In KRAS and BRAF tumors, metabolic reprogramming is a premise to support rapid prolif- eration. In T cells, the mitochondrial T cell activation inhibitor (TCAIM) is known to affect mitochondrial morphology but its effect on cellular metabolism is not well understood. Via math- ematical modelling, I investigate the differential regulation of closely related cell lines. I present the first mathematical model for colon cancer and T cell metabolism, unraveling differential regulation between related cell lines. The model shows that CaCO2-BRAFV600Ecells are mostly downregulated compared to CaCO2-KRASG12Vand CaCO2-control. Additionally, it demon- strates the critical role of monocarboxylate transporter (MCT), especially for CaCO2-KRASG12V. Concerning T cells, I compare wild-type T cells to homozygous TCAIM T cells. This unveils that TCAIM homozygous cells have a mostly downregulated TCA cycle, validated by RNASeq data, and are less metabolically active than wild-type T cells. Furthermore, if the glycolytic flux is not sufficient to support lactate export and biomass production, the model reveals that the TCA cy- cle is reversed as it requires less regulation. -

Inherited Monogenic Defects of Ceramide Metabolism Molecular
Clinica Chimica Acta 495 (2019) 457–466 Contents lists available at ScienceDirect Clinica Chimica Acta journal homepage: www.elsevier.com/locate/cca Review Inherited monogenic defects of ceramide metabolism: Molecular bases and diagnoses T ⁎⁎ Patricia Dubota,b, Frédérique Sabourdya,b, Jitka Rybovac,Jeffrey A. Medinc,d, , ⁎ Thierry Levadea,b, a Laboratoire de Biochimie Métabolique, Centre de Référence en Maladies Héréditaires du Métabolisme, Institut Fédératif de Biologie, CHU de Toulouse, Toulouse, France b INSERM UMR1037, CRCT (Cancer Research Center of Toulouse), Université Paul Sabatier, Toulouse, France c Department of Pediatrics, Medical College of Wisconsin, Milwaukee, WI, USA d Department of Biochemistry, Medical College of Wisconsin, Milwaukee, WI, USA ABSTRACT Ceramides are membrane lipids implicated in the regulation of numerous biological functions. Recent evidence suggests that specific subsets of molecular species of ceramide may play distinct physiological roles. The importance of this family of molecules in vertebrates is witnessed by the deleterious consequences of genetic alterations in ceramide metabolism. This brief review summarizes the clinical presentation of human disorders due to the deficiency of enzymes involved either in the biosynthesis or the degradation of ceramides. Information on the possible underlying pathophysiological mechanisms is also provided, based on knowledge gathered from animal models of these inherited rare conditions. When appropriate, tools for chemical and molecular diagnosis of these disorders and therapeutic options are also presented. 1. Introduction/foreword relationships that are relevant for unraveling the biological role of these genes and gene products in humans. Studies on ceramides and sphingolipid metabolism have attracted a lot of attention recently. This is largely related to the multiplicity of 2. -

Enhancing Skin Health: by Oral Administration of Natural Compounds and Minerals with Implications to the Dermal Microbiome
Review Enhancing Skin Health: By Oral Administration of Natural Compounds and Minerals with Implications to the Dermal Microbiome David L. Vollmer 1, Virginia A. West 1 and Edwin D. Lephart 2,* 1 4Life Research, Scientific Research Division, Sandy, Utah 84070, USA; [email protected] (D.L.V.); [email protected] (V.A.W) 2 Department of Physiology, Developmental Biology and The Neuroscience Center, Brigham Young University, Provo, Utah 84602, USA * Correspondence: [email protected]; Tel.: +1-801-422-2006 Received: 23 August 2018; Accepted: 1 October 2018; Published: 7 October 2018 Abstract: The history of cosmetics goes back to early Egyptian times for hygiene and health benefits while the history of topical applications that provide a medicinal treatment to combat dermal aging is relatively new. For example, the term cosmeceutical was first coined by Albert Kligman in 1984 to describe topical products that afford both cosmetic and therapeutic benefits. However, beauty comes from the inside. Therefore, for some time scientists have considered how nutrition reflects healthy skin and the aging process. The more recent link between nutrition and skin aging began in earnest around the year 2000 with the demonstrated increase in peer-reviewed scientific journal reports on this topic that included biochemical and molecular mechanisms of action. Thus, the application of: (a) topical administration from outside into the skin and (b) inside by oral consumption of nutritionals to the outer skin layers is now common place and many journal reports exhibit significant improvement for both on a variety of dermal parameters. Therefore, this review covers, where applicable, the history, chemical structure, and sources such as biological and biomedical properties in the skin along with animal and clinical data on the oral applications of: (a) collagen, (b) ceramide, (c) β-carotene, (d) astaxanthin, (e) coenzyme Q10, (f) colostrum, (g) zinc, and (h) selenium in their mode of action or function in improving dermal health by various quantified endpoints. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
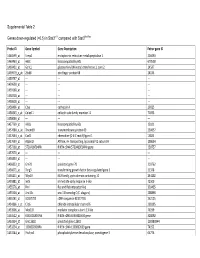
0.5) in Stat3∆/∆ Compared with Stat3flox/Flox
Supplemental Table 2 Genes down-regulated (<0.5) in Stat3∆/∆ compared with Stat3flox/flox Probe ID Gene Symbol Gene Description Entrez gene ID 1460599_at Ermp1 endoplasmic reticulum metallopeptidase 1 226090 1460463_at H60c histocompatibility 60c 670558 1460431_at Gcnt1 glucosaminyl (N-acetyl) transferase 1, core 2 14537 1459979_x_at Zfp68 zinc finger protein 68 24135 1459747_at --- --- --- 1459608_at --- --- --- 1459168_at --- --- --- 1458718_at --- --- --- 1458618_at --- --- --- 1458466_at Ctsa cathepsin A 19025 1458345_s_at Colec11 collectin sub-family member 11 71693 1458046_at --- --- --- 1457769_at H60a histocompatibility 60a 15101 1457680_a_at Tmem69 transmembrane protein 69 230657 1457644_s_at Cxcl1 chemokine (C-X-C motif) ligand 1 14825 1457639_at Atp6v1h ATPase, H+ transporting, lysosomal V1 subunit H 108664 1457260_at 5730409E04Rik RIKEN cDNA 5730409E04Rik gene 230757 1457070_at --- --- --- 1456893_at --- --- --- 1456823_at Gm70 predicted gene 70 210762 1456671_at Tbrg3 transforming growth factor beta regulated gene 3 21378 1456211_at Nlrp10 NLR family, pyrin domain containing 10 244202 1455881_at Ier5l immediate early response 5-like 72500 1455576_at Rinl Ras and Rab interactor-like 320435 1455304_at Unc13c unc-13 homolog C (C. elegans) 208898 1455241_at BC037703 cDNA sequence BC037703 242125 1454866_s_at Clic6 chloride intracellular channel 6 209195 1453906_at Med13l mediator complex subunit 13-like 76199 1453522_at 6530401N04Rik RIKEN cDNA 6530401N04 gene 328092 1453354_at Gm11602 predicted gene 11602 100380944 1453234_at -

Supplemental Materials Supplemental Table 1
Electronic Supplementary Material (ESI) for RSC Advances. This journal is © The Royal Society of Chemistry 2016 Supplemental Materials Supplemental Table 1. The differentially expressed proteins from rat pancreas identified by proteomics (SAP vs. SO) No. Protein name Gene name ratio P value 1 Metallothionein Mt1m 3.35 6.34E-07 2 Neutrophil antibiotic peptide NP-2 Defa 3.3 8.39E-07 3 Ilf2 protein Ilf2 3.18 1.75E-06 4 Numb isoform o/o rCG 3.12 2.73E-06 5 Lysozyme Lyz2 3.01 5.63E-06 6 Glucagon Gcg 2.89 1.17E-05 7 Serine protease HTRA1 Htra1 2.75 2.97E-05 8 Alpha 2 macroglobulin cardiac isoform (Fragment) 2.75 2.97E-05 9 Myosin IF (Predicted) Myo1f 2.65 5.53E-05 10 Neuroendocrine secretory protein 55 Gnas 2.61 7.60E-05 11 Matrix metallopeptidase 8 Mmp8 2.57 9.47E-05 12 Protein Tnks1bp1 Tnks1bp1 2.53 1.22E-04 13 Alpha-parvin Parva 2.47 1.78E-04 14 C4b-binding protein alpha chain C4bpa 2.42 2.53E-04 15 Protein KTI12 homolog Kti12 2.41 2.74E-04 16 Protein Rab11fip5 Rab11fip5 2.41 2.84E-04 17 Protein Mcpt1l3 Mcpt1l3 2.33 4.43E-04 18 Phospholipase B-like 1 Plbd1 2.33 4.76E-04 Aldehyde dehydrogenase (NAD), cytosolic 19 2.32 4.93E-04 (Fragments) 20 Protein Dpy19l2 Dpy19l2 2.3 5.68E-04 21 Regenerating islet-derived 3 alpha, isoform CRA_a Reg3a 2.27 6.74E-04 22 60S acidic ribosomal protein P1 Rplp1 2.26 7.22E-04 23 Serum albumin Alb 2.25 7.98E-04 24 Ribonuclease 4 Rnase4 2.24 8.25E-04 25 Cct-5 protein (Fragment) Cct5 2.24 8.52E-04 26 Protein S100-A9 S100a9 2.22 9.71E-04 27 Creatine kinase M-type Ckm 2.21 1.00E-03 28 Protein Larp4b Larp4b 2.18 1.25E-03 -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

The Metabolic Serine Hydrolases and Their Functions in Mammalian Physiology and Disease Jonathan Z
REVIEW pubs.acs.org/CR The Metabolic Serine Hydrolases and Their Functions in Mammalian Physiology and Disease Jonathan Z. Long* and Benjamin F. Cravatt* The Skaggs Institute for Chemical Biology and Department of Chemical Physiology, The Scripps Research Institute, 10550 North Torrey Pines Road, La Jolla, California 92037, United States CONTENTS 2.4. Other Phospholipases 6034 1. Introduction 6023 2.4.1. LIPG (Endothelial Lipase) 6034 2. Small-Molecule Hydrolases 6023 2.4.2. PLA1A (Phosphatidylserine-Specific 2.1. Intracellular Neutral Lipases 6023 PLA1) 6035 2.1.1. LIPE (Hormone-Sensitive Lipase) 6024 2.4.3. LIPH and LIPI (Phosphatidic Acid-Specific 2.1.2. PNPLA2 (Adipose Triglyceride Lipase) 6024 PLA1R and β) 6035 2.1.3. MGLL (Monoacylglycerol Lipase) 6025 2.4.4. PLB1 (Phospholipase B) 6035 2.1.4. DAGLA and DAGLB (Diacylglycerol Lipase 2.4.5. DDHD1 and DDHD2 (DDHD Domain R and β) 6026 Containing 1 and 2) 6035 2.1.5. CES3 (Carboxylesterase 3) 6026 2.4.6. ABHD4 (Alpha/Beta Hydrolase Domain 2.1.6. AADACL1 (Arylacetamide Deacetylase-like 1) 6026 Containing 4) 6036 2.1.7. ABHD6 (Alpha/Beta Hydrolase Domain 2.5. Small-Molecule Amidases 6036 Containing 6) 6027 2.5.1. FAAH and FAAH2 (Fatty Acid Amide 2.1.8. ABHD12 (Alpha/Beta Hydrolase Domain Hydrolase and FAAH2) 6036 Containing 12) 6027 2.5.2. AFMID (Arylformamidase) 6037 2.2. Extracellular Neutral Lipases 6027 2.6. Acyl-CoA Hydrolases 6037 2.2.1. PNLIP (Pancreatic Lipase) 6028 2.6.1. FASN (Fatty Acid Synthase) 6037 2.2.2. PNLIPRP1 and PNLIPR2 (Pancreatic 2.6.2. -

Beta Version
Beta Version Zentrum für Infektionsforschung Research Centre for Infectious Diseases Wissenschaftlicher Bericht Josef-Schneider-Str. 2/D15 Scientific Report 2014–2015 97080 Würzburg Germany T +49-931-3182575 F +49-931-3182578 zentrum für M [email protected] infektionsforschung research centre for infectious diseases research centre for infectious diseases 2014–2015 zentrum für infektionsforschung – scientific report 2014-2015 content 1. general remarks 3.6 Department of Internal Medicine II 98 3.6.1 Hermann Einsele – Interaction of Immune Effector Cells with Aspergillus fumigatus 100 1.1 Speaker‘s Report 2014 – 2015 / Sprecherbericht für den Zeitraum 2014 – 2015 6 3.6.2 Andreas Beilhack – Experimental Stem Cell Transplantation 102 1.2 Directory of People Associated with the ZINF 12 3.6.3 Hartwig Klinker – Division of Infectious Diseases 104 1.3 Structure of the ZINF 18 3.6.4 Jürgen Löffl er – Immunity against Aspergillus spp. 106 1.4 News from the ZINF 20 3.6.5 Andrew Ullmann – Clinical Infectious Diseases 108 2. young investigator groups of the zinf 4. zinf members associated with other institutes 2.1 Cynthia Sharma (ZINF) – Deep Sequencing Approaches to Pathogenesis 28 4.1 Gerhard Bringmann – Natural Products Chemistry 112 2.2 Daniel Lopez (ZINF) – Cell-Cell Communication and Signal Transduction 30 4.2 Thomas Dandekar – Bioinformatics 114 2.3 Nicolai Siegel (ZINF) – Trypanosoma Gene Regulation 32 4.3 Markus Engstler – Molecular and Physical Parasitology 116 2.4 Ana Eulalio (BioSysNet) – Host RNA Metabolism 34 4.4 Ute Hentschel-Humeida – Marine Sponge-Microbe Interactions 118 2.5 Christian Perez (IZKF) – Regulatory Networks in Pathogenesis 36 4.5 Ulrike Holzgrabe – Medicinal Chemistry 120 2.6 Sebastian Geibel (Elite Network Bavaria) – Structural Biology of Mycobacteria 38 4.6 Caroline Kisker – Structure Based Drug Design 122 2.7 Sina Bartfeld (ZINF) – Organoids as Host Model 40 4.7 Gabriela Krasteva-Christ – Pulmonary Neurobiology 124 4.8 August Stich – Tropical Medicine 126 4.9 Heike Walles – Tissue Engineering 128 3. -

Protein Network Analyses of Pulmonary Endothelial Cells In
www.nature.com/scientificreports OPEN Protein network analyses of pulmonary endothelial cells in chronic thromboembolic pulmonary hypertension Sarath Babu Nukala1,8,9*, Olga Tura‑Ceide3,4,5,9, Giancarlo Aldini1, Valérie F. E. D. Smolders2,3, Isabel Blanco3,4, Victor I. Peinado3,4, Manuel Castell6, Joan Albert Barber3,4, Alessandra Altomare1, Giovanna Baron1, Marina Carini1, Marta Cascante2,7,9 & Alfonsina D’Amato1,9* Chronic thromboembolic pulmonary hypertension (CTEPH) is a vascular disease characterized by the presence of organized thromboembolic material in pulmonary arteries leading to increased vascular resistance, heart failure and death. Dysfunction of endothelial cells is involved in CTEPH. The present study describes for the frst time the molecular processes underlying endothelial dysfunction in the development of the CTEPH. The advanced analytical approach and the protein network analyses of patient derived CTEPH endothelial cells allowed the quantitation of 3258 proteins. The 673 diferentially regulated proteins were associated with functional and disease protein network modules. The protein network analyses resulted in the characterization of dysregulated pathways associated with endothelial dysfunction, such as mitochondrial dysfunction, oxidative phosphorylation, sirtuin signaling, infammatory response, oxidative stress and fatty acid metabolism related pathways. In addition, the quantifcation of advanced oxidation protein products, total protein carbonyl content, and intracellular reactive oxygen species resulted increased -

Human Induced Pluripotent Stem Cell–Derived Podocytes Mature Into Vascularized Glomeruli Upon Experimental Transplantation
BASIC RESEARCH www.jasn.org Human Induced Pluripotent Stem Cell–Derived Podocytes Mature into Vascularized Glomeruli upon Experimental Transplantation † Sazia Sharmin,* Atsuhiro Taguchi,* Yusuke Kaku,* Yasuhiro Yoshimura,* Tomoko Ohmori,* ‡ † ‡ Tetsushi Sakuma, Masashi Mukoyama, Takashi Yamamoto, Hidetake Kurihara,§ and | Ryuichi Nishinakamura* *Department of Kidney Development, Institute of Molecular Embryology and Genetics, and †Department of Nephrology, Faculty of Life Sciences, Kumamoto University, Kumamoto, Japan; ‡Department of Mathematical and Life Sciences, Graduate School of Science, Hiroshima University, Hiroshima, Japan; §Division of Anatomy, Juntendo University School of Medicine, Tokyo, Japan; and |Japan Science and Technology Agency, CREST, Kumamoto, Japan ABSTRACT Glomerular podocytes express proteins, such as nephrin, that constitute the slit diaphragm, thereby contributing to the filtration process in the kidney. Glomerular development has been analyzed mainly in mice, whereas analysis of human kidney development has been minimal because of limited access to embryonic kidneys. We previously reported the induction of three-dimensional primordial glomeruli from human induced pluripotent stem (iPS) cells. Here, using transcription activator–like effector nuclease-mediated homologous recombination, we generated human iPS cell lines that express green fluorescent protein (GFP) in the NPHS1 locus, which encodes nephrin, and we show that GFP expression facilitated accurate visualization of nephrin-positive podocyte formation in -

Epistatic Interactions Associated with Fatty Acid
FACULDADE DE CIÊNCIAS AGRÁRIAS E VETERINÁRIAS UNIVERSIDADE ESTADUAL PAULISTA CÂMPUS DE JABOTICABAL EPISTATIC INTERACTIONS ASSOCIATED WITH FATTY ACID PROFILE OF BEEF FROM NELLORE CATTLE Sabrina Thaise Amorim Zootecnista 2020 FACULDADE DE CIÊNCIAS AGRÁRIAS E VETERINÁRIAS UNIVERSIDADE ESTADUAL PAULISTA CÂMPUS DE JABOTICABAL EPISTATIC INTERACTIONS ASSOCIATED WITH FATTY ACID PROFILE OF BEEF FROM NELLORE CATTLE Sabrina Thaise Amorim Orientador: Prof. Dr. Fernando Sebastián Baldi Rey Co-orientador: Dr. Fernando Brito Lopes Co-orientadora: Dra. Nedenia Bonvino Stafuzza Dissertação apresentada à Faculdade de Ciências Agrárias e Veterinárias – Unesp, Campus de Jaboticabal, como parte das exigências para a obtenção do título de Mestre em Genética e Melhoramento Animal. 2020 Amorim, Sabrina Thaise A524e Epistatic interactions associated with fatty acid profile of beef from Nellore cattle / Sabrina Thaise Amorim. -- Jaboticabal, 2020 173 p. Dissertação (mestrado) - Universidade Estadual Paulista (Unesp), Faculdade de Ciências Agrárias e Veterinárias, Jaboticabal Orientador: Fernando Sebastián Baldi Rey Coorientador: Fernando Brito Lopes 1. Genética. 2. Melhoramento Animal. 3. Genômica. I. Título. Sistema de geração automática de fichas catalográficas da Unesp. Biblioteca da Faculdade de Ciências Agrárias e Veterinárias, Jaboticabal. Dados fornecidos pelo autor(a). Essa ficha não pode ser modificada. DADOS CURRICULARES DO AUTOR Sabrina Thaise Amorim, nascida em 02 de julho de 1995 na cidade de Brusque – Santa Catarina, filha de Alexandre Adriano Amorim e Liliane RaQuel Pavesi Amorim. Iniciou em março de 2013 o curso de graduação em Zootecnia na Universidade Federal de Santa Catarina, obtendo o título de Zootecnista em dezembro de 2017. Durante a graduação foi bolsista de Iniciação Científica do CNPq, monitora da disciplina “Genética Aplicada à Zootecnia”, integrante do Grupo de Pesquisa em Produção Animal e integrante do Laboratório de Pesquisa e Ensino em Genética Animal (LEPGA) da mesma instituição de fomento, sob a orientação do Prof.